Superior Ophthalmic Vein Thrombosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Superior ophthalmic vein thrombosis (SOVT) is a rare vision- and life-threatening complication with many underlying etiologies such as infectious and inflammatory orbital disease, trauma, neoplasm, and a hypercoagulable state. Presenting signs of SOVT are caused by venous congestion and may include painful proptosis, eyelid swelling, ptosis, impairment in motility, and vision loss.[1] [2]
Pathology
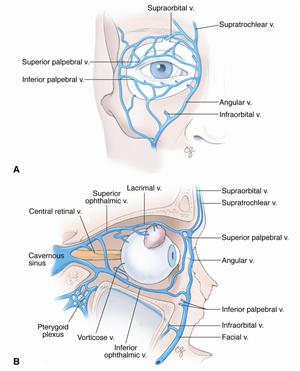
The superior ophthalmic vein originates in the superior inner angle of the orbital cavity and travels with the superior orbital artery to drain into the cavernous sinus (Figure 1). It is the vein responsible for most of the venous drainage of the orbit.[1]
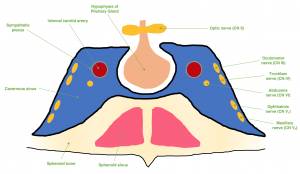
SOVT is caused by altered venous blood flow, and can be due to anatomic or systemic causes. Risk factors usually include at least one of Virchow’s triad of vascular damage, stasis, or hypercoaguability.[3] SOVT may present similarly to, or occur simultaneously to orbital cellulitis or cavernous sinus thrombosis (CST).[1][2] When SOVT develops into CST, there is subsequent involvement of the cranial nerves in the cavernous sinus along with intracranial complications resulting in cavernous sinus syndrome (Figure 2).
Etiology and Incidence
Causes of SOVT can be separated into septic or aseptic (Table 1).
Table 1: Etiology of superior ophthalmic vein thrombosis reported in the literature[1][2]
| Aseptic | Septic | ||
|---|---|---|---|
| Vascular Malformations | Dural arteriovenous fistula of cavernous sinus, carotid cavernous fistula | Sinusitis | Sphenoidal sinusitis, ethmoidal sinusitis, pansinusitis |
| Auto-immune/ systemic | Thyroid eye disease, systemic lupus erythematosus, ulcerative colitis | Orbital infections | Orbital cellulitis, dacryocystitis induced orbital cellulitis, ethmoid sinusitis |
| Trauma | Facial trauma | Dental infections | Dental infection with and without orbital cellulitis and pansinusitis |
| Hematological | Autoimmune hemolytic anemia, antiphospholipid syndrome, sickle trait, hereditary hemorrhagic telangiectasia (HHT) | Facial infections | Facial cellulitis and orbital cellulitis, masticator space abscess |
| Malignancies | Adenoid cystic carcinoma of nasal mucosa, Cavernous sinus meningioma, hypercoagulable state associated with occult malignancy | Other | Otomastoiditis, Lemierre syndrome |
| Hormonal | Oral contraceptive pill, tamoxifen, minestrine |
Aseptic etiologies reported in the literature include orbital vascular malformations (dural arteriovenous fistula, carotid cavernous fistula), autoimmune and systemic conditions (systemic lupus erythematosus, thyroid eye disease, ulcerative colitis), facial trauma, hematologic etiologies (antiphospholipid syndrome, sickle trait), orbital neoplasm, hormonal therapies (tamoxifen, oral contraceptive pill), and other assorted causes (Tolosa-Hunt Syndrome and idiopathic orbital inflammatory disease).[1][2][3][4][5][6] Often no systemic disease or coagulation disorder is found.[1]
Septic causes reported in the literature include infections of the sinuses, orbit, teeth, and face. The offending pathogens may be aerobic or anaerobic bacteria, with Staphylococcus aureus and streptococci reported as the most common causes.[3][4]Recently, cases of SOVT were also reported in association with covid-19 infection and its vaccination.[7][8]
The incidence of SOVT is not known, but is typically described as rare. A case series published by van der Poel et al. reported only 69 total cases in the literature from 1975 to 2019, with 77.8% of those cases found to be from aseptic causes.[1] A more recent study by Sotoudeh et al. in 2019 reported an additional 24 cases, 50% of which were from septic SOVT.[2]
Diagnosis
History and Physical examination
The clinical presentation of SOVT can be explained by orbital congestion due to impaired venous drainage.[1] Patients typically present with pain, chemosis, eyelid edema, ptosis, proptosis, limited ocular motility, and impaired visual acuity. Typically, the complaints will be unilateral, but if the patient has concurrent CST, they may have an onset with unilateral ophthalmic signs that rapidly become bilateral.[9] Systemic conditions may also cause bilateral involvement.[10]
Imaging
The symptoms of SOVT can overlap with orbital cellulitis and cavernous sinus thrombosis, making imaging critical for diagnosis.[2] The preferred imaging modality is contrast enhanced computed tomography (CT) or magnetic resonance (MR) angiography. Imaging can confirm a diagnosis of an isolated SOVT, or detect the presence of SOVT with concurrent cavernous sinus thrombosis and orbital cellulitis.[1][3][4]
On a contrast enhanced CT, SOVT is characterized by an enlarged superior ophthalmic vein with an indistinct outer border due to perivascular edema. A filling defect may be seen within the SOV itself, or a thin lining may be present close to the vessel wall due to either vessel wall enhancement or a lumen between the clot and the vessel.[11]
On contrast enhanced MR, there will be enhancement of intraorbital fat with edema and enhancement of the eye musculature due to venous congestion. Similar to contrast enhanced CT, MRI will show intra-luminal filling defects in the SOV. Other secondary signs such as proptosis and thickening of the extraocular muscles may be noted.[11]
Additional sequences such as diffusion-weighted imaging may be useful if contrast medium is contraindicated.[12]
Laboratory tests
If a patient presents without sepsis and low concern for orbital cellulitis or sinusitis, other underlying conditions must be considered. A thorough laboratory work up should be performed for possible underlying systemic and hypercoagulable disorders (Table 1).
Management
General treatment
Optimal therapy for SOVT is not well defined and is subject to debate. It is generally accepted that intervention should be guided by etiology, if one is found. Possible treatments may include antibiotics, anticoagulation, steroids, and/or surgery. As SOVT is rare, there have been no large-scale studies or randomized trials.
Medical therapy
Infection is a common cause of SOVT. Empiric treatment with a broad-spectrum antibiotic is recommended if there is concern for sepsis, orbital cellulitis, or cavernous sinus thrombosis.[1] Broad spectrum antibiotics, such as vancomycin and ceftazidime, can be used while awaiting culture results.[6] Some literature states antibiotics should be extended for two weeks beyond clinical resolution of an infection as often pathogens are sequestered within a thrombus.[4] There has not been a consensus on duration of antibiotic therapy.[1]
The utility of anticoagulation in isolated SOVT has not yet been established by any randomized clinical trial. The literature typically discusses anticoagulation to prevent thrombosis extension to the cavernous sinus, or when there has already been progression to cavernous sinus thrombosis.[9] If there is no absolute contraindication, it is generally accepted that systemic anticoagulation can be initiated.[3][4] A report by Weerasinghe et al. in 2016 concluded that anticoagulation is associated with reduced mortality in those with cavernous sinus thrombosis.[13] While current reports favor the use of anticoagulation, optimal dosing and duration has not been established.[1]
Systemic corticosteroids are also a controversial treatment in SOVT, and there is no aggregate evidence for it at this time.[1] If the etiology is believed to be non-infectious and more consistent with an orbital inflammatory syndrome, steroids can be considered. Steroids may aid in symptomatic improvement by relieving orbital congestion and reducing proptosis.[3][5]
Surgery
If an orbital abscess or sinus disease is found, surgical intervention is indicated to drain the primary source of infection.[9] The other role for surgery would be if orbital crowding caused optic nerve compression, such as in thyroid eye disease. In these cases, orbital decompression is important in preventing vision loss.[14]
Transfemoral thrombectomy by interventional radiology has been successful in treating cavernous sinus and superior ophthalmic vein thrombosis, but seems to be primarily employed in fulminant cases.[15]
Prognosis
The prognosis of SOVT typically depends on the underlying etiology. Early detection of SOVT is crucial to prevent progression to CST and its severe effects.[2] SOVT mostly resolves without any serious sequelae, however in some cases visual acuity may not be regained.[1]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Van der Poel NA, de Witt KD, van den Berg R, de Win MM, Mourits MO. Impact of superior ophthalmic vein thrombosis: a case series and literature review. Orbit.2018;1-7.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Sotoudeh J, Shafaat O, Aboueldahab, Vaphiades M, Soutoudeh E, Bernstock J. Superior ophthalmic vein thrombosis: What radiologist and clinician must know? European J. of Radiology Open. 2019;258-264.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Lim LH, Scawn RL, Whipple KM, et al. Spontaneous superior ophthalmic vein thrombosis: A rare entity with potentially devastating consequences. Eye (Lond). 2014;28:348-351.
- ↑ 4.0 4.1 4.2 4.3 4.4 Cumurcu T, Demirel S, Kesler S, Bulut T, Cavdar M, Dogan M, Sarac K. Superior ophthalmic vein thrombosis developed after orbital cellulitis. Semin Ophthalmol. 2013;28(2):58-60.
- ↑ 5.0 5.1 Mandic JJ, Mandic K, Mrazovac D. Superior ophthalmic vein thrombosis with complete loss of vision as a complication of autoimmune and infective conditions. Ocul. Immunol. Inflamm. 2018;26(7):1066-1068.
- ↑ 6.0 6.1 Michaelides M, Aclimandos W. Bilateral superior ophthalmic vein thrombosis in a young woman. Acta Ophthalmol. 2003;81(1):88-90.
- ↑ Antonios Bayas, Martina Menacher, Monika Christ, Lars Behrens, Andreas Rank , Markus Naumann. Bilateral superior ophthalmic vein thrombosis, ischaemic stroke, and immune thrombocytopenia after ChAdOx1 nCoV-19 vaccination.Lancet. 2021 May 1;397(10285):e11.
- ↑ Khurram R, Naidu V, Butt MF, Durnford L, Joffe M. Superior ophthalmic vein thrombosis secondary to COVID-19: an index case. Radiol Case Rep. 2021 May;16(5):1138-1143. doi: 10.1016/j.radcr.2021.02.063. Epub 2021 Mar 3. PMID: 33688386; PMCID: PMC7927642.
- ↑ 9.0 9.1 9.2 Desa V, Green R. Cavernous sinus thrombosis: current therapy. J Oral Maxillofac Surg. 2012;70(9):2085–2091.
- ↑ Rao R, Ali Y, Nagesh CP, Nair U. Unilateral isolated superior ophthalmic vein thrombosis. Indian J Ophthalmol. 2018;66(1):155-157.
- ↑ 11.0 11.1 Walker JC, Sandhu A, Pietris G. Septic superior ophthalmic vein thrombosis. Clin Exp Ophthalmol. 2002;30:144–146.
- ↑ Pendharkar HS, Gupta AK, Bodhey N, Nair M. Diffusion restriction in thrombosed superior ophthalmic veins: Two cases of diverse etiology and literature review. J Radiol Case Rep. 2011;5:8–16.
- ↑ Weerashinghe D, Luek CJ. Septic cavernous sinus thrombosis: case report and review of the literature. Neuroophthalmology. 2016;40(6):263-276.
- ↑ Sorrentino D, Taubenslag KJ, Bodily LM, Duncan K, Setfko T, Yu JY. Superior ophthalmic vein thrombosis: A rare complication of Graves’ orbitopathy. Orbit. 2018;37(3):175-178.
- ↑ Bauer J, Kansagra K, Chao KH, Feng L. Transfemoral thrombectomy in the cavernous sinus and superior ophthalmic vein. BMJ Case Rep. 2018;2018:bcr2017013571. Published 2018 Feb 7. doi:10.1136/bcr-2017-013571