Thygeson Superficial Punctate Keratitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Definition
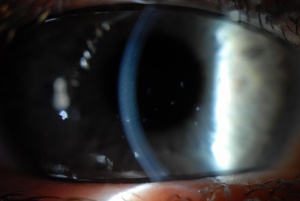
Described in 1950 by Phillips Thygeson in a case report series, Thygeson's superficial punctate keratitis (TSPK) is an insidious, chronic and recurrent disorder, characterized by small and elevated oval corneal intraepithelial, whitish-gray opacities, extending to the entire anterior surface of the cornea of both eyes. Corneal lesions show a tendency for the central pupillary area distribution with mild or absent conjunctival inflammation and no association to systemic disease. [1][2] Later clinical reports and diagnostic imaging modalities such as in vivo confocal microscopy [3][4] have shown that TSPK occurs within the anterior stroma as well epithelial layers, and can result in anterior stromal scarring.[5]
Epidemiology
There are no specific data on the epidemiology of the disease. TSPK may affect both sexes, but a higher incidence has been reported in females. [1] The onset of the disease occurs between the second and third decades of life, with a range of 2.5 to 70 years of age (median: 29 years). It is probable that the prevalence and distribution of the disease is underestimated, as there are limited recent publications.
Pathophysiology
The pathophysiology of TSPK remains unknown. Both, viral and immunologic mechanisms have been implicated. Adenovirus, herpes simplex virus, and varicella zoster virus, have all been implicated as a possible causes of the disease. However, Braley and Alexander [6] provided questionable results suggesting a virus may be responsible for TSPK, and in 1974, Lemp, et al [7] isolated varicella zoster virus from the corneal surface of a 10-year-old boy with TSPK. More recent studies using polymerase chain reaction (PCR), were not able to detect varicella zoster virus from eyes with TSPK, providing doubts this virus is a causative agent. [8][9]
On the other hand, an immune based etiology has also been proposed, since the presence of the HLA-DR3, a class-II MHC molecule associated with immune response genes and multiple autoimmune disorders (Gluten enteropathy, Addison's and Sjögren's syndromes, systemic lupus erythematosus, diabetes mellitus) has been positively implicated to patients with TSPK. [10]
Clinical manifestations
The disease is usually bilateral, but may be asymmetric. Patients frequently experience photophobia, tearing, burning, foreign body sensation, and irritation during exacerbations. Pain, and blurry vision are also common [10]. Redness of the eyes or mucous secretion may be present. The course of the disease is variable, one episode can last from 1 to 2 months and the remission can take as long as 6 weeks. Some reports suggest that after 4 years the disease tends not to recur in most cases without complications. [10] Nevertheless, there are reports from patients observed over the course of more than 20 years with TSPK, and in one case, the disease lasted for 41 years.[11]
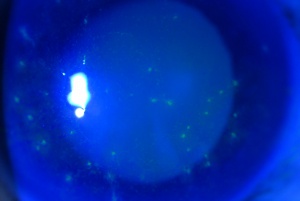
The typical TSPK is an elevated or flat round-oval shaped, gray-whitish lesion, occupying the central intraepithelial corneal area with minimal underlying stromal edema or inflammation. The acute lesion may stain minimally with fluorescein, and may or may not stain with vital dyes (rose bengal or lissamine green). [12] On occasions, the lesion is described as starry, and in the late stages, subepithelial fibrosis or an anterior stromal scar can be noticed. Around 20 of them are present in each eye, but up to 50 lesions have been reported. The lesions tend to disappear without leaving a trace in the course of 4 to 6 weeks. Corneal sensitivity is usually preserved or slightly diminished. The conjunctiva remains quiet but for a few cases where redness and filament formation may also be found. [12]
Pathology
The histopathology of TSPK is characterized by intra and intercellular edema at the level of the corneal epithelium [13][4] and involvement of the subepithelial nerve plexus, Bowman’s membrane, and the anterior stroma. These changes are most severe in eyes with a longer duration of TSPK. [2][4] Under confocal microscopy, keratocytes show highly reflective nuclei and cell bodies of irregular size, orientation, and shape. These changes were present under the intraepithelial lesions, and in other areas where lesions were not present. They are thought to be related to the duration of the disease, and were not seen in normal controls. [4] There is no evidence of the presence of inflammatory cells in the areas of corneal stroma adjacent to the intraepithelial lesions. [13] Using confocal microscopy, Kobayashi reported three findings that were consistently present in all patients with TSPK: aggregates of highly reflective deposits with a starburst-like appearance that might correspond with punctate lesions at the superficial and basal epithelial cell layers, invasion of Langerhans cells at the basal epithelial layer, and anterior stromal haze. [3]
Differential diagnosis
Based on the clinical course and the clinical manifestations of the disease, particularly the typical corneal lesions, the diagnosis of TSPK should not represent a problem. However, there are several clinical entities that may resemble TSPK and should be considered in the differential diagnosis:
- Staphylococcal epithelial keratitis
- Pneumococcal conjunctivitis
- Seborrheic blepharitis
- Keratoconjunctivitis sicca (Sjögren syndrome)
- Neurotrophic keratitis
- Exposure keratitis
- Recurrent corneal erosion syndrome
- Map-dot-fingerprint dystrophy
- Viral keratitis
- Vernal keratoconjunctivitis
- Others: molluscum contagiosum, trauma.
Treatment
Multiple therapeutic strategies have been tried over the years for the management of TSPK, but none of them have resulted to be entirely successful. Antibiotics have not been effective so far. [14] Antivirals have shown mixed results; such as, mild improvements reported with trifluridine therapy, [15]while idoxuridine has been shown to cause persistent anterior stromal ghost opacities and scarring, and is therefore contraindicated for TSPK. [6][7][16][14]
Topical lubricants are only effective for partially relieving the clinical symptoms of TSPK. [17] On the contrary, topical corticosteroids are considered as mainstay treatment for TSPK because they are highly effective in controlling both, the clinical signs and symptoms of the disease, although there has been a lot of non-proven speculations that they may prolong the clinical course of the disease. [12][14] An important point of corticosteroid treatment for TSPK is that in most cases, they must be tapered gradually over a long period of time (months) until an infrequent, but regular dose is achieved (i.e. weekly or biweekly). The goal of corticosteroid therapy is to administer the minimum dosage and strength possible to control the symptoms of TSPK. [11][18]
Due to its therapeutic success and safety profile compared to corticosteroids, topical cyclosporine (CsA) has been proposed as first-line treatment for patients with TSPK. [15][19][20] However, CsA has not been compared to corticosteroids in a controlled clinical trial for the treatment of TSPK, and one well-recognized inconvenience of topical CsA is stinging at instillation that may compromise therapeutic compliance. [19][20] Another steroid sparing agent that has been used with some success is topical tacrolimus, both as drops [21] and ointment [22].
Another alternative for severe TSPK is the use of extended-wear therapeutic soft contact lenses, although potential complications such as microbial keratitis may occur. [23]Contact lenses improve symptoms by covering the elevated corneal lesions and nerves, which are constantly in friction with the palpebral conjunctiva during blinking. [14][16]
There have been a few case reports of TSPK patients treated with excimer laser phototherapeutic keratectomy (PTK) with only partial improvement of signs and symptoms, but with a high rate of recurrence of the corneal lesions, making it no alternative for the management of the disease. [24][25][26]
Summary
In summary, the following recommendations have been made with respect to the treatment of TSPK. The benign course of the disease requires the use of lubricant eyedrops and topical surface steroids, at low and infrequent dose for prolonged periods of time with close monitoring of intraocular pressure and cataract formation. [16] Topical CsA or tacrolimus can be used as an alternative treatment to steroids, taking into account the possibility of intolerance, cost and poor compliance issues. [19][20] In severe cases, extended-wear therapeutic contact lenses could be used for the relief of TSPK symptoms, monitoring for corneal infections and intolerance. [24] After the diagnosis is established, the disease may last for many years with a waxing and waning clinical course, and a tendency to disappear without clinical sequelae.[5]
References
- ↑ Jump up to: 1.0 1.1 Thygeson P: Superficial punctate keratitis, JAMA 144: 1544, 1950.
- ↑ Jump up to: 2.0 2.1 2. Thyeson P: Further observations on superficial punctate keratitis, Arch Ophthalmol 66:158, 1962.
- ↑ Jump up to: 3.0 3.1 Kobayashi A, Yokogawa H, Kazuhisa S. In Vivo Laser Confocal Microscopy Findings of Thygeson Superficial Punctate Keratitis. Cornea 2011;30:675–680.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Watson SL, Hollingsworth J, Tullo AB. Confocal microscopy of Thygeson’s superficial punctate keratopathy. Cornea 2003;22:294-9.
- ↑ Jump up to: 5.0 5.1 Fintelmann RE, Vastine DW, Bloomer MM, Margolis TP. Thygeson superficial punctate keratitis and scarring. Cornea. 2012 Dec;31(12):1446-8.
- ↑ Jump up to: 6.0 6.1 Braley AEK, Alexander RC: Superficial punctate keratitis: isolation of a virus, Arch Ophthalmol 50:147, 1953
- ↑ Jump up to: 7.0 7.1 Lemp MA, Chambers RW, Lurdy J: Viral isolation in superficial punctate keratitis, Arch Ophthalmol 91:8, 1974.
- ↑ Reinhard T, Roggendorf M, Fengler I, Sundmacher R. PCR for varicella zoster virus genome negative in corneal epithelial cells of patients with Thygeson's superficial punctate keratitis. Eye. 2004;18(3):304-5.
- ↑ Connell PP, O'Reilly J, Coughlan S, Collum LM, Power WJ. The role of common viral ocular pathogens in Thygeson's superficial punctate keratitis. Br J Ophthalmol. 2007;91(8):1038-41.
- ↑ Jump up to: 10.0 10.1 10.2 Darrell RW: Thygeson's superficial punctate keratitis: natural history and association with HLA-DR3, Trans Am Ophthalmol Soc 79:486, 1981.
- ↑ Jump up to: 11.0 11.1 8. Tanzer DJ, Smith RE: Superficial punctate keratitis of Thygeson: the longest course on record? Cornea. 1999 Nov;18(6):729-30.
- ↑ Jump up to: 12.0 12.1 12.2 Thygeson P: Clinical and laboratory observation on superficial punctate keratitis, Am J Ophthalmol 61:1344, 1966.
- ↑ Jump up to: 13.0 13.1 Cheng L, Young A, Wong A, et al. In vivo confocal microscopy of Thygeson’s superficial punctate keratitis. Clin Exp Ophthalmol 2004; 32:325-7.
- ↑ Jump up to: 14.0 14.1 14.2 14.3 Tabbara KF, Ostler HB, Dawson C, Oh J. Thygeson's superficial punctate keratitis. Ophthalmology. 1981;88(1):75-7.
- ↑ Jump up to: 15.0 15.1 Nesburn AB, Lowe GH III, Lepoff NJ, et al. Effect of topical trifluridine on Thygeson’s superficial punctate keratitis. Ophthalmology 1984;91:1188-92.
- ↑ Jump up to: 16.0 16.1 16.2 Goldberg DB, Schanzlin DJ, Brown SI: Management of Thygeson's superficial punctate keratitis, Am J Ophthalmol 89:22 1980.
- ↑ Gock G, Ong K, McClellan K. A classical case of Thygeson’s superficial punctate keratitis. Aust NZ J Ophthalmol 1995;23:76-7
- ↑ Duszak RS. Diagnosis and management of Thygeson’s superficial punctate keratitis. Optometry 2007; 78, 333-338.
- ↑ Jump up to: 19.0 19.1 19.2 Reinhard T, Sundmacher R: Topical cyclosporin A in Thygeson's superficial punctate keratitis. Graefes Arch Clin Exp Ophthalmol 1999; 237(2):109-112).
- ↑ Jump up to: 20.0 20.1 20.2 Benitez-del Castillo JM, Garcia-Sanchez J. Effect of topical cyclosporin-A on Thygeson’s superficial punctate keratitis. Doc Ophthalmol 1996–7;93(3):193–8.
- ↑ Shoughy SS, Tabbara KF. Topical Tacrolimus in Thygeson Superficial Punctate Keratitis. Cornea. 2020 Jun;39(6):742-744. doi: 10.1097/ICO.0000000000002224. PMID: 31842035
- ↑ Marquezan MC, Nascimento H, Vieira LA, Serapião M, Ghanem RC, Belfort R Jr, Freitas D. Effect of Topical Tacrolimus in the Treatment of Thygeson's Superficial Punctate Keratitis. Am J Ophthalmol. 2015 Oct;160(4):663-8. doi: 10.1016/j.ajo.2015.06.019. Epub 2015 Jun 29. PMID: 26133248
- ↑ Forstot SL., Bender PS: Treatment of Thygeson's superficial punctate keratopathy with soft contact lenses, Am J Ophthalmol 88:186, 1979.
- ↑ Jump up to: 24.0 24.1 Goldstein MH, Feistmann JA, Bhatti MT. PRK-pTK as a treatment for a patient with Thygeson' superficial punctate keratopathy. CLAO J. 2002; 28(4):172-3.
- ↑ Fite SW, Chodosh J. Photorefractive keratectomy for myopia in the setting of Thygeson's superficial punctate keratitis. Cornea. 2001;20(4):425-6.
- ↑ Netto MV, Chalita MR, Krueger RR. Thygeson's superficial punctate keratitis recurrence after laser in situ keratomileusis. Am J Ophthalmol. 2004;138(3):507-8.