Three-Dimensional Display Systems for Surgery in Ophthalmology
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Over the past two decades, new innovations have led to a dramatic increase in the number of microsurgeries performed. However, traditional microsurgery using the traditional binocular microscope can lead surgeons to deleterious neck and back postures that cause musculoskeletal fatigue and injuries, which has been associated with reduced surgical longevity [1]. The prevalence of neck, upper body, or lower back symptoms among ophthalmologists has been reported to be as high as 62% [2][3].
Three-dimensional (3D) display systems were first developed for aircraft and military use. Innovative, ground-breaking developments brought this technology to the operating theater. Live three-dimensional (3D) display systems have been adopted in medicine, particularly after the creation of the TrueVision 3D Visualization System for Microsurgery (TrueVision Systems, Inc, Santa Barbara, California), and these have applications in many surgical specialties.
Conventional 3D systems are classified as either active or passive systems.
- In active systems, the 3D image is obtained by showing high-speed consecutive images for the right and left eyes alternatively, while a special pair of electronic glasses actively suppresses the image in the other eye.
- In passive 3D systems, the three-dimensional image is acquired by mixing two images horizontally and then passively separating them into polarized 3D glasses.
Heads-up surgery in ophthalmology
The term “heads-up surgery” describes the performance of microsurgical procedures not by looking at the eyepieces of the microscope, but by viewing the microscopic image on a panel display sent from a 3D camera [4]. It is derived from the so-called “head-up display”, a display system first used in aircraft flight decks which projects an image into the normal field of view. This display system allows visualization in a “heads-up” position. These terms differ in that the image in heads-up surgery is shown on a display rather than projected.
Heads-up surgery eliminates the constraints imposed by the standard binocular microscope and minimizes fatigue by providing greater degrees of freedom to operate in a more neutral, physiologic position, without affecting the image quality or technical difficulty. It is also potentially an aide to surgical teaching since multiple people in the same room can share the high-resolution view of the surgeon.
Cataract and the anterior segment
TrueVision 3D system (TrueVision Systems Inc., Santa Barbara, CA, USA)
In ophthalmology, cataract and anterior segment surgery in human eyes using heads-up surgery was first reported by Weinstock in 2010 [5][6]. At the 2010 American Society of Cataract and Refractive Surgery (ASCRS) meeting in Boston, he presented a retrospective analysis comparing cataract surgery using standard binocular microscope with a microscope equipped with TrueVision 3D system (TrueVision Systems Inc., Santa Barbara, CA, USA). Weinstock reported excellent outcomes in both groups, with minimal procedure time difference between groups. Interestingly, the rate of unplanned vitrectomy was three times higher in the standard microscope group compared with the TrueVision group.
The TrueVision 3D Surgical System is a camera unit that attaches to standard surgical microscopes, sending stereoscopic images and video to a 3D, high-definition (HD), large-screen monitor positioned a few feet from the surgeon, providing visualization in real time. The US Food and Drug Administration (FDA) has granted clearance for the TrueVision Refractive Cataract Toolset, an application that provides 3D graphical overlays for image-guided cataract surgery. More recently, TrueVision has developed the TrueGuide and the TruePlan applications, which have been designed for intelligent surgical planning to aid in achieving targeted refractive outcomes, including the use of toric intraocular lens (IOL) [7]. In one study, Solomon J reported results of toric IOL implantation using TrueGuide. 83.3% of eyes were corrected to <0.50 D of cylinder, and 100% were corrected to <1.00 D cylinder. In addition, 80% of the eyes had final vision 20/20, and 100% of the eyes achieved 20/25 or better. [7] [8]
Other anterior segment surgeries have been performed using the heads-up system, including amniotic membrane transplantation [9] and corneal surgery. Mohamed YH et al. have reported the first case of corneal surgery using the heads-up system [10]. They performed a non-Descemet Stripping Automated Endothelial Keratoplasty (nDSAEK) for post-traumatic bullous keratopathy, and reported great visual experience and ergonomics. However, the authors state that frequent adjustment of focus was needed for clear stereoscopic view of the flap.
Vitreoretinal procedures
The heads-up surgery in the retina world was introduced by Eckardt and Paulo[4]. They conducted a study to assess whether vitreoretinal surgery could be performed using the heads-up display system with a 3D, high dynamic range surgical camera, a HD LCD display which requires the use of passive 3D polarized glasses. The authors suggested the main advantage of heads-up technique over standard surgery is the superior ergonomics. However, they report that this technique was not more difficult than traditional surgery. Additionally, the brightness of the surgical field can be superior than that of traditional surgery, without exposing the retina to additional light. Electronic amplification of the camera's signal to increase brightness might be helpful in situations of vitreous hemorrhages, opaque media, or darkly pigmented fundi.
NGENUITY® 3D Visualization System (Alcon, TX, USA)
This three-dimensional visualization system has been used extensively for ocular surgeries including strabismus surgery, cataract surgery, glaucoma surgery, and vitreoretinal surgeries.[11] [12] [13] [14] [15] This system utilizes passive circularly polarized 3D polarization glasses, and a 55-inch 4K ultra-HD OLED (organic light emitting diode) display.[16] Potential advantages include similar surgical time/complication rate compared to conventional microscope, decreased power of endoilluminator, reduced phototoxicity, ease of use in uncommon situations including severe kyphosis, reduced need of triamcinolone staining of the vitreous, and high surgeon and nurse satisfaction scores; recent enhancements allow allow for integration of patient information and utilization of "color channels" that can enhance visualization of microtissues such as the internal limiting membrane.[16] Reported limitations include difficult logistics, cost, assistant's discomfort, difficulty due to sudden head movement of the patient, and poor view in media opacities. [16]
Other heads-up 3D visualization systems in ophthalmology include:
- Sony HD Medical Display system (Sony, Tokyo, Japan)[17]
- MKC 700 HD and CFA 3DL1 (Ikegami, Tokyo, Japan)
- Artevo 800 (Zeiss, Germany)
- Panoramic RUV viewing system for vitreoretinal surgery (Leica, Wetzlar, Germany)
Head-mounted systems in ophthalmology
Ivan Sutherland’s early experiments in the 1960s led to the development of the “head-mounted display systems”, abbreviated HMS. Sutherland constructed an HMS that displayed a simple wireframe model on a binocular display. [19] The main applications of HMS have included military, police, firefighting, and civilian-commercial use, namely in video gaming and sports. HMS has been used by authorities to display tactical information such as maps or thermal imaging data while viewing a real scene.
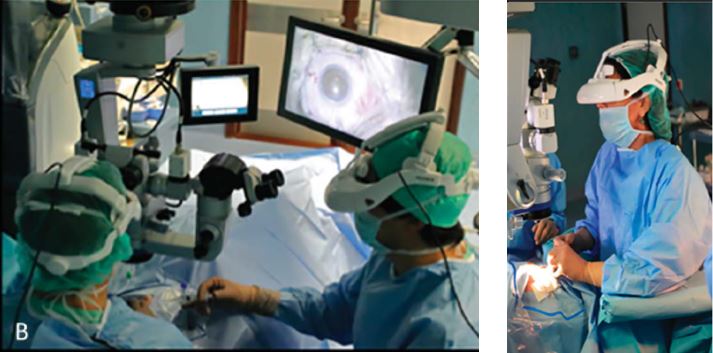
The use of this innovative HMS technology in Ophthalmology was first reported by our group, [Dutra-Medeiros et al.][18]. We performed several ophthalmic surgeries using the Haag-Streit Surgical microscope HS Hi-R NEO 900 (Haag-Streit Surgical GmbH, Wedel, Germany) connected to the Sony Head-Mounted System HMS-3000 MT device.
Sony (Sony Electronics, Inc, Tokyo, Japan) has been a pioneer in the field on head-mounted display, and first ventured into the operating room in 2012. The HMS-3000MT [20] is a personal viewing system that provides a 3D color video display of images from 3D surgical camera systems. It consists of the HMI-3000MT image processor unit plus the HMM-3000MT head mounted display that provides a stereoscopic visualization from the imaging system, and provides a 3D color video display of images from the 3D, full-HD surgical camera systems MCC-3000 MT. This system has the option to connect a second head mounted monitor, giving other theater staff a simultaneous 3D view. This device is compliant and certified for IEC 60601-1 and product safety standards in the U.S.A., Canada, and Europe.
Depth perception inside the HMS device requires different images for the left and right eyes. The head-mounted system differs from conventional 3D systems by showing two simultaneous images, one for each eye, avoiding the ghosting image effect caused by cross-talk in active 3D systems. The system of dual video inputs using two independent organic light-emitting diodes (OLED) panels offers a complete separate video signal to each eye, which provides the maximum resolution for each image, and maximum frame rate for each eye [20]. The HMS provides a high-resolution (1280 x 720) stereoscopic images with precise reproduction of colors and blacks.
Our group performed several ophthalmic surgeries [18] including pars plana vitrectomy, alone and combined with phacoemulsification/intraocular lens (IOL) implantation. Other vitreoretinal techniques were performed, including subluxated IOL extraction, epiretinal membrane peeling, internal limiting membrane peeling, endolaser photocoagulation, and tamponade with silicone oil and sulfur hexafluoride gas.
Other head-mounted systems include:
- Avegant Glyph retinal projection system (Avegant Corp., Belmont, CA, USA)
- Clarity™ (Beyeonics Surgical, Haifa, Israel)
Conclusions
Three-dimensional display systems are showing ever more promising results in the field of ophthalmology, both for anterior and posterior segment surgeons. Heads-up surgery using 3D display screens has been increasingly accepted due to their advantages in terms of ergonomics and surgical teaching/coordination. The use of head-mounted display systems is a novel emerging concept in ophthalmology. In our experience [18], the Sony HMS-3000MT helmet was well-fitted into the surgeon’s heads and its weight was not uncomfortable. The helmet allows the surgeon to see his/her own hands and surgical instruments by looking down. We consider HMS technique for vitreoretinal surgery to have a short learning curve. In addition to the great image quality, we experienced great depth perception and spatial orientation. The wide 45º horizontal viewing angle enables a more natural visual experience. Since the assistant surgeons in the operating theater can also wear a helmet and experience simultaneous, stereoscopic images as the main surgeon, this technique may prove to be an excellent tool for live surgery teaching and training in the future.
References
- ↑ Mendez BM, Chiodo MV, Vandevender D, et al. Heads-up 3D microscopy: an ergonomic and educational approach to microsurgery. Plast Reconstr Surg Glob Open 2016;4:e717.
- ↑ Dhimitri KC, McGwin G, McNeal SF, et al. Symtoms of musculoskeletal disorders in ophthalmologists. Am J Ophthalmol 2005;139:179–81.
- ↑ Hyer JN, Lee RM, Chowdhury HR, Smith HB, Dhital A, Khandwala M. National survey of back & neck pain amongst consultant ophthalmologists in the United Kingdom. Int Ophthalmol. 2015;35:769–75.
- ↑ Jump up to: 4.0 4.1 Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina 2016;36:137–147.
- ↑ Weinstock RJ, Desai N. Heads up cataract surgery with the TrueVision 3D Display System. In: Garg A, Alio JL, eds. Surgical Techniques in Ophthalmology—Cataract Surgery. New Dehli, India: Jaypee Medical Publishers; 2010:124–127.
- ↑ Weinstock RJ. Operate with your head up. Cataract Refract Surg Today. 2011;8:66, 74
- ↑ Jump up to: 7.0 7.1 TrueGuide brochure, available at http://www.truevisionsys.com/TVS_TrueGuideBrochureN032515.final.pdf
- ↑ Jonathan Solomon at ACOS/CXL Congress Deer Valley 2014 – information available in the TrueGuide brochure
- ↑ Uematsu M, Amniotic membrane transplantation with head-up surgery, presentation at the Annual Cornea Day in the 21th ESCRS Winter Meeting Maastricht 2017
- ↑ Mohamed, Yasser Helmy et al. “First Experience of nDASEK with Heads-up Surgery: A Case Report.” Ed. Samantha Martin. Medicine 96.19 (2017): e6906. PMC. Web. 29 May 2017.
- ↑ Hamasaki I, Shibata K, Shimizu T, et al. Lights-out surgery for strabismus using a heads-up 3D vision system. Acta Med Okayama. 2019;73:229–33.
- ↑ Weinstock RJ, Diakonis VF, Schwartz AJ, Weinstock AJ. Heads-up cataract surgery: complication rates, surgical duration, and comparison with traditional microscopes. J Refract Surg. 2019;35:318–22.
- ↑ Kita M, Mori Y, Hama S. Hybrid wide-angle viewing-endoscopic vitrectomy using a 3D visualization system. Clin Ophthalmol. 2018;12:313–7.
- ↑ Skinner CC, Riemann CD. “Heads up” digitally assisted surgical viewing for retinal detachment repair in a patient with severe kyphosis. Retina Cases Brief Rep. 2018;12:257–9.
- ↑ Coppola M, La Spina C, Rabiolo A, et al. Heads-up 3D vision system for retinal detachment surgery. Int J Retin Vitr. 2017;3:46.
- ↑ Jump up to: 16.0 16.1 16.2 Moura-Coelho, Nuno,l, José Henriques, Gama Pinto João Nascimento, et al. “Three-Dimensional Display Systems in Ophthalmic Surgery – A Review.” European Ophthalmic Review 13, no. 1 (2019): 31. https://doi.org/10.17925/EOR.2019.13.1.31.
- ↑ Mohamed YH, Uematsu M, Inoue D, Kitaoka T. First experience of nDSAEK with heads-up surgery: a case report. Medicine (Baltimore). 2017;96:e6906
- ↑ Jump up to: 18.0 18.1 18.2 18.3 Dutra-Medeiros M , Nascimento J, Henriques J, Barrão S, Fernandes-Fonseca A, Aguiar-Silva N, Moura-Coelho N, Ágoas V. THREE-DIMENSIONAL HEAD-MOUNTED DISPLAY SYSTEM FOR OPHTHALMIC SURGICAL PROCEDURES Retina. 2017 Jan 16. doi: 10.1097/IAE.0000000000001514. [Epub ahead of print]
- ↑ Scherffig L. Moving into view: enacting virtual reality. Media Tropes eJournal 2016;1:1913–6005.
- ↑ Jump up to: 20.0 20.1 Sony’s HMS-3000MT brochure, available at https://pro.sony.com/bbsccms/assets/files/mkt/med/brochures/HMS-3000MT_brochure.pdf


