Techniques for Combined Cataract and Filtering Glaucoma Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Summary
Cataract and glaucoma are the leading causes of blindness worldwide. The prevalence of both diseases is increasing with aging population. Techniques for cataract surgery have undergone significant refinements with excellent visual outcomes enjoyed by our patients. The goal of glaucoma surgery is to lower intraocular pressure to prevent or slow down the progression of optic nerve damage and associated visual field loss. Although many patients present with these concomitant diseases, there is no general consensus on surgical management of coexisting cataract in patients with glaucoma. The surgeon has to decide which approach may be best suited for a particular patient, combined surgery or staged (sequential) surgeries, depending on the patient’s severity of glaucoma and visual compromise from a cataract. This brief review will discuss indications, surgical techniques, and outcomes of various types of combined cataract and glaucoma surgery.
Combined Cataract and Glaucoma Surgery
Potential Advantages
- Patient Convenience: A single visit to the operating room maybe beneficial in terms of cost, risks of anesthesia, presence of other medical conditions precluding additional stress of multiple surgeries, environmental and social issues
- Avoid potential post-operative IOP spike which can be seen after cataract surgery, especially for cases with advanced optic neuropathy
- Long term control of IOP with glaucoma surgery and quick visual recovery from removal of a significant cataract
Potential Disadvantages
- More intraoperative and postoperative complications than with either cataract surgery or glaucoma surgery alone. Cataract surgery in patients with glaucoma may prove to be more challenging due to chronic miosis/poor pupil dilation from medications or presence of synechiae. Patients with glaucoma secondary to trauma or exfoliation syndrome may have weak/fragile zonules, which may lead to zonular dehiscence and vitreous loss. Vitreous loss may lead to failure of glaucoma surgery. More inflammation is induced with combined cases, especially with one site surgery.
- Combined procedures may be less effective than glaucoma surgery alone in controlling IOP, especially for eyes with advanced glaucomatous damage
- Longer visual recovery
Regardless of the approach, a thorough discussion with the patients regarding the potential risks, benefits, and alternatives should be done.
When to Consider Combined Surgery
Determining visual potential in patients with coexisting cataract and glaucoma can be challenging. It is often hard to discern how much the glaucoma is contributing to the reduced visual acuity. There are several approaches, which can be tried to better predict post-operative visual acuity. The Potential Acuity Meter (PAM) focuses a Snellen acuity chart on the retina to remove lenticular affects and is very useful to show overall macular potential of vision. The physician, however, must also take into account the patient’s visual field, which may be approaching fixation. For those patients with only small central fields of vision and/or a spilt fixation visual field, the idea of a filtering surgery for many Ophthalmologist raises another point of interest in the decision process, which is the possibility of “snuff-out” or loss of the remaining central vision. Snuff-out, however, usually occurs due to an intraoperative event or postoperative complication and is rarely idiopathic. A review by Costa et al. showed that approximately 6% of patients who had glaucoma with advanced preoperative visual field defects who underwent trabeculectomy had a severe reduction in their central visual acuity. Patients who lost central vision had statistically higher rates of surgical complications and higher preoperative IOPs.[1] Importantly, unexplained snuff-out was not observed. This and the previous mentioned points are important for not only judging the severity of the glaucoma, but also providing the patient with realistic expectations for post-operative visual acuity and an accurate risk-benefit ratio of the surgical options.
A patient is a good surgical candidate for cataract extraction alone when there is only mild glaucomatous damage and the IOP is well controlled on one or possibly two topical medications. Cataract extraction with a posterior chamber intraocular lens (PCIOL) can be associated with a significant IOP rise in the early postoperative course in patients with pre-existing glaucoma.[2][3]This can be due to retained viscoelastic material, increased intraocular inflammation, steroid response in an already impaired trabecular meshwork.
Physicians need to be aware that in glaucoma patients after phacoemulsification and PCIOL implantation; many studies have shown a significant rise in IOP compared to non-glaucomatous patients. It is possible that up to half of patients may have an IOP of 25mmHg or greater and the greatest asset in the care of these patients is to expect this rise and monitor IOP frequently and aggressively.[4][2][3]It is important for the physician and patient to also be aware that during the first 2 to 4 months after cataract surgery, many patients with glaucoma will have IOPs above their preoperative baseline, whereas patients without glaucoma will often have unaffected or even lower IOP as stated above. Some studies have shown that patients with pre-existing POAG can have a small drop in IOP and require fewer medications after cataract surgery but this is not common and generally is not seen until 1 to 2 years after surgery.[2][3] Regardless of the possible late post-operative IOP lowering affects, cataract surgery alone should not be relied upon in treating uncontrolled primary open angle glaucoma, but may be a treatment option in angle closure glaucoma patients.
When glaucoma is uncontrolled despite the use of maximum medical therapy and laser trabeculoplasty, when possible, the physician and patient are faced with the fact that glaucoma surgery will be required. The surgery of choice is the surgery that will control the IOP best, and most often this is a filtering operation performed alone. When a patient also has a visually significant cataract, the decision becomes more complicated. In a minority of patients it is possible that glaucoma surgery can reduce the post-operative need for IOP lowering therapy and this may improve the vision and quality of life enough to delay cataract surgery. As an alternative, the cataract can also be removed later, once the filtering bleb is functioning and tissue integrity is sound. This two-stage approach is sometimes preferred, as it has been shown that patients who underwent the two-stage procedure, had a greater percentage of long-term IOP reduction compared to those patients who underwent a combined procedure.[5] Physicians must also keep in mind that the use of anti-metabolites such as mitomycin-C at the time of combined surgery can lead to more complications such as hypotony, maculopathy, bleb leak, blebitis and possible endopthalmitis.[3] [6] [7] [8] [9]
Thus, in an eye with incipient cataract, where visual impairment is mild and the glaucoma is uncontrolled a better surgical outcome may occur with a two staged approach, all the time informing the patient that cataractogenic changes with likely accelerate after surgery and that a 5 year incidence of 87% of cataracts with noted after trabeculectomies[10], although recent studies have begun to show similar long-term IOP control with both surgical plans.[11]
The third approach for surgical care is for those patients in whom you would consider a combined procedure. In those patients, the selection and glaucoma staging is very important. Although a great amount of thought may be needed to determine the correct situation for performing a combined surgery the following situations are some in which a combined approach might be considered: (1) there is adequate IOP control but significant drug-induced side effects; (2) adequate IOP control on maximal medications but advanced glaucomatous optic atrophy; (3) IOP is only under borderline control on maximal medications; or (4) uncontrolled glaucoma on maximal medications and an urgent need to restore vision and two surgeries are not feasible nor in the patient’s best interest. When performing a single surgery the patient will only be exposed to one surgical session and as such there is less risk of IOP spikes just after surgery. This is a powerful factor when dealing with patients with advanced glaucoma and concern of loss of central vision.
Pre-operative Evaluation
Patients with both cataract and glaucoma should undergo a complete ocular examination to determine the extent of each disease that is contributing to visual deterioration. This is accomplished by careful history and clinical exam includings:
- Glaucoma Medications--How many medications is the patient on? Are there serious side effects of these medications affecting other medical issues?Is compliance an issue? Is cost an issue?
- Visual acuity—What is the patients best corrected visual acuity? What is the best potential visual acuity? Is glare an issue? How much of decline in vision is due to cataract versus glaucoma?
- Intraocular pressure—Is the IOP controlled?
- Gonioscopy - Is the angle open or closed? May require special post-operative management in cases of CACG eyes which are at increased risk for malignant glaucoma. Is there subtle angle recession?
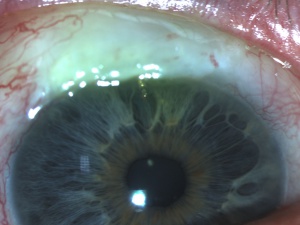
- Slit Lamp Exam-Evaluate type and extent of cataract. Is there evidence of prior trauma with iridodenesis or phacodenesis? pseudoexfoliation, or posterior synechiae? How is pupil dilation?
- Optic nerve exam and retina evaluation- How damaged is the optic nerve? Is there evidence of coexisting macular or retinal pathology that may be playing a role in decline of visual acuity and may also limit visual potential?
- Visual Field Testing—Aids in evaluation of extent of glaucoma. If a patient has central island from severe glaucoma, cataract surgery may not be beneficial in terms of visual outcome.
After careful evaluation and discussion with the patient, the decision regarding single procedure (cataract or glaucoma surgery alone) or combined surgery (combined cataract and glaucoma surgery) can be made.
Special Considerations
Poor-Pupil Dilation
Poor pupillary dilation is often seen in patients with glaucoma. This can be a result of chronic use of miotics, chronic inflammation leading to synechiae formation, chronic angle closure, prior trauma, or prior laser procedures. Patients with pseudoexfoliation, diabetes, or those on alpha-adrenergic receptor blockers may also have issues with dilation. Proper identification of these conditions prior to surgery can help plan the necessary steps that need to be taken before and during the procedure to ensure success of the case.
If the patient is on any miotics, these should be stopped before cataract surgery. The use of intracameral preservative-free epinephrine 1:10,000 may aid in pupillary dilation. Synechiae and pupillary membranes may often be broken using a cyclodialysis spatula. Once these adhesions are broken, the viscoelastic can help in further dilation. If these measures are not sufficient any of the following steps may be used:
- Sphincterotomies
- Pupil Stretching using Kuglen or Sinsky
- Mechanical dilation using iris hooks, Morcher dilating ring, or Malyugan ring
Inadequate Anterior Capsule Visualization
Inadequate anterior capsule visualization may occur in patients with corneal opacities or edema and when there is a poor red reflex as in patients with dense cataracts or in the presence of vitreous hemorrhage. In such cases the use of trypan blue can greatly aid in safely completing the capsulorhexis.
Anesthesia
Cataract surgery is now frequently performed under topical anesthesia using 2% Xylocaine jelly. Trabeculectomies are now also being performed under topical anesthesia with supplemental intracameral or subtenon injections with lidocaine or marcaine. Combined cases tend to be lengthy and can be performed using retrobulbar, peribulbar, or topical anesthesia depending on the surgeons experience and preference.
Single-Site vs. Two-Site Surgery (Cataract Extraction with Trabeculectomy)
Once the decision to do combined surgery has been made, it is up to the surgeon to decide whether to perform a single-site or a two-site surgery. Single-site surgery is done using the scleral tunnel technique. With the increasing popularity of temporal clear cornea approach for cataract surgery, two-site surgery has gained more popularity.
Single-Site Surgery Technique
Single-Site Surgery is done with the surgeon sitting superiorly. Both the trabeculectomy and cataract surgery are performed using the same conjunctival and scleral incisions.
- Superior peritomy is performed to expose bare sclera. Gentle cautery is performed as needed. Paracentesis is made either before or after the peritomy.
- If using anti-metabolites, such as 5-flourouracil (5-FU) or mitomycin-C (MMC), these may be applied using the surgeon's preferred technique.
- A partial-thickness scleral flap, hinged at the limbus is made. Alernatively, a scleral tunnel incision can be made initially, with completion of the flap after the cataract portion of the surgery using Vanass scissors
- A keratome is used to enter the anterior chamber
- Phacoemulsification is performed in the usual manner
- Intraocular lens is inserted
- Viscoelastic is removed
- Sclerectomy is performed using a Kelley descsment’s punch or wedge sclerectomy using a sharp point blade and Vanass scissors
- A peripheral iridectomy may be made if desired.
- The scleral flap is closed using interrupted or releasable 10-0 mylon sutures. These should be adjusted to ensure adequate flow.
- Tenons and conjunctiva are closed.
| Advantages of Single-Site Surgery |
|---|
|
| Disadvantages of Single-Site Surgery |
|
Two-Site Surgery Technique
In two-site surgery, the surgeon first completes the cataract extraction sitting temporally and then moves superiorly to complete the trabeculectomy.
- Temporal clear corneal cataract surgery is performed in the usual manner. It is recommended that the main incision be sutured (typically using 10-0 nylon) to prevent wound leak.
- Surgeon moves superiorly and performs trabeculectomy using his or her preferred technique.
| Advantages of Two-Site Surgery |
|---|
|
| Disadvantages of Two-Site Surgery |
|
| IOP Control with Single vs. Two-Site Surgery |
|---|
|
Post-Operative Management
Post-operative management for combined cases is similar to that for glaucoma surgery. The patient should be seen on the first post-operative day and then weekly thereafter until the IOP has stabilized. Sutures may by pulled or lysed as needed. In the presence of significant inflammation, more frequent visits may be required.
Post-operative medications
- Antibiotic drops every four hours for the first week.
- Steroid drops every 2 hours for the first month, followed by taper. Steroids may be tapered sooner following tube shunt surgery or if a concern is raised about steroid response.
- Cycloplegics may be used in cases of shallow anterior chamber or hypotony. Also beneficial in post-operative cases of CACG to prevent malignant glaucoma.
Potential Complications
Similar to the ones encountered with cataract surgery alone or trabeculectomy alone. The following list includes some of the complications encountered after glaucoma surgery. For additional information, refer to the section on Trabeculectomy.
- Shallow or flat anterior chamber
- Persistent inflammation
- Choroidal effusion
- Bleb leaks
- Persistant bleb dysthesia
- Filtration failure
- Corneal dellen
- Suprachoroidal hemorrhage
- Endophthalmitis
- Chronic hypotony
- Maculopathy
The risk of persistent hypotony and associated complications such as maculopathy, late-onset bleb leaks, infection of the bleb, and endophthalmitis may be increased with the adjunctive use of antifibrotic agents. For additional information, refer to the section on Trabeculecomy.
Other Types of Combined Surgery
Traditional combined cataract and glaucoma surgery has involved trabeculectomy. Other forms of glaucoma surgery have been increasingly combined with cataract surgery. These include:
Glaucoma drainage devices
Glaucoma drainage devices are generally reserved for complicated secondary glaucomas, such as uveitic glaucoma and neovascular glaucoma, young patients, eyes with previously failed filters, and in eyes with insufficient conjunctiva due to scarring from prior surgical procedures or injuries. These devices essentially drain aqueous out of the eye into subconjunctival reservoirs created by external plates. These devices differ in size and shape and by the presence or absence of a valve. The non-valved devices include Molteno, Baerveldt, and Shocket. The valved devices include Ahmed, Krupin, OptiMed, and Joseph. The basic surgical technique involves placement of the plate in one of the superior quadrants approximately 8 mm from the limbus, preferrably the superotemporal quadrant to avoid compression on the optic nerve, with the tube placement in the anterior chamber. Approximately, 6-8 weeks post-operatively, a fibrous capsule forms around the plate and regulates flow.
In patients presenting with both cataracts and uncontrolled glaucoma, any of these devices can be placed at the time of cataract surgery. Phacoemulsification with intraocular lens placement can be completed first. Attention is then turned to the superior conjunctiva. A peritomy is performed. The plate of the drainage implant is secured to bare sclera through the preplaced holes. A 23 or 25-gauge needle is used to enter the anterior chamber and this opening is used to place the tube into the anterior chamber (the tube may also be placed in the sulcus in pseudophakic eyes or pars plana in vitrectomized eye). The tube is secured to the sclera and covered with a patch graft. Conjunctiva is then closed. Alternatively, some surgeons prefer to secure the plate first while the eye is firm, complete cataract extraction, and then return to place the tube into the anterior chamber.
Studies have shown combined cataract and tube shunt surgery to be a safe and effective surgical option in certain clinical settings.
Ex-PRESS miniature glaucoma shunt
Ex-PRESS glaucoma shunt (manufactured by Alcon) is a biocompatible miniature stainless steel implant. It is placed beneath a scleral flap into the anterior chamber to facilitate drainage and form a bleb similar to traditional trabeculectomy. A 25 gauge needle is used to enter the anterior chamber at the gray line under the scleral flap, followed by insertion of this device. Since there is no sclerectomy or iridectomy performed, less inflammation is encountered postoperatively. This modified trabeculectomy can be combined with a cataract surgery. In a comparative case series of 345 eyes, the surgical success was reported to be 94.8% in the Ex-PRESS only group (mean follow-up: 25.7 months, range 1-46 months) and 95.6% in the Ex-PRESS combined with cataract extraction (mean follow-up:21.9 months (range 1.9-46 months). Another retrospective review found similar efficacy and safety profiles between Ex-PRESS shunt and standard trabeculectomy, although with considerable more cost when using the Ex-PRESS shunt.
Ex-PRESS Shunt in a Phakic Eye
Ex-PRESS Shunt Combined with Cataract Extraction
Photos Courtesy of Sarwat Salim, MD, FACS, University of Tennessee
Microinvasive Glaucoma Surgery (MIGS)
A number of new and evolving micro invasive strategies to provide surgical management for glaucoma patients that do not meet criteria for trabeculectomy or tube shunts are available. These are frequently combined with cataract surgery when appropriate. For more information, please visit the MIGS entry: https://eyewiki.aao.org/Microinvasive_Glaucoma_Surgery_(MIGS)
References
- ↑ Costa VP, Smith M, Spaeth GL, Gandham S, Markovitz B. Loss of visual acuity after trabeculectomy. Ophthalmology. 1993;100(5):599-612.
- ↑ 2.0 2.1 2.2 Shingleton BJ, Gamell LS, O'Donoghue MW, et al: Long-term changes in intraocular pressure after clear corneal phacoemulsification: normal patients versus glaucoma suspect and glaucoma patients. J Cataract Refract Surg 25: 885-90, 1999
- ↑ 3.0 3.1 3.2 3.3 Gimbel HV, Meyer D, DeBroff BM, et al: Intraocular pressure response to combined phacoemulsification and trabeculotomy ab externo versus phacoemulsification alone in primary open-angle glaucoma. J Cataract Refract Surg 21: 653-60, 1995
- ↑ Hayashi K, Hayashi H, Nakao F, et al. Effect of cataract surgery on intraocular pressure control in glaucoma patients. J Cataract Refract Surg 2001; 27:1779–1786.
- ↑ El-Sayyad FF, Helal MH, Khalil MM, et al: Phacotrabeculectomy versus two-stage operation: a matched study. Ophthalmic Surg Lasers 30: 260-5, 1999
- ↑ Yalvac I, Airaksinen PJ, Tuulonen A: Phacoemulsification with and without trabeculectomy in patients with glaucoma. Ophthalmic Surg Lasers 28: 469-75, 1997
- ↑ Bobrow JC: Cataract extraction and lens implantation with and without trabeculectomy: an intrapatient comparison. Trans Am Ophthalmol Soc 96: 521-56, 1998
- ↑ Storr-Paulsen A, Pedersen JH, Laugesen C: A prospective study of combined phacoemulsification-trabeculectomy versus conventional phacoemulsification in cataract patients with coexisting open angle glaucoma. Acta Ophthalmol Scand 76: 696-9, 1998.
- ↑ Gandolfi SA, Vecchi M: 5-fluorouracil in combined trabeculectomy and clear-cornea phacoemulsification with posterior chamber intraocular lens implantation. A one-year randomized, controlled clinical trial. Ophthalmology 104: 181-6, 1997
- ↑ Seah SK, Jap A, Prata JA Jr, et al. Cataract surgery after trabeculectomy. Ophthalmic Surg Lasers 1996; 27:587–594.
- ↑ Murthy SK, Damji KF, Pan Y, Hodge WG. Trabeculectomy and phacotrabeculectomy, with mitomycin-C, show similar two-year target IOP outcomes. Can J Ophthalmol 2006; 41:51–59
- Friedman DS, Jampel HD, Lubomski LH, et al. Surgical strategies for coexisting glaucoma and cataract: an evidence-based update. Ophthalmology. 2002; 109:1902-1913
- Ticho U, Ophir A: Late complications after glaucoma filtering surgery. Am J Ophthalmol 1993; 115:506-10.
- Murthy SK, Damji KF, Pan Y, Hodge WG. Trabeculectomy and phacotrabeculectomy, with mitomycin-C, show similar two-year target IOP outcomes. Can J Ophthalmol 2006; 41:51–59
- Buys YM, Chipman ML, Zack B, et al.Prospective randomized comparison of one- versus two-site Phacotrabeculectomy two-year results. Ophthalmology. 2008; 115:1130-33.
- Wyse T, Meyer M, Ruderman JM, et al. Combined trabeculectomy and phacoemulsificatin: a one-site vs a two-site approach. Am J Ophthalmol. 1998 Mar;125(3):334-9.
- Bayer A, Erdem U, Mumcuoglu T, et al. Two-site phacotrabeculectomy versus bimanual microincision cataract surgery combined with trabeculectomy. Eur J Ophthalmol. 2009 Jan-Feb;19(1):46-54.
- Borggrefe J, Lieb W, Grehn F. A prospective randomized comparison of two techniques of combined cataract-glaucoma surgery.Graefes Arch Clin Exp Ophthalmol. 1999 Nov;237(11):887-92 .
- Park HJ, Weitzman M, Caprioli J.Temporal corneal phacoemulsification combined with superior trabeculectomy: A retrospective case-control study. Arch Ophthalmol. 1997 Mar;115(3):318-23.
- El Sayyad F, Helal M, el-Maghraby et al. One-site versus 2-site phacotrabeculectmy: a randomized study.J Cataract Refract Surg. 1999 Jan;25(1):77-82.
- Joseph R. Zelefsky and Stephen A. Obstbaum. Chapter 77: Cataract and Glaucoma Surgery. In: PN. Schacknow and JR Samples, editors. The Glaucoma Book: A Practical, Evidence-based Approach to Patient Care. New York.Springer Science+Business Media, LLC 2010; 889-903.
- Hoffman KB, Feldman RM, Budenz DL, et al.Combined cataract extraction and Baerveldt glaucoma drainage implant: Indications and outcomes. Ophthalmology 2002; 109:1916-1920.
- Chung AN, Aung T, Wang JC, et al. Surgical outcomes of combined phacoemulsification and glaucoma drainage implant surgery for Asian patients with refractory glaucoma with cataract.Am J Ophthalmol 2004;137(2):294-300.
- Nassiri N, Nassiri N, Sadeghi YS, et al. Combined phacoemulsification and Ahmed valve glaucoma drainage implant: a retrospective case series. Eur J Ophthalmol 2008;18(2):191-198
- Kanner EM, Netland PA, Sarkisian S, et al. Ex-PRESS Miniature Glaucoma Device Implanted Under a Scleral Flap Alone or Combined with Phacoemulsification Cataract Surgery. J Glaucoma 2009;18(6):488-91.
- Moisseiev E, Zunz E, Tzur R, et al. Standard Trabeculectomy and Ex-PRESS Miniature Glaucoma Shunt: A Comparative Study and Literature Review. J Glaucoma 2015;24(6):410-6.