Traumatic Globe Luxation
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Globe luxation is a rare condition that can present spontaneously or more commonly following trauma, where there is complete or partial prolapse of the globe from the orbit. Varying degrees of globe prolapse may be encountered in clinical practice with variable clinical, functional, structural and aesthetic outcomes.[1][2][3] Severe cases may be associated with associated orbital soft tissue and bone injuries with variable lengths of the optic nerve and thus variable location of the optic nerve being severed. Likewise variable severity of extra ocular muscle disruption may also be encountered
Classification
Globe injuries traditionally have been classified into closed globe injuries(CGI), open globe injuries(OGI). A third form may be varying degrees of globe luxations and globe avulsions (GA).
Several classifications may be employed in relation to globe luxation. It may be partial or incomplete (prolapse of the globe alone with a structurally intact optic nerve and extraocular muscles) or complete (prolapse along with severed optic nerve and extraocular muscles).[1][2][4] An uncommon form of complete globe avulsion is the Long Segment Optic Nerve avulsion which is often associated with autoenucleations.
Globe avulsions may also be classified in to luxation alone (with or without partial avulsion), dislocation( globe prolapse into the paranasal sinuses or intracranial cavity) or complete avulsion.[5][6][7]
Etiology
Based on the etiology, globe luxation can be classified as spontaneous, voluntary and post-traumatic. Spontaneous luxation may occur without conscious effort, with or without predisposing factors. Typically this includes shallow orbits, lax orbital soft tissue and adnexal structures. Voluntary globe luxation is the ability to protrude the globe by the patient, most often by simple conscious eyelid manipulation. Traumatic luxation occurs following high velocity direct or indirect trauma especially to the head and neck region. Trauma seems to be the most common etiology for the luxation of the globe, the spectrum of which include road traffic accidents, surfboard injury and from other forms of extreme sports, human and animal bites, domestic blunt or penetrating injury and finally self-inflicted injuries. Road traffic accidents appear to be the common cause.[4][8][9][10][11] Apart from accidental injuries, traumatic enucleation and various degrees of globe avulsion may be encountered in psychiatric disorders - self or other, with cultural, religious and other factors in play (https://en.wikipedia.org/wiki/Kannappa).
There are also 56 reported cases (71 globes) of self enucleation/auto enucleation (Oedipism Rex https://en.wikipedia.org/wiki/Oedipus_Rex)[12] since 1933-2015 with a significant proportion either from underlying mental illness (mostly schizophrenia), religious influences, dementia and those under influence of recreational drugs.[13][14][15][16]
Gouging was a brutal fight in which a combatant was successful if he would press the adversary’s eyeball out with his thumb by sudden severe torsion on the globe. This was a common cause of globe luxation many years ago especially in the west prior to the invention of revolvers for duels. Surprisingly no serious or permanent damage has been reported lately.[17] Accidental gouging has also been reported in obstructed labour as a problem due to faulty application of forceps during delivery. [18]
In general, globe luxation can occur spontaneously, more commonly following trauma, or can be associated with other systemic diseases like thyroid eye disease, shallow orbits (Crouzon syndrome, Apart syndrome, etc), chronic obstructive pulmonary diseases, floppy eye lid syndrome or lax extraocular muscles.[19][20][21] Mechanical maneuvers like Valsava, eyelid manipulation, general anesthesia, contact lens insertion and removal and trauma have also has been reported as the cause of globe luxation.[20][22]
Epidemiology
Traumatic luxation of the globe is a rare condition with only 109 cases reported until 2021.[9] Amaral et al reported that it is more common in males 4.7:1 with a mean age of 29.5 years (5 - 74 years).[23][24] Traumatic globe luxation into the paranasal sinuses is even more rare and until 2016 there were only 24 cases reported with male female ratio of 6:1, 42% of which were caused by traffic accidents. The maxillary sinus is the most common involved (87.5%) following with ethmoidal sinus (12.5%). [24][25]
Pathophysiology

Morris et al had proposed three hypotheses for globe luxation. The first is an elongated object entering the medial orbit may act as a fulcrum propelling the globe forward. The second is a wedge-shaped object entering the orbit medially and displacing the globe anteriorly. The third is a direct transection of the optic nerve by a penetrating sharp object.[27]
Isolated anterior luxation of the globe alone, without optic nerve or extraocular muscle avulsion, occurs when a blunt object is insinuated in the superomedial orbit, between the globe and the superomedial orbit. This not only induces a globe prolapse but is also followed by a secondary severe reflex spasm of the orbicularis oculi locking the globe in place. While the eyelids normally play an important role in preventing globe prolapse, blunt or sharp objects encountered in daily life such as bike handles, gift wrapping tubes, door handles, fences, etc may induce a globe prolapse from secondary raised intraorbital pressure whilst pushing the upper eyelid backwards.[3][28][29][30][26][31]
A second mechanism is the coup-contre coup injury, commonly associated with craniofacial trauma. A resultant orbital haemorrhage may precipitate rapid anterior movement of the globe(s).
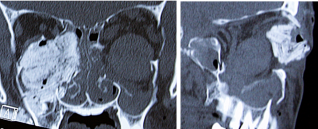
A third mechanism is direct result of sudden reduction of the orbital cavity volume such as following large blow-in fractures, typically of the orbital roof.[3][32] Paradoxically, large displaced orbital wall blow out fractures may precipitate a globe prolapse into one of the paranasal sinuses – most commonly the maxillary sinus and less commonly the ethmoidal sinus and even more rarely the intracranial cavity.[3][25][33][34][35]
An avulsion of the optic nerve and/or extraocular muscle(s) following the globe luxation may be from sharp objects, or a bony fragment that may transect that the optic nerve, aggravated by extreme forward displacement of the globe. The latter movement may cause a complete disruption of optic nerve fibers at the lamina cribrosa, which lack a myelin sheath. Extraocular muscle involvement is also common following severe maxillofacial trauma e.g Le Fort II or III fractures, with almost 90% of midfacial fractures associated with ocular trauma presenting with significant proptosis or some degree of globe luxation.[4][36]

Diagnosis
Clinical Features

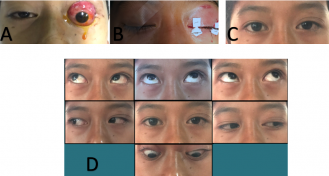
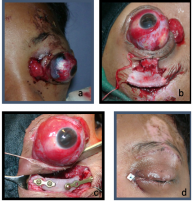
Presenting clinical symptoms may vary from a completely asymptomatic patient (underlying psychiatric conditions – ‘la belle indifference’) to one with severe pain and visual loss. Acute presentation include a restless patient with profuse bleeding, periorbital ecchymosis, apparent proptosis with immobile globe with secondary blepharospasm. Rarely, the cut end of the optic nerve may also be visualized.[38]
Apart from visual loss persistent globe luxation can also lead to other complications such as corneal abrasion, exposure keratopathy, secondary blepharospasm and pthisis bulbi in late stages from ocular ischemia and/or corneal perforation. Life threatening complications such as meningitis, intracranial hemorrhage and cerebrospinal fluid leakage have also been reported.[4] In auto-enucleation cases, the injury and complications may be more severe and even life threatening. These include visual field defects not only in the ipsilateral eye but also contralateral eye from chiasmal damage causing temporal field defect and also neurovascular sequale such as subarachnoid hemorrhage.[16][38][37][39]
Loss of extraocular muscle(s)’ is reported when one or more muscles are avulsed or transected. The most common muscle involved is the medial rectus followed by the inferior rectus, superior rectus, lateral rectus and oblique muscles respectively in that order.[4][36][40]
In typical globe luxation, the globe is visualized outside the orbit but in rare situations, the patient may present with an ‘empty socket’. In such situations, the globe may be prolapsed into one of the paranasal sinuses (maxillary sinus followed by the ethmoid sinus).[1][35][27][41] Displacement of the globe into paranasal sinus can be easily explained by large displaced blow out fractures. Careful examination should be performed when the trauma involves the ethmoid sinus due to the proximity of the skull base with potential CSF leak (‘liquor fistula’).[42] Even more rarely, globe luxation into the into the anterior cranial fossa may occur following by extensive and displaced frontal fracture of orbital roof, with a combination of high intraorbital pressure and dehiscence of the orbital roof as causative factors.[7][43][44]
Management
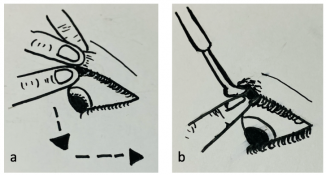
Management of the globe luxation is an ophthalmic and medical emergency, as most cases end up with poor visual prognosis despite best and early management. There are two established maneuvers that have been described to repositioned the luxated eye ball. Both require some form of cooperation by the patient and if possible, with some sedation and/or anesthesia along with an orbicularis or facial nerve block. The first maneuver is performed while asking the patient to look down. The upper eyelid is gently and firmly pulled upward while the globe is simultaneously depressed with the index finger of the other hand to repositioning the globe. The second method is using Desmarres retractor which is introduced between the upper lid and the globe. Once the tip is under the eyelid, digital manipulation is performed to depress and reposition the globe into the orbit.[45][46]
In cases where there is associated optic nerve or extraocular muscle damage, globe restoration must be performed as early as possible to restore full structural and hopefully functional recovery of the globe. Secondary procedures that may be considered include performing a tarsorrhaphy, upper eyelid retraction repair, orbital fracture repair, and orbital decompression in severe cases.[4][32] High dose intravenous corticosteroid and neuroprotective agent may also be considered to reduce posttraumatic inflammation and edema albeit with limited evidence. Panje et all recommended 1 mg dexamethasone/kg body weight initially continue with 0,5 mg/kg every six hours for next 24 hour, and 1 mg/kg per day for one or two days for the optic nerve injury. After successful globe reduction, the patient should have immediate relief of pain and return of vision and extraocular muscle function if there is no optic nerve and extraocular muscle damage. Such functional recovery has been reported up to a week post luxation.[20][26][46][47][48]
Management for globe luxation into the paranasal sinus is similar to blow out fracture repairs but should be performed much more delicately with least induced iatrogenic trauma and undue delay.
There are two techniques to reposition the globe luxated into the paranasal sinuses. The first is direct traction on the globe with instrumental help. The second is manual repositioning of the globe via transmaxillary or transnasal approach.[5][25][33][49] In these cases, close collaboration with an endoscopic assisted craniomaxillofacial surgical technique is essential for good exposure with least trauma t to the vital orbital structures including the globe, the extraocular muscles and the optic nerve.[50] Orbital reconstruction may then be performed either with autologous bone or more commonly one of the alloplastic implants - titanium plates, porous poplyethylene or bioresorbable implants.[25][33][49]
| Timeline | Approach | Note |
|---|---|---|
| At Emergency Department | Global assessment, note emergency situation
a. life threatening b. vision threatening Ophthalmic assessment CT-scan Decide if the reposition of the globe can be done directly, if there is no optic nor extraocular muscle avulsion |
Head injury Retrobulbar haemorrhage, globe luxation Optic nerve avulsion Extraocular muscles avulsion Orbital fracture Give analgesic (iv, per oral, topical) Try to reposition the globe using manual eye repositioning |
| Intraoperative | Explore and reattach the extraocular muscle, tarsoraphy, upper eyelid retraction repair, orbital fracture repair, and orbital decompression in severe cases | High dose intravenous corticosteroid and neuroprotective agents may also be considered to reduce post-traumatic inflammation and edema |
In patients who present with autoenucleation, management should include psychiatric consultation, suicide precautions and securing family support. Rapid parenteral tranquilization is often needed as a prophylaxis against suicide and further self mutilation.[14][15][51]
The sequence of management thus is initial globe repositioning, followed by exploration and repair of avulsed extraocular muscles when present preferably as soon as possible. It should be remembered the longer the globe and orbital structures are prolapsed, the poorer the structural and thus functional and even esthetic prognosis owing to ocular ischemia, exposure keratopathy, extraocular muscle retraction within the orbit. Preservation of the globe even in patients with visual loss is important in the view of aesthetic and psychological considerations of the patient and family.[1][3][52][53]
In exceptional cases of either several and completely avulsed globe along with optic nerve and extraocular muscles or in patients presenting late with severe exposure , corneal perforation or phthisis, enucleation may be performed (5,9% ).[36][54] Enucleation therefore is the last option in managing this condition, and only should be done when the integrity of the globe can’t be repositioned and reinserted after all possible efforts, and also in such case of complete optic nerve and extra ocular muscle avulsion.[52][53] In such patients the socket should be rehabilitated either as a delayed primary procedure or secondarily with an orbital implant and customized prosthesis to restore normal appearance thus aiding psychological rehabilitation.
Summary
Globe luxation and avulsions are ophthalmic emergencies as they are severely vision threatening and sometimes bilateral. Early recognition and prompt management by repositioning the globe and trying to reattach the extraocular muscles may lead to possibility of globe salvage and possibly regaining visual recovery, with better cosmetic, physiological result, and improves psychological status of the patient.
Submitted in Recognition of and on behalf of the Asia Pacific Ophthalmic Trauma Society (APOTS)
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 Kiratli H, Tumer B, Bigic S. Management of traumatic luxation of the globe. Acta Ophthalmol Scand. 1999;77:340–2
- ↑ Jump up to: 2.0 2.1 Lang G, Bialasiewicz A, Rohr W. Beideseitige traumatische avulsio bulbi. Klin Mbl Augenheilk. 1991;198:112–6
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Gupta H, Natarajan S, Vaidya S, Gupta S, Shah D, Merchant R, et al. Traumatic eye ball luxation: A stepwise approach to globe salvage. Saudi J Opthalmology. 2017;31:260–5
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 Viji R, Yazhini T. Traumatic luxation of the globe: A novel simple treatment. J ophthalmic Sci Res. 2017;55(2):145–7
- ↑ Jump up to: 5.0 5.1 Noman SA, Mostafa Ibrahim Shindy. Immediate Surgical Management of traumatic dislocation of the eye globe into the maxillary sinus: Report of a rare case and literature review. Craniomaxillofac, trauma Reconstr. 2017;10:151–8
- ↑ Jellab B, Baha A, Moutaouakil A. Management of severe cranio-orbito-facial trauma with a dislocation of the globe into the maxillary sinus. Bull soc Belge Ophtalmol. 2008;37–41
- ↑ Jump up to: 7.0 7.1 Vahdati SS, Sadeghi H. Orbital roof fracture: Dislocation of globe into the anterior cranial fossa. JAEMCR. 2011;2(1):47–9
- ↑ Tok L, Tok O, Argun T, Yilmaz O, Gunes A, Unlu E, et al. Bilateral traumatic globe luxation with optic nerve transection. Case REp Ophthalmol. 2014;5(3):429–34
- ↑ Jump up to: 9.0 9.1 Roka N, Roka Y. Traumatic luxation of the eye ball with optic nerve transection following road traffic accident: report of two cases and brief review of literature. Nepal J Ophthalmol. 2018;10(20):196–202
- ↑ Hindman H, Shikumaran D, Halfpenny C, Hirschbein M. Traumatic globe luxation and enucleation caused by a human bite injury. Ophthalmic Plast Reconstr Surg. 2007;23(5):422–3
- ↑ Paya C, Delyfer M, Thoumazet F, Pechemeja J, BOCQUET J, Korobelnik J, et al. Traumatic optic nerve avulsion: A case report. J Fr Ophthalmol. 2012;35(5):360
- ↑ Oedipus Rex
- ↑ Jones N. Self Enucleation and psychosis. BR J Ophthalmol. 1990;74(9):571–3
- ↑ Jump up to: 14.0 14.1 FAN AH. Auto enucleation: A Case Report and Literature review. Psychiatry. 2007
- ↑ Jump up to: 15.0 15.1 Khan JA, Buescher L, Ide CH, Ben Pettigrove. Medical management of self enucleation. Arch Ophthalmol. 1985;103:386–9
- ↑ Jump up to: 16.0 16.1 Gauger EH, Souber RK, Richard C Allen. Complications and oucomes after autoenuclation. Curr Opin Ophthalmol. 2015;26:429–38
- ↑ Gould GM, Pyle WL. Anomalies and curiosities of medicine. New York. The Julian Press Inc. 1956; 527-528.
- ↑ Khanduja S, Aggarwal S, Solanki S, Khanduja N, Sachdeva S. ‘Globe Luxation’: A Dramatic Complication of Forceps Assisted Vaginal Delivery. Indian J Pediatrics. 2015 Aug;82(8):759–60.
- ↑ Pujari A, Bajaj M s, Regani H, Jayaram N. Post traumatic complete globe luxation. Delhi J Ophthalmol. 2017;28(54).
- ↑ Jump up to: 20.0 20.1 20.2 Kunesh J, Katz S. Spontaneous globe luxation associated with contact lens placement. Arch Ophthalmol. 2000;118(4):410–1
- ↑ Eing F, Cruz AAV e. Surgical treatment of globe subluxation in the active phase of the myogenic type of Graves orbitopathy: case reports. Arq Bras Oftalmlogica. 2012;75
- ↑ Clendenen S, Kostick D. Ocular globe luxation under general anesthesia. Anesth Analg. 2008;107:1630–1
- ↑ Amaral M, Carvalho M, Ferreira A, Mesquita R. Traumatic globe luxation associated with orbital fracture in a child: a case report and literature review. J Maxillofac Oral Surg. 2015;14:323–30
- ↑ Jump up to: 24.0 24.1 Lida S, Kogo M, Siguira T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J oral Maxillofac Surg. 2001;30:286–90
- ↑ Jump up to: 25.0 25.1 25.2 25.3 Amaral MBF, Nery AC. Traumatic globe dislocation into paranasal sinuses: Literature review and treatment guidelines. J Cranio-Maxillo-Facial Surg. 2016;1–6
- ↑ Jump up to: 26.0 26.1 26.2 26.3 Nauli R, Kartiwa A, Dahlan R, Boesoirie SF, Boesoirie K, Prahasta A. Visual Recovery After Combining Immediate Reposition with Early Intravenous Steroid and Neuroprotective Agent Administration in a Patient with Traumatic Globe Subluxation: A Case Report. APAO Congress. 2018.
- ↑ Jump up to: 27.0 27.1 Morris W, Ossborn F, JC Flemming. Traumatic evulsion of the globe. Ophthal Plast Reconstr Surg. 2002;18:261–7
- ↑ NG J, Payner T, Holck D, Martin R, WT Nunery. Orbital trauma caused by bicycle hand brakers. Ophthal Plast Reconstr Surg. 2004;20(1):60–3
- ↑ Santos T, Vajgel A. Avulsion of globe following maxillofacial trauma. J Craniofac Surg. 2012;62(7):812–3
- ↑ Sardos D Saint, Hamel P. Traumatic globe luxation in a 6 year old girl playing with a tube of wrapping paper. J AAPOS. 2007;11:406–7
- ↑ Poroy C, Cibik C, Bulent Yazici. Traumatic globe subluxation and intracranial injury caused by bicycle brake handle. Arch Trauma Res. 2016;5(3)
- ↑ Jump up to: 32.0 32.1 32.2 32.3 Boesoirie SF, Thaufiq L. Reconstruction of Supraorbital fracture with Globe Prolapse using Miniplate and Screw. In: The 11th National Congres and 32nd Annual Meeting IOA. 2006
- ↑ Jump up to: 33.0 33.1 33.2 Abreshami M, Aletaha M, Bagheri A, Bagheri SH, Shahin Yazdani. Traumatic subluxation of the globe into the maxillary sinus. Ophthal Plast Reconstr Surg. 2007;23(2):156–8
- ↑ Kang B Do, Jang MH. A case of blowout fracture of the orbital wall with eyball entrapped within ethmoid sinus. Korean J Ophthalmol. 2003;17:149–53
- ↑ Jump up to: 35.0 35.1 Tranfa F, Matteo G Di, Salle F Di, Bonavolonta G. Traumatic displacement of the globe into the ethmoid sinus. J Ophthalmol. 2000;130(2):253–4
- ↑ Jump up to: 36.0 36.1 36.2 Pillai S, Mahmood MA, Limaye SR. Complete evulsion of the globe and optic nerve. BR J Ophthalmol. 2015;71:69–72
- ↑ Jump up to: 37.0 37.1 Sundar G. Orbital Fractures. Principles. concepts and managament. Sundar G, editor. Imaging Science Today, USA; 2018
- ↑ Jump up to: 38.0 38.1 Middleton T, Smith R. Optic nerve avulsion secondary to traumatic enucleation. Neurosurgery. 1987;21:89–91
- ↑ Suzuki N, Fujitsu K, N Tanaka. Traumatic enucleation of the eye ball-report of a case and considerations concerning the pathogenic mechanism of intracranial complications. No Shinkei Geka. 1988;16:1293–7
- ↑ Plager D, Parks M. Recognition and repair of the lost rectus muscle. A Report of 25 cases. Ophthalmology. 1990;97:131–7
- ↑ Kim S, Baek S. Traumatic dislocation of the globe into the maxillary sinus associated with extraocular muscle injury. Graefe’s Arch Clin Exp Ophthalmol. 2005;243:1280–3
- ↑ Pereira FJ, Bettega RN de P, Cruz AAV e. Management of globe luxation followed by traumatic liquoric fistula: case report. Arq Bras Oftalmlogica. 2011;74:58–60
- ↑ Shimia M, Sayyahmelli S. Traumatic displacement of the globe into the brain. Rawal Med J. 2009;34
- ↑ Gollapudi PR, Nandigama PK, Sharath Kumar Maila. Traumatic intracranial prolapse of eyeball-a case report. Br J Neurosurg. 2013;27(1)
- ↑ Tse D. Simple maneuver to reposit a subluxed globe. Arch Ophthalmol. 2000;118(3):410–1
- ↑ Jump up to: 46.0 46.1 Kelly EW, Fitch MT. Recurrent spontaneous globe luxation: A Case Report and review of manual reduction techniques. J Emerg Meidicine. 2013;44:17–20
- ↑ Love J, Love NB. Luxation of the globe. AM J Emerg Med. 1993;11:61–3
- ↑ Panje W, Gross C, Anderson R. Sudden blindness following facial trauma. Otolaryngol Heade Neck Surg. 1981;89:941–8
- ↑ Jump up to: 49.0 49.1 Haggerty C, Roman P. Repositioning of a traumatically displaced globe with maxillary antrostomy: review of the literature and treatment recomedations. J Oral Maxilofac Surg. 2013;71:1915–22
- ↑ Choudhury D, Sharma PK. A Case report of traumatic dislocation of eyeball. Niger J Ophthalmol. 2016;24:89–91
- ↑ Shore D, Anderson D, Cutler N. Prediction of self mutilation in hospitalized schizophrenic. Am J Psychiatry. 1978;135:1406–7
- ↑ Jump up to: 52.0 52.1 Kumari E, Chakraborty S, Ray B. Traumatic globe luxation: a case report. Indian J Ophthalmol. 2015;63(8):682–4
- ↑ Jump up to: 53.0 53.1 Gupta R, Gupta P. Complete globe protrusion post trauma. ISOR J Dent Med Sci. 2013;3(6):28–9
- ↑ Amaral MBF, Carvalho MF, Ferreira AB, Alves RM. Traumatic globe luxation asscociated with orbital fracture in a child: A case report and literature review. J Maxillofac Oral Surg. 2012;1:323–30
- Das D, Mohapatra A, Modaboyina S, Agrawal S. Bilateral globe luxation with multiple facial fractures: what next? BMJ Case Rep. 2021 Sep 3;14(9):e244099. doi: 10.1136/bcr-2021-244099. PMID: 34479895; PMCID: PMC8420692.
- Vránová K, Chytilová K, Dobiáš M, Tvrdý P, Handlos P. Traumatic dislocation of the eye into the maxillary sinus: Case report and literature review. J Forensic Sci. 2021 Sep;66(5):2002-2005. doi: 10.1111/1556-4029.14742. Epub 2021 Apr 25. PMID: 33895989.