Temporary Keratoprosthesis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
A temporary keratoprosthesis is a device that is placed during combined corneal and vitreoretinal surgeries to allow for a clear surgical view of the posterior segment in eyes with concurrent corneal pathology. Prior to the advent of the temporary keratoprosthesis, patients with corneal opacities and vitreoretinal disease would undergo penetrating keratoplasty alone followed by posterior segment surgery after adequate healing and resolution of corneal edema which could take months. Commonly, traumatic eye injuries affect both the anterior and posterior segment, and repair of this pathology can be time-sensitive. The device can also be used during a modified triple procedure (cataract extraction, intraocular lens placement, penetrating keratoplasty) to maintain a closed system with a clear view during lens removal. Intraoperative temporary keratoprosthesis allows for timely treatment of vitreoretinal disease despite the status of the cornea. In addition, this device may also be used as a short-term temporary seal for corneas awaiting transplantation (e.g. corneal perforation).[1]
History
The first use of a temporary keratoprosthesis was reported in 1981 with the Landers temporary keratoprosthesis. This device consists of a polymethylmethacrylate (PMMA) threaded biconcave optical cylinder.[1] [2][3][4]However, this initial design did not permit a wide view of the peripheral retina due to a long optical cylindrical axis of 5 mm.[1] In 1989, the Eckardt temporary keratoprosthesis was created. This device is made of silicone rubber material secured by four nylon sutures.[1][5][6][7] However, the soft silicone material causes a clouded view during air-fluid exchange and prevents the keratoprosthesis from recurrent use due to damage from multiple suture tracks.[1] In the early 2010s the Landers wide-field trunkless model was designed, offering a hard PMMA central window with high reusability and a wide view of the peripheral retina without the use of ancillary lenses due to a decreased cylindrical axis of 1 mm.[3][8] In addition, this model was fit with predrilled suture holes in the peripheral flange, allowing easy suturing to the globe.[3][8] The Cobo keratoprosthesis is also available, consisting of a hard quartz corneal window with tapered edges allowing its use in a wide range of corneal trephine diameters.[1][4][9]
The concept of intraoperative temporary corneal grafts is not limited to prosthetic devices. The use of corneal buttons from corneal grafts not suitable for a full penetrating keratoplasty has been documented by Nardi et al in performing closed system combined triple procedures consisting of a temporary corneal graft, cataract extraction, intraocular lens implantation and final penetrating keratoplasty.[10] In the three cases, an 8.5 mm diameter corneal button unsuitable for penetrating keratoplasty was sutured with interrupted sutures and replaced with a permanent allograft after completion of the lens implantation without any perioperative complications.[10] Additionally, the use of an intraoperative temporary sutured soft bandage contact lens was also reported in 2021 by Skevas et al, as a successful alternative to a temporary keratoprosthesis during vitreoretinal surgery in certain situations when appropriate corneal tissue is not available. In the three reported cases, one case solely used a soft bandage contact lens without any adhesion or fixation while two cases involved suturing the contact lens to the globe.[11]
Design
The original principle of design for a temporary keratoprosthesis is the use of a slightly larger trunk diameter relative to the corneal trephine in order to create a watertight seal.[4][12] However, published studies have demonstrated efficient corneal sealing using keratoprosthesis with diameters up to 0.3 mm less than the corneal trephine. In 2011, Watson et al published a study establishing certain criteria for a watertight seal including centering the keratoprosthesis and allowing adequate intact cornea or sclera for predrilled suture holes.[13] These findings support the use of temporary keratoprosthesis in extended scenarios such as ocular trauma involving irregular corneal trephine edges or with diameters larger than available keratoprosthesis sizes.
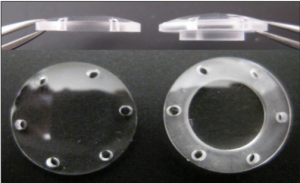
The Landers keratoprosthesis is composed of hard polymethylmethacrylate with a central core of PEG available in diameters of 6.2 mm, 7.2 mm and 8.2 mm for trephine sizes of 6 mm, 7 mm and 8 mm, respectively.[4][9][13] The cylindrical axis length comes in 5 mm and 6.2 mm.[4] By utilizing a hard plastic material, the Landers keratoprosthesis preserves the integrity of the keratoprosthesis from damage from peripheral suturing and allows reusability.[9][13] Due to the low refractive power of the Landers, it is often used in a ‘combined lens system’ by using a polymethylmethacrylate hard lens on top of the keratoprosthesis to produce a magnified view of the macula intraoperatively.
This device was improved upon with the next generation modern wide-field trunkless Landers keratoprosthesis minimizing the need for a combined lens system with a decreased cylindrical axis of 1 mm allowing a wide view of the peripheral retina.[3][8] In cases with irregularly shaped corneal defects, the Landers wide field keratoprosthesis may be used with the corneal window superimposed over instead of within the corneal defect.[4][9] The wide-field Landers has diameters of 6.2 mm, 7.2 mm and 8.2 mm.[4][9][13]
The Eckardt keratoprosthesis is composed of optically clear soft silicone with a hydrophilic surface. It is available in diameters of 7 mm and 8 mm for trephine sizes of 6.7 mm and 8.5 mm, respectively. The cylindrical axis length is 2 mm.[4][5] By utilizing a soft material, the Eckardt keratoprosthesis provides a wider optical zone and shorter vertical length compared to the Landers keratoprosthesis, with a minimum cylindrical length of 5 mm.[4] In addition, the increased elasticity optimizes peripheral molding and sealing to irregular corneal defects.[9]
The Cobo keratoprosthesis is composed of a truncated quarts cone which is autoclavable allowing reusability, available in a diameter of 6.5 mm. Due to the tapered cone design, the keratoprosthesis may be used for a wide range of corneal trephine diameters. The Cobo keratoprosthesis is fitted with a stainless-steel handle which is useful for injection of fluid or gas for internal tamponade during intraoperative hemorrhage.[4]
Video link: https://www.aao.org/annual-meeting-video/use-of-different-types-temporary-keratoprosthesis-
Indications
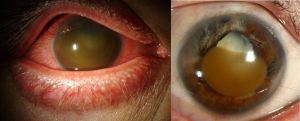
Temporary keratoprosthesis allows for visualization of intraocular structures during combined corneal and vitreoretinal surgery. This is useful in preventing the delay of posterior segment treatment, especially in the setting of ocular trauma where corneal visibility is often limited from corneal blood staining, large edematous corneal wounds, or corneal explosive injury with corneal foreign bodies.[1][14][15] Most commonly performed concurrent vitreoretinal surgeries include pars plana vitrectomy with scleral buckling, retinal reattachment, and foreign body removal.[1][7][14][16]Temporary keratoprosthesis may also be used in combined corneal transplant and additional anterior segment procedures including lensectomy in the setting of a standard or traumatic cataract, lens rupture, or extrusion of the lens.[1][17][18]
Surgical Procedure
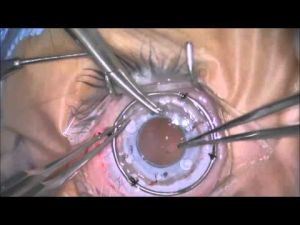
The pathologic cornea is trephined with removal of the corneal button which is discarded or stored in protective viscoelastic material. The temporary keratoprosthesis is chosen with its diameter corresponding to the diameter of the corneal trephine and prepared by injecting saline solution into the infusion line with a 5 cc or 10 cc syringe and 21-gauge blunt needle. The temporary keratoprosthesis is placed in the center of the corneal defect and sutured with 6-0 or 7-0 Vicryl or 9-0 nylon interrupted for fixation onto the sclera through predrilled holes. After proper placement and sealing of the temporary keratoprosthesis, the vitreoretinal surgery may proceed. Anterior vitrectomy may be performed under open sky approach prior to the fixation of the temporary keratoprosthesis, or using a pars plana approach after fixation.
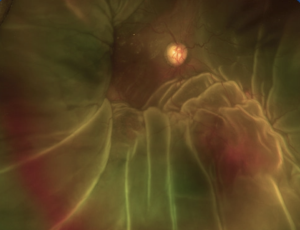
After the vitreoretinal surgery is complete, the temporary keratoprosthesis is removed after adequate posterior segment tamponade with either silicone oil or air. After removal of the temporary keratoprosthesis, corneal transplantation with a permanent allograft may be performed. Due to hypotony of the eye after temporary keratoprosthesis removal, suturing of the penetrating keratoplasty must be performed in a timely fashion to preserve intraocular pressure and avoid suprachoroidal hemorrhage.
In the setting of ocular trauma, the temporary keratoprosthesis may also be replaced with the original trephined corneal button with delayed permanent penetrating keratoprosthesis to decrease the risk of allograft rejection.
Complications
The most common potential complications from temporary keratoprosthesis include suprachoroidal hemorrhage, lack of corneal allograft clarity, derangements in intraocular pressure, sympathetic ophthalmia, and phthisis.[7][16][19][20][21] Although these complications have been documented in the literature, the incidence is low. The degree of complications also varies depending on the preoperative conditions including history of trauma, prior rejection of corneal grafts, preexisting ocular disease, and type of surgery. Temporary keratoprosthesis in open globe repair presents with the highest rates of complications including ciliary body malfunction and secondary graft failure.[15][16][22] However, poor postoperative visual outcomes were more strongly associated with pre-existing disease rather than degree of trauma, with retinal integrity as the major predictor.
Postoperative persistent hypotony is common especially in severely injured eyes, with a possible need for permanent silicone-oil tamponade. However, persistent silicone oil tamponade has also been associated with a higher risk of corneal graft failure compared to cases with silicone oil removal due to interference with corneal nourishment.[1][15][17]
Permanent corneal graft rejection after a combined temporary keratoprosthesis and vitreoretinal surgery in the setting of acute ocular trauma has also been documented.[15][16][23] This is most commonly due to corneal neovascularization secondary to postoperative inflammation, endothelial cell loss, poor postoperative care, and treatment noncompliance. However, the rate of graft rejection is not directly related to the use or lack of temporary keratoprosthesis, but rather with the severity of ocular trauma and complexity of surgery, indicating poor graft healing secondary to ocular inflammation.[7][15][18][22] Roters et al found that corneal graft failure increased if permanent allografts were placed within eight weeks of trauma.[15] However, Dong et al found that timely retinal reattachment within one month of trauma was imperative in dictating postoperative visual outcomes.[18] These studies indicate the need for a case-by-case basis on when to place a permanent penetrating keratoplasty versus temporizing measures such as suturing back the original trephined corneal button.
Alternatives to using a temporary keratoprosthesis during vitreoretinal surgery involves proceeding with open-sky approach or corneal transplantation with an allograft. Using a temporary keratoprosthesis circumvents complications associated with these procedures such as a higher risk of expulsive suprachoroidal hemorrhage, vitreous prolapse, and delayed surgical intervention leading to worse prognosis.[1][13]
Cost
The Landers keratoprosthesis and Cobo keratoprosthesis are manufactured by Ocular Instruments in Bellevue USA with listing prices of $490 and $750, respectively. The Eckardt keratoprosthesis is manufactured by Heinrich Wöhlk Kontaktlinsen in Kiel Germany with unknown public listing price.[5][9]
Treatment Outcomes
Postoperative visual outcomes are highly dependent on the variability of ocular trauma, as well as the extent of retinal pathology. Because of these differences, study outcomes cannot be directly compared between different series and surgical outcomes such as visual acuity must be analyzed in relation to preoperative conditions.[10][11][16][24] However, temporary keratoprosthesis have been well tolerated with minimal complications relative to alternative open-sky approach. In addition, there are well documented benefits regarding timely vitreoretinal surgery which is not possible in cases requiring a preceding penetrating keratoplasty with healing.
The success of combined cases using temporary keratoprosthesis may be measured by the status of the permanent corneal graft as well as resolution of anatomic defects, most notably retinal reattachment. The most common indicators of success are postoperative visual acuity and absence of complications. The following paragraphs describe current literature on outcomes from using different devices for temporary keratoprosthesis.
Traditional devices (Eckardt, Landers):
Surgical outcomes are difficult to compare between different traumatic versus non-traumatic cases due to varying inclusion criteria, differences in preoperative vision, severity of ocular trauma, and surgical technique. This also complicates comparison between devices, and between studies investigating the same device. However, overall temporary keratoprosthesis results in improved visual outcomes, corneal clarity, and retinal attachment.
In a study published by Alvarez et al comparing surgical results of Eckardt keratoprosthesis in vitreoretinal surgery in traumatic versus non-traumatic cases, there were similar rates of success in corneal clarity (49% in both groups), with higher rates of success in retinal reattachment in non-trauma patients (90% non-trauma vs 78% trauma) and higher rates of visual acuity improvement in trauma patients (47% non-trauma vs 67% trauma). These differences in visual acuity may be explained by a higher rate of phthisis in the non-trauma group despite similar rates of retinal detachment and graft rejection.[16]
In a study investigating the use of Eckardt keratoprosthesis in 31 eyes in the setting of ocular trauma, 47% of eyes showed improved final visual acuity and 41.9% of cases maintained a clear corneal graft.[20] Similarly, Roters et al reported 34 cases with only 21% with improved visual acuity. However, there was a higher prevalence of extensive pre-existing disease compared to other studies associated with more extensive surgical procedures and worse outcomes.[15] In a study investigating 5 traumatic and 3 non-traumatic eyes, 75% of eyes showed improved final visual acuity and 88% of eyes maintained retinal attachment and corneal clarity.[24]
In a study focused on the use of Landers keratoprosthesis in ocular trauma in 107 eyes, 86% of eyes were salvaged with useful visual function, 80% of eyes with improved final visual acuity, and 72.9% maintaining corneal clarity with retinal reattachment.[18] Another study of 12 eyes demonstrated improvement in visual acuity in 59% of eyes and 92% of eyes with retinal reattachment, but only 25% of eyes maintained a clear corneal graft after one year.[21] A smaller study of 8 eyes found 62.5% of eyes with improvement in visual acuity, 75% of eyes with retinal reattachment, and 62.5% of eyes with corneal clarity over a mean follow up period of 21 months.[22]
Graft-based corneal buttons:
In a study by Nardi et al documenting using corneal buttons from corneal grafts not suitable for allograft in combined vitreoretinal cataract cases, none of the patients experienced any complications. In contrast, one patient who underwent an open sky cataract extraction instead of using a temporary corneal button experienced an expulsive choroidal hemorrhage in the contralateral eye.[10] Using a temporary corneal button allowed maintenance of a positive vitreous pressure and lowered the risk of such complications.
Soft bandage contact lenses:
In a study by Skevas et al successfully replacing a traditional temporary keratoprosthesis with a sutured soft bandage contact lens, there were three reported cases with good postoperative outcomes without complications. In one case, the soft bandage contact lens was used without any adhesion or fixation while two cases involved suturing to allow fixation.[11] After vitreoretinal surgery, the bandage contact lenses were replaced with a sutured permanent allograft cornea.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1. Jain A NS, Saxena S. Keratoprosthesis in Vitreoretinal Surgery. In: Jain A NS, Saxena S, ed. Cutting-edge Vitreoretinal Surgery. 1 ed. Springer Nature Singapore; 2021:427 - 433:chap 39.
- ↑ 2. Landers MB, 3rd, Foulks GN, Landers DM, Hickingbotham D, Hamilton RC. Temporary keratoprosthesis for use during pars plana vitrectomy. Am J Ophthalmol. May 1981;91(5):615-9. doi:10.1016/0002-9394(81)90061-1
- ↑ 3.0 3.1 3.2 3.3 3. Toth CA, Landers MB, 3rd. A new wide-field temporary keratoprosthesis. Retina. 1993;13(4):353-5.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 4. Brightbill FS MP, McGhee CN, Farjo AA. Part 5: Special Situations in Corneal Surgery. In: Brightbill FS, ed. Corneal Surgery: Theory, Technique and Tissue. Mosby; 2008:677 - 681:chap 5.
- ↑ 5.0 5.1 5.2 5. DORC 1285.2 ECKARDT TEMPORARY SILICONE KERATOPROSTHESIS, TYPE II 7MM. https://oisto.com/dorc-1285.2-eckardt-temporary-silicone-keratoprosthesis-type-ii-7mm/
- ↑ 6. Eckardt C. A new temporary keratoprosthesis for pars plana vitrectomy. Retina. Spring 1987;7(1):34-7.
- ↑ 7.0 7.1 7.2 7.3 7. Gallemore RP, Bokosky JE. Penetrating keratoplasty with vitreoretinal surgery using the Eckardt temporary keratoprosthesis: modified technique allowing use of larger corneal grafts. Cornea. Jan 1995;14(1):33-8.
- ↑ 8.0 8.1 8.2 8. Kapran Z, Ozkaya A, Erdogan G, et al. Wide-Field Landers Keratoprothesis in Various Combined Corneal and Vitreoretinal Problems: Twelve-Month Results. Ophthalmic Surg Lasers Imaging Retina. Mar 1 2017;48(3):237-241. doi:10.3928/23258160-20170301-07
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9. Temporary Keratoprosthesis. https://ocularinc.com/products/vitrectomy-lenses/temporary-keratoprosthesis.html?dir=asc&limit=all&mode=list&order=price
- ↑ 10.0 10.1 10.2 10.3 10. Nardi M, Giudice V, Marabotti A, Alfieri E, Rizzo S. Temporary graft for closed-system cataract surgery during corneal triple procedures. J Cataract Refract Surg. Aug 2001;27(8):1172-5. doi:10.1016/s0886-3350(01)00748-9
- ↑ 11.0 11.1 11.2 11. Skevas C, Bigdon E, Steinhorst A, et al. A novel temporary keratoprosthesis technique for vitreoretinal surgery. Int J Ophthalmol. 2021;14(11):1791-1795. doi:10.18240/ijo.2021.11.21
- ↑ 12. Watson JS, Tran TT, Porfilio WL, Landers MB, 3rd. Maintaining a watertight globe while operating with a temporary keratoprosthesis. Retina. Jun 2011;31(6):1118-21. doi:10.1097/IAE.0b013e318203c16e
- ↑ 13.0 13.1 13.2 13.3 13.4 13. Watson JS, Tran TT, Landers MB, 3rd. The landers trunkless temporary keratoprosthesis. Arch Ophthalmol. Aug 2011;129(8):1067-9. doi:10.1001/archophthalmol.2011.189
- ↑ 14.0 14.1 14. Benner JD, Landers MB, 3rd. An infusion temporary keratoprosthesis for pars plana vitrectomy. Am J Ophthalmol. Oct 1996;122(4):579-80. doi:10.1016/s0002-9394(14)72123-3
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15. Roters S, Szurman P, Hermes S, Thumann G, Bartz-Schmidt KU, Kirchhof B. Outcome of combined penetrating keratoplasty with vitreoretinal surgery for management of severe ocular injuries. Retina. Feb 2003;23(1):48-56. doi:10.1097/00006982-200302000-00008
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16. Bove Alvarez M, Arumi CG, Distefano L, et al. Comparative study of penetrating keratoplasty and vitreoretinal surgery with Eckardt temporary keratoprosthesis in ocular trauma versus non-trauma patients. Graefes Arch Clin Exp Ophthalmol. Nov 2019;257(11):2547-2558. doi:10.1007/s00417-019-04420-0
- ↑ 17.0 17.1 17. Chen HJ, Wang CG, Dou HL, et al. Anatomical outcome of vitreoretinal surgery using temporary keratoprosthesis and replacement of the trephined corneal button for severe open globe injuries: one-year result. J Ophthalmol. 2014;2014:794039. doi:10.1155/2014/794039
- ↑ 18.0 18.1 18.2 18.3 18. Dong X, Wang W, Xie L, Chiu AM. Long-term outcome of combined penetrating keratoplasty and vitreoretinal surgery using temporary keratoprosthesis. Eye (Lond). Jan 2006;20(1):59-63. doi:10.1038/sj.eye.6701794
- ↑ 19. Khouri AS, Vaccaro A, Zarbin MA, Chu DS. Clinical results with the use of a temporary keratoprosthesis in combined penetrating keratoplasty and vitreoretinal surgery. Eur J Ophthalmol. Sep-Oct 2010;20(5):885-91. doi:10.1177/112067211002000512
- ↑ 20.0 20.1 20. Garcia-Valenzuela E, Blair NP, Shapiro MJ, et al. Outcome of vitreoretinal surgery and penetrating keratoplasty using temporary keratoprosthesis. Retina. 1999;19(5):424-9. doi:10.1097/00006982-199909000-00010
- ↑ 21.0 21.1 21. Nowomiejska K, Haszcz D, Forlini C, et al. Wide-Field Landers Temporary Keratoprosthesis in Severe Ocular Trauma: Functional and Anatomical Results after One Year. J Ophthalmol. 2015;2015:163675. doi:10.1155/2015/163675
- ↑ 22.0 22.1 22.2 22. Mayali H, Kayikcioglu O, Altinisik M, Bicak F, Kurt E. Clinical Results in Patients with Combined Penetrating Keratoplasty and Vitreoretinal Surgery Using Landers Wide-field Temporary Keratoprosthesis. Turk J Ophthalmol. Oct 24 2019;49(5):270-276. doi:10.4274/tjo.galenos.2019.87059
- ↑ 23. Cunningham ET, Adan A, Nguyen QD, Zierhut M. Tocilizumab for the Treatment of Ocular Inflammatory Disease. Ocul Immunol Inflamm. Jan 2 2021;29(1):2-5. doi:10.1080/09273948.2020.1859257
- ↑ 24.0 24.1 24. Omari A, Khan N, Tausif H, Nyalakonda R, Williams GA, Gupta C. Temporary Keratoprosthesis with Penetrating Keratoplasty in Conjunction with Pars Plana Vitrectomy for Repair of Retinal Detachments in Patients with Anterior and Posterior Segment Pathology. Retin Cases Brief Rep. Feb 1 2021;doi:10.1097/ICB.0000000000001136