Surgical Management of Intumescent Cataracts
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Article Overview
Intumescent cataracts have both opacification and swelling of the crystalline lens and may be due to ocular trauma[1]. Unlike hypermature cataracts, intumescent cataracts present with prominent sectorial markings in the anterior cortex and may display a break in the capsule[2]. Performing an intact capsulorrhexis during cataract surgery is complicated by intralenticular pressure and the absence of the red reflex. These challenges can be overcome by capsular staining with Trypan blue, decompressing the liquified cortex, and utilizing anterior segment optical coherence tomography[1][2].
Disease Entity
Disease
An intumescent cataract is a complicated form of cataract with lens hydration and increased intralenticular pressure[3].
Risk Factors
Intumescent cataracts may be associated with either blunt trauma or intraocular surgery, particularly pars plana vitrectomy[1][4]. Traumatic cataracts occur in 5-10% of all ophthalmic trauma and presentation varies based on the mechanism of trauma and the integrity of the capsular bag[5],[6]. Blunt trauma may trigger intumescence with post-inflammatory plaques, while small punctures may heal and cause only local opacities[1]. Systemic conditions such as diabetes mellitus are also associated with progression to intumescence[4].
General Pathology
Intumescent cataracts appear as opacification of the crystalline lens with swelling of the lens material[1]. High intralenticular pressure, loss of lens structural integrity, and thinning of the lens capsule accompany intumescence[1][4]. Young patients with intumescence often have a softened lens nucleus, but older patients with intumescence may have an enlarged and sclerotic lens nucleus[1]. In advanced intumescence, the lens nucleus may exhibit a golden color rather than the dark brown color characteristic of an aged nucleus[1]. In either case, the opaque lens nucleus material blocks the red reflex[1].
Pathophysiology
Intumescent cataracts display abnormalities in lens epithelial cells. Dysfunction of the sodium-potassium pump leads to imbalances in electrolytes and water that cause lens opacification[7],[8]. Unique to intumescent cataracts, this Na-K pump dysfunction creates inward osmotic pressure and epithelial cell swelling[9], with subsequent cellular lysis and cataract formation[10]. Transmission electron microscopy of lens epithelial cells reveals epithelial swelling, intraepithelial vacuolization, osmotic granule extrusion from the lens epithelial cell membrane, and breaks in the longitudinal integrity of lens capsule[9][10][11]. These extrusions of the basement membrane confer tensile weakness that may lead to surgical complications[11]. Intraocular hydraulic forces may diffusely transfer the traumatic energy, rupture the capsule, and cause immediate or delayed opacification[12]. These patients are predisposed to elevated intraocular pressure and uveitis from the anomalous lens epithelial cells and capsules, as well as lens particle and protein leakage. Patients may develop phacolytic glaucoma from direct obstruction of trabecular outflow by macrophages engorged with lens protein; phacoantigenic uveitis can result from exposed lens protein, with or without elevated intraocular pressure[4].
Primary Prevention
Intumescent cataracts can be prevented by avoiding trauma via protective eyewear and by controlling blood sugar levels in diabetics[1][4].
Diagnosis
Physical Examination
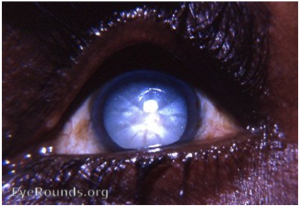
Intumescent cataracts are staged between immature cortical and mature corticonuclear cataracts. On gross appearance, an intumescent cataract will appear opaque with white crystalline lens cortex (image 1). It can be differentiated from a hypermature cataract by the presence of prominent sectoral markings in the anterior cortex, which are missing in hypermature cataracts[3].
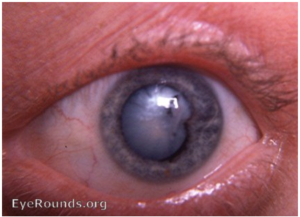
Intumescent cataracts due to physical damage or trauma may show a break in the capsule and pigment remnants on the anterior lens capsule (image 2).
Symptoms and Signs
- Blurred and dimmed vision
- Vision may be hand motion or count fingers
- Difficulty seeing in low light situations
- Halos or streaks around lights
- Loss of ability to differentiate colors
- Clouding of the lens
Diagnostic Procedure
It is important to properly diagnose and classify intumescent cataracts as surgical protocols differ from those used to treat immature cataracts. Slit lamp biomicroscopy reveals a pearly white lens with a tense anterior capsule. Anterior segment optical coherence tomography showing a lens thickness of 5.36 mm or greater coupled with a spherical lens shape indicates an intumescent cataract[13]. Scheimpflug densitometry may also be used to evaluate the opacity of the lens; a high density suggests the large nucleus more specific to intumescent cataracts[13].
Differential Diagnosis
- Hypermature Morgagnian cataract
- Mature cortical cataract
- Immature cortical cataract
- Non-intumescent White cataracts
Management
Surgical Treatment
Standard cataract surgery is a viable treatment modality for intumescent cataracts with special attention given to the anterior chamber pressure intraoperatively. Pre-operatively a complete exam and intraocular lens power calculation are performed. After standard dilation and creation of the side port incision, the anterior chamber is filled with air, trypan blue, and then a dispersive viscoelastic to flatten the anterior lens capsule.
The anterior capsule is punctured, and loose cortical material aspirated with a canula or needle to decompress the intralenticular space and flatten the anterior capsule[14]. Alternatively, phaco capsulotomy[15] may also be performed using the phaco handpiece. Either the bevel-up or bevel-down configuration of the phaco probe may be used. We prefer bevel-up for this as it directs aspiration away from the subincisional space, allowing for easier access. Using high IOP (>80mmHg) and low flow settings (can generally start with Sculpt settings and just increase IOP), briefly apply ultrasonic energy to break through the anterior capsule and into the lens. The phaco probe should then be kept in position 2 (irrigation/aspiration) to remove the liquified material. Before removing the phaco probe, dispersive viscoelastic should be injected to pressurize the anterior chamber. The remainder of the cataract surgery can then be performed.
Alternative approaches have been studied. Titiyal et al used optical coherence tomography to identify pockets of fluid intraoperatively to assist the completion of the capsulorrhexis[2]. These pockets of fluid indicate areas of raised intralenticular pressure (ILP) with an increased risk of rhexis extension. Alternatively, a two-staged continuous curvilinear capsulorrhexis can be performed by creating a mini capsulorrhexis which is secondarily enlarged[16]. Mahajan et al describe a vacuum rhexis technique using a 24 gauge needle and suction with a 10 mL syringe[17].
Post-Operative
Early post-operative evaluation assesses for rises in intraocular pressure; intraocular lens stability and capsule contracture are assessed at subsequent visits especially for cases with loose zonules[1].
Complications
Surgery is complicated by the absence of the red reflex creating poor visibility of the lens capsule in addition to lens intumescence[1]. Capsular staining is the most common technique to manage the anterior capsule; oblique illumination from a fiber optic light pipe has also been used to improve visibility[1]. Other authors have proposed phacocapsulotomy to release intralenticular fluid and reduce radial tear formation[18] [19].
A white cataract flanked by a widely split, trypan blue-stained capsule has been referred to as the Argentinian flag sign, and can be indicative of not only radial extension of the anterior capsule, but extension through the posterior capsule. This complication can occur immediately upon puncturing the anterior capsule, and can be managed by re-administration of viscoelastic and creation of the capsulorrhexis flap with horizontal forces directed centrally[20]. Complications include posterior capsule rupture, vitreous loss, zonular rupture, retained or dropped nuclear material, inability to implant the intraocular lens, prolonged surgical time, and corneal endothelial damage[19] [21].
Intumescent lenses also cause thinned, stretched, and mobile posterior capsules. The excess mobility and capsular fragility increase the risk of posterior capsule rupture[4]. These capsules also lack a protective epinucleus; dispersive viscoelastic can be injected behind the nucleus during phacoemulsification to provide an artificial epinucleus for capsular protection[4]. Lens hydration in younger patients both softens the nucleus and opacifies the cortex[4]. These nuclei may require less ultrasound for removal and no hydrodissection or hydrodelineation[4]. Capsules in younger patients may also be overstretched, hypermobile, and prone to rupture[4].
Zonular weakness or absence are more common among both elderly patients and patients with traumatic cataracts[4]. A capsular tension ring can be placed if zonular weakness is suspected but only in the presence of an intact anterior and posterior capsule[4]. Additional stability can be provided by a sutured capsule tension ring if there is severe loss of zonules[4]. A transscleral sutured intraocular lens or an anterior chamber intraocular lens are viable alternatives if the capsular bag and sulcus are not viable options[4].
Prognosis
Prognosis in intumescent cataracts is good despite the increased risk of surgical complications, uveitis, and glaucoma, with up to 92% of patients having best-corrected visual acuity of 20/40 or better at 6-weeks post procedure[22].
References
- ↑ Jump up to: 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Steinert RF. The Intumescent Cataract. In: Cataract Surgery. Elsevier; 2010:333-337. doi:10.1016/B978-1-4160-3225-0.00027-1
- ↑ Jump up to: 2.0 2.1 2.2 Titiyal J, Kaur M, Shaikh F, Goel S. Real-time intraoperative dynamics of white cataract-intraoperative optical coherence tomography-guided classification and management. J Cataract Refract Surg. 46(4):598-605.
- ↑ Jump up to: 3.0 3.1 Caccamise WC. Intumescent cataract. EyeRounds.org. Published 2008. https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/intumescent-cataract.html
- ↑ Jump up to: 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 Kim WS, Kim KH. Challenges in Cataract Surgery. Springer Berlin Heidelberg; 2016. doi:10.1007/978-3-662-46092-4
- ↑ Diego Zamora-de la Cruz, Marisol Garzón. Management of Traumatic Cataract. EyeNet Mag. Published online August 2016. https://www.aao.org/eyenet/article/management-of-traumatic-cataract
- ↑ Tsurimaki Y. Traumatic cataract. Curr Encycl Ophthalmol. Published online 1993:175-180.
- ↑ Hightower KR. The role of the lens epithelium in development of UV cataract. Curr Eye Res. 1995;14(1):71-78. doi:10.3109/02713689508999916
- ↑ Delamere NA, Tamiya S. Expression, regulation and function of Na,K-ATPase in the lens. Prog Retin Eye Res. Published online 2004:23.
- ↑ Jump up to: 9.0 9.1 Inanc M, Tekin K, Erol YO, et al. The ultrastructural alterations in the lens capsule and epithelium in eyes with traumatic white cataract. Int Ophthalmol. 2019;39(1):47-53. doi:10.1007/s10792-017-0783-0
- ↑ Jump up to: 10.0 10.1 Andjelic S, Drašlar K, Hvala A, Hawlina M. Anterior lens epithelium in intumescent white cataracts - scanning and transmission electron microscopy study. Graefes Arch Clin Exp Ophthalmol. 2016;254(2):269-276. doi:10.1007/s00417-015-3220-y
- ↑ Jump up to: 11.0 11.1 Hawlina M, Stunf S, Hvala A. Ultrastructure of anterior lens capsule of intumescent white cataract. Acta Ophthalmol (Copenh). 2011;89(4):e367-e370. doi:10.1111/j.1755-3768.2010.02102.x
- ↑ Shah MA, Shah SM, Shah SB, Patel CG, Patel UA. Morphology of traumatic cataract: does it play a role in final visual outcome? BMJ Open. 2011;1(1):e000060-e000060. doi:10.1136/bmjopen-2011-000060
- ↑ Jump up to: 13.0 13.1 Centurion V, Leal EB, Lacava AC. Image test in the sure diagnosis of intumescent white cataract. Rev Bras Oftalmol. 67(5):236-242.
- ↑ Nabil K. M. (2017). Lens decompression technique for prevention of intraoperative complications during phacoemulsification of intumescent cataract. Indian J Ophthalmol, 65(12), 1436–1439.
- ↑ Teng CC. Phaco capsulotomy: a technique to prevent the Argentinean Flag Sign. Clin Ophthalmol. 2017 Nov 6;11:1937-1940. doi: 10.2147/OPTH.S138676. PMID: 29184382; PMCID: PMC5685091
- ↑ Kara-Junior N., de Santhiago M. R., Kawakami A., Carricondo P., & Hida W. T. (2009). Mini-rhexis for white intumescent cataracts. Clinics (Sao Paulo, Brazil), 64(4), 309–312.
- ↑ Mahajan S, Gitanjli S, Garg R. Vacuum rhexis - A novel capsulorhexis technique for white cataracts. Indian J Ophthalmol. 2002 Nov;70(11):4043-4046.
- ↑ Genç S, Güler E, Çakır H, Özertürk Y. Intraoperative complications in intumescent cataract surgery using a phaco capsulotomy technique. J Cataract Refract Surg. 2016;42(8):1141-1145. doi:10.1016/j.jcrs.2016.06.025
- ↑ Jump up to: 19.0 19.1 El-Gasim M, Vinod K, Teng CC. Preventing the Argentinian Flag Sign During the Extraction of White Intumescent Cataracts: Phaco Capsulotomy Experience. Invest Ophthalmol Vis Sci. 2015;56(7):683-683.
- ↑ Little BC, Smith JH, Packer M. Little capsulorhexis tear-out rescue. J Cataract Refract Surg. 2006;32(9):1420-1422. doi:10.1016/j.jcrs.2006.03.038
- ↑ Figueiredo CG, Figueiredo J, Figueiredo GB. Brazilian technique for prevention of the Argentinean flag sign in white cataract. J Cataract Refract Surg. 2012;38(9):1531-1536. doi:10.1016/j.jcrs.2012.07.002
- ↑ Balyan M, Jain A, Malhotra C, Ram J, Dhingra D. Achieving successful capsulorhexis in intumescent white mature cataracts to prevent Argentinian flag sign - A new multifaceted approach to meet the challenge. Indian J Ophthalmol. 2021;69(6):1398. doi:10.4103/ijo.IJO_1903_20