Synchysis Scintillans
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
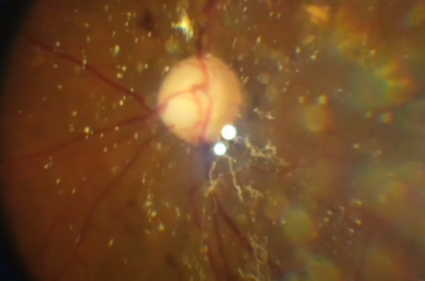
Synchysis scintillans, or cholesterolosis bulbi, is a rare degenerative ocular condition characterized by the accumulation of cholesterol crystals in the vitreous humor of the eye.[1] Cholesterol crystals appear as small, highly refractive opacities in the posterior chamber of the eye that freely move in a gravity-dependent manner, giving a snow globe-like effect.[2] There may also be anterior chamber involvement. While it is typically found in severely diseased eyes, synchysis scintillans is often an incidental asymptomatic finding.
Disease
Synchysis scintillans was first described by Parfait-Landrau in 1828[2][3][4] and was differentiated from asteroid hyalosis by Benson in 1894.[5] The naming of the condition has been a subject of contention, most notably by Potter, who in 1983 argued that the pathological designation of “cholesterolosis bulbi” is more precise than the clinical descriptor “synchysis scintillans.”[4] It is often found incidentally during posterior segment examination. On fundoscopy, yellow, highly reflective, flat, angular crystals can be seen in the vitreous humor, which has been liquefied via syneresis. Liquefaction of the vitreous results in th opacities settling inferiorly in a gravity-dependent manner when the eye is immobilized.
Synchysis scintillans is postulated to be due to a degenerative process in the vitreous. This can happen in any age group due to other ocular conditions like vitreous hemorrhage, hyphema, retinal detachment, or chronic uveitis.[6] Rarely, when the vitreous gains access to the anterior chamber (e.g., in aphakia), synchysis scintillans of the anterior chamber can also be seen.
Epidemiology
There have been few studies investigating the epidemiology of synchysis scintillans. However, there is a general consensus that it is a rare condition, occurs typically around the 3rd decade of life, can have a bilateral presentation, and there is no race predominance.[1][4][7] The incidence is approximately 0.003% with no gender predilection and seen unilaterally in 80% cases. [8]
Risk Factors
- Vitreous hemorrhage
- Diabetic retinopathy
- Chronic uveitis
- Retinal detachment
- Ocular trauma
- Hyphema
- Hypermature cataracts
- Phacolysis
- Coats disease[3][9]
General Pathology
The opacities observed in synchysis scintillans have been assessed via chromatography to be pure cholesterol.[10] The cholesterol crystals are generally larger than inflammatory cells and may settle inferiorly to form a pseudohypopyon when the eye is immobilized.[11] Although diagnosis can typically be made by fundoscopy, a vitreous biopsy or anterior chamber aspirate can be taken for crystal analysis.[11] Pathological findings reveal crystals with a rhomboidal shape with notched corners that are birefringent with polarization microscopy and stain positive to Oil-Red-O.[11]
Pathophysiology
Though the exact mechanism of synchysis scintillans is unknown, there have been multiple mechanisms proposed to explain the precipitation of cholesterol crystals out of solution in the vitreous humor. Bergandi et al reported dysregulation of superoxide dismutase and catalase enzymic activities at the vitreous base along with decreased amount of HA was significantly in patients with this entity. [12]
It is associated with advanced stage diabetic retinopathy and Coats disease and may occur after vitreous hemorrhage, chronic uveitis, retinal detachment, and ocular trauma.
Posterior Chamber Cholesterolosis
Under normal conditions, blood cholesterol concentration is much higher than vitreous cholesterol concentration. One proposed mechanism of pathogenesis of synchysis scintillans is the release of cholesterol from lysed red blood cells.[1][2][13][14] This would explain cases that are associated with vitreous hemorrhage, as the degeneration of extravascular blood releases excess cholesterol that precipitates as crystals out of solution in the vitreous.
However, this mechanism of cholesterolosis from the degeneration of blood is insufficient to explain cases of synchysis scintillans that occur without hemorrhage, such as cases of retinal detachment or hypermature cataracts.[14][15][16][17] With retinal detachment, cholesterol is hypothesized to originate from subretinal fluid that diffuses into the posterior chamber through retinal breaks.[9] In the case of hypermature cataracts, it is possible that exudative lens material leads to intraocular cholesterol crystals.[15]
Finally, intraocular inflammation has been proposed as a pathway for pathogenesis.[2] A recent study suggests that oxidative stress and lipoperoxidation are causative factors in intraocular cholesterol crystal formation.[18] Vitreous humor was obtained via pars plana vitrectomy from eyes affected by synchysis scintillans and patients with vitreoretinal disorders without synchysis scintillans.[18] Synchysis scintillans patients had significantly lower activities of catalase and Cu,Zn-superoxide dismutase, decreased hyaluronic acid, and increased 4-HNE-protein conjugate aggregation when compared to non-synchysis vitreoretinal disorder patients.[18] This suggests that redox imbalance and increased oxidative modifications in patients with synchysis scintillans plays a role in pathogenesis, potentially due to changes in the blood-aqueous or blood-vitreous barrier.[2][18]
Anterior Chamber Cholesterolosis
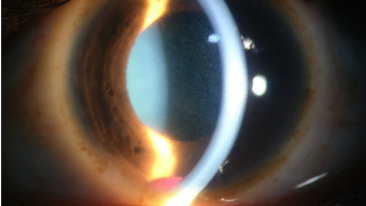
While the majority of synchysis scintillans cases are observed in the vitreous, cases of anterior chamber involvement have sporadically been reported.[1][10][13][15][19][20][21][22][23][24] Typically, anterior chamber cholesterolosis occurs with prolonged visual impairment.[17][25] It is associated with ocular insults and underlying diseases such as traumatic cataract, lens subluxation, retinal detachment, or vitreous hemorrhage.[1]
Several processes have been proposed to explain anterior chamber involvement in synchysis scintillans. Cholesterol crystals may enter directly from the vitreous via the pupillary space.[17] Lens abnormalities such as aphakia and lens subluxation may also allow the particles to pass through the atrophied iris and degenerated suspensory ligament from the posterior to anterior chamber.[13][14][19][24] Some patients present with cholesterol crystals only in the anterior chamber with a vitreous free of floaters.1,11,20,21 In these cases, it is possible that cholesterol crystals first form in the anterior chamber from proteins and fats that enter from the posterior chamber via intraocular fluid flow.[1][13][17][22][23]
Diagnosis
History
While diagnosis of synchysis scintillans is made through a clinical fundus examination, a thorough patient history is needed to identify any underlying disease processes. Synchysis scintillans is asymptomatic and not observed in healthy eyes, so the presence of vitreal cholesterol crystals indicates that there is a history of ocular disease or trauma.
Understanding epidemiology and risk factors for synchysis scintillans can help in diagnosis. The condition is associated with vitreous hemorrhage, late-stage diabetic retinopathy, chronic uveitis, retinal detachment, ocular trauma, hyphema, hypermature cataracts, and Coats disease.[3][9] It is a rare condition with unknown incidence and lack of sex or race predominance.[1][4][7] It typically presents earlier in life than asteroid hyalosis, around the 3rd decade, but can present in a patient of any age with an underlying ocular disease.[4]
Physical Examination
On fundus examination, synchysis scintillans can be observed as highly refractive vitreous opacities that are flattened, brown, or gold-colored.[2] During eye movements, the floaters are dispersed throughout the posterior chamber. When the eye is immobile, the crystals settle inferiorly in the globe in a gravity-dependent manner due to liquefaction of the vitreous. Synchysis scintillans usually affects eyes bilaterally in the posterior chamber, although anterior chamber involvement has also been reported.
While fundoscopy is usually sufficient to reach a diagnosis, complementary examinations can be used in cases of intense vitreous opacity.[2] These exams include optical coherence tomography, fluorescein angiography, and ocular ultrasound, and can help to understand more about the underlying ocular disease.[2]
Signs and Symptoms
Synchysis scintillans is asymptomatic. Patients presenting with symptoms such as decreased visual acuity or ocular pain should be evaluated for other disease or traumatic etiologies.
Clinical Diagnosis
Fundus examination with indirect ophthalmoscopy or slit lamp biomicroscopy will reveal synchysis scintillans. Appropriate follow-up of underlying pathologies such as diabetic retinopathy and retinal detachment is recommended using exams such as coherence tomography, fluorescein angiography, or ocular ultrasound.[2] Though fundoscopy is sufficient, establishment of a definitive diagnosis can be done by taking a vitreous biopsy or anterior chamber aspirate.[11] Fresh, unprocessed solution are best for pathological analysis of samples and reveal pure cholesterol crystals, rhomboidal in shape with notched corners, staining positive for Oil-Red-O and appearing birefringent with polarization microscopy.[11] Vitrectomy should not be performed for synchysis scintillans alone, since the condition is asymptomatic, and should only be done for patients with other underlying diseases where vitrectomy is indicated.
Differential Diagnosis
Synchysis scintillans must be differentiated from asteroid hyalosis, both of which are rare conditions characterized by floating opacities in the vitreous.
Asteroid hyalosis is characterized by the presence of small, yellowish-white, spherical opacities composed of lipids, calcium, and phosphorus. Classically, asteroid hyalosis presents as “stars in the night sky.”[26] This condition is usually unilateral, more common in men, and occurs in older adults over age 65. The floaters move according to ocular movement, returning to its original position after the eye is immobile, and do not settle inferiorly.[2] The density of asteroid hyalosis does not correlate with visual dysfunction; if a patient presents with significantly diminished acuity, asteroid hyalosis is not to blame, and there is likely another etiology of the symptoms.
Synchysis scintillans is characterized by small, highly refractive, gold, flattened opacities composed of pure cholesterol. This condition typically affects eyes bilaterally, has no sex or race predominance, and occurs in adult patients in a younger age demographic than asteroid hyalosis (around the 3rd decade). Unlike asteroid hyalosis, these cholesterol crystals are not suspended within the vitreous, but instead float freely in the vitreous space. When the globe moves, crystals appear in the center of the vitreous body. After immobilization of the globe, the cholesterol crystals will sink inferiorly because the crystals are not attached to the vitreal framework. A-mode images display characteristic flickering spikes from the reflections of these crystals.
Management
Uveitis or vascular work-up may be required to rule out active or lingering inflammation, which can produce vitritis. Since vitreous hemorrhage is associated with degenerative processes that can raise intraocular pressure, patients should also be monitored for glaucoma.
Treatment
Since synchysis scintillans is considered a non-progressive and asymptomatic ocular condition, treatment is usually unnecessary. However, the condition may be the result of underlying ocular diseases such as chronic uveitis, vitreous hemorrhage, retinal detachment, raised intraocular pressure, or inflammation.[27] These underlying conditions should be treated accordingly.
A therapeutic strategy which targets oxidative stress may be effective in the treatment of synchysis patients.[18] However, no pharmacological studies have been done to assess this strategy. In a case with a patient with glaucoma and cholesterolosis bulbi in both the anterior and posterior segments, pars plana vitrectomy was performed.[9] Not all of the cholesterol crystals could be removed due to a continuous influx of crystals.[9] While the vitrectomy led to successful decrease in intraocular pressure and bevacizumab injection led iris neovascularization regression, the number of cholesterol crystals did not decrease significantly.[9]
Historically, anterior segment cholesterolosis has been treated with enucleation due to intractable pain and a risk of contralateral eye involvement leading to inflammation of sympathetic ophthalmia.[9]
Prognosis
The non-progressive and asymptomatic nature of synchysis scintillans makes prognosis dependent on the underlying ocular etiology associated with the condition. Synchysis scintillans caused by phacolysis tends to have a better prognosis compared to chronically diseased eyes.[14]
Additional Resources
- Video of Synchysis Scintillans - https://www.youtube.com/watch?v=EI1ANFYsLn4
- Video of Asteroid Hyalosis - https://www.youtube.com/watch?v=UDDX5xG19dM
- Another video of Asteroid Hyalosis - https://www.youtube.com/watch?v=lNd8GaYNp6E
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Wand M, Smith TR, Cogan DG. Cholesterosis Bulbi: The Ocular Abnormality Known as Synchysis Scintillans. American Journal of Ophthalmology. 1975;80(2):177-183. doi:10.1016/0002-9394(75)90129-4
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Gonçalves M.B. (2020) Asteroid Hyalosis and Synchysis Scintillans. In: Rodrigues E., Meyer C, Tomazoni E. (eds) Trauma and Miscellaneous Disorders in Retina. Retina Atlas. Springer, Singapore. Doi:10.1007/978-981-13-8550-6
- ↑ 3.0 3.1 3.2 Kumar S. Cholesterol crystals in the anterior chamber. Br J Ophthalmol 1963;47:295-9.
- ↑ 4.0 4.1 4.2 4.3 4.4 Potter JW. Synchysis Scintillans, Cholesterosis Bulbi, and Asteroid Bodies: Does Synchysis Scintillans Exist? The Australian Journal of Optometry. 1983;66(6):232-238. doi:10.1111/j.1444-0938.1983.tb03724.
- ↑ Margo CE. Age-Related Diseases of the Vitreous. In: Cavallotti CAP, Cerulli L, eds. Age-Related Changes of the Human Eye. Aging Medicine. Humana Press; 2008:157-191. doi:10.1007/978-1-59745-507-7_8
- ↑ Brodsky MC. Synchysis Scintillans in a Child. JAMA Ophthalmol. 2015;133(7):e150793-e150793. doi:10.1001/jamaophthalmol.2015.0793
- ↑ 7.0 7.1 Mitchell P, Wang MY, Wang JJ. Asteroid hyalosis in an older population: the blue Mountains Eye Study. Ophthalmic Epidemiol. 2003;10(5):331–5.
- ↑ Das AV, Kadam Y, Tyagi M. Clinical Profile and Demographic Distribution of Synchysis Scintillans: An Electronic Medical Record-Driven Big Data Analytics From an Eye Care Network in India. Cureus. 2022 Jun 16;14(6):e25982.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Park J, Lee H, Kim YK, et al. A case of cholesterosis bulbi with second- ary glaucoma treated by vitrectomy and intravitreal bevacizumab. Korean J Ophthalmol. 2011;25(5):362–5.
- ↑ 10.0 10.1 Andrews JS, Lynn C, Scobey JW, et al. Cholesterosis bulbi. Case report with modern chemical identification of the ubiquitous crystals. Br J Ophthalmol. 1973;57(11):838–44.
- ↑ 11.0 11.1 11.2 11.3 11.4 Miller DM, Murray TG. Man has decreased vision after remote trauma. Ophthalmology times. 2003;28(2):22-.
- ↑ Bergandi L, Skorokhod OA, et al. Oxidative Stress, Lipid Peroxidation, and Loss of Hyaluronic Acid in the Human Vitreous Affected by Synchysis Scintillans. J Ophthalmol. 2019 Oct 30;2019:7231015
- ↑ 13.0 13.1 13.2 13.3 Eagle, R. C. Jr. and Yanoff, M. 1975. Cholesterolosis of the anterior chamber. Albrecht Von Graefes Arch. Klin. Exp. Ophthalmol. 193: 121–134
- ↑ 14.0 14.1 14.2 14.3 Kennedy, C. J. 1996. The pathogenesis of polychromatic cholesterol crystals in the anterior chamber. Aust. N. Z. J. Ophthalmol. 24: 267–273.
- ↑ 15.0 15.1 15.2 Brooks AMV, Drewe RH, Grant GB, Billington T, Gillies WE. 1994. Crystalline nature of the iridescent particles in hypermature cataracts. Br. J. Ophthalmol. 78: 581–582.
- ↑ Miller, A. D. and Zachary, J. F. 2017. Nervous system. pp. 805–907. In: Pathologic Basis of Veterinary Disease, 6th ed. (Zachary J. F. ed.), Elsevier, St. Louis.
- ↑ 17.0 17.1 17.2 17.3 Sano Y, Okamoto M, Hayashi M, Sato T, Maehara S, Matsuda K. Synchysis scintillans of the anterior chamber in a dog. J Vet Med Sci. 2018;80(11):1733-1736. doi:10.1292/jvms.18-0322
- ↑ 18.0 18.1 18.2 18.3 18.4 Bergandi L, Skorokhod OA, La Grotta R, Schwarzer E, Nuzzi R. Oxidative Stress, Lipid Peroxidation, and Loss of Hyaluronic Acid in the Human Vitreous Affected by Synchysis Scintillans. Journal of Ophthalmology. 2019;2019:e7231015. doi:10.1155/2019/7231015.
- ↑ 19.0 19.1 Banc A, Stan C. 2015. Anterior chamber synchysis scintillans: a case report. Rom. J. Ophthalmol. 59: 164–166.
- ↑ Forsius H. 1961. Cholesterol-crystals in the anterior chamber. A clinical and chemical study of 7 cases. Acta Ophthalmol. (Copenh.)
- ↑ Gruber E. 1955. Crystals in the anterior chamber. Am. J. Ophthalmol. 40: 817–827.
- ↑ 22.0 22.1 Sanmugasunderam S, Giligson A, Choi SB. 2003. A “sparkling” eye. CMAJ 169: 319.
- ↑ 23.0 23.1 Wand M. 1990. Cholesterolosis of the anterior chamber. Arch. Ophthalmol. 108: 780.
- ↑ 24.0 24.1 Wand M, Gorn RA. 1974. Cholesterolosis of the anterior chamber. Am. J. Ophthalmol. 78: 143–144.
- ↑ Lu P, Huang J. Ultrasound findings in a case of Eales’ disease and ocular trauma with anterior chamber cholesterolosis. BMC ophthalmology. 2020;20(1):393-393. doi:10.1186/s12886-020-01660-1
- ↑ Benson AH. Disease of the vitreous: a case of monocular asteroid hyalitis. Trans Ophthalmol Soc U K. 1894;14:101–4.
- ↑ Kumar V, Goel N, Piplani B, Raina UK, Ghosh B. Spontaneous posterior dislocation of nucleus with synchysis scintillans. Contact Lens and Anterior Eye. 2011;34(3):144-146. doi:10.1016/j.clae.2011.02.009