Subclavian Steal Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
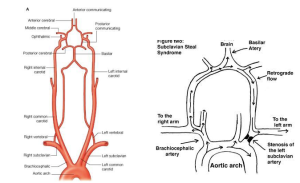
Subclavian Steal Syndrome (SSS) is characterized by a subclavian artery stenosis located proximal to the origin of the vertebral artery that leads to stealing of the blood. [1] Having SSS is quite uncommon at 2.5%. [2] The result is a pressure gradient favoring reversed blood flow (retrograde flow) in the vertebral artery distal and ipsilateral to the subclavian stenosis. [3]
In the images above, Image 1A demonstrates the blood flow in the vertebral artery when there is no subclavian stenosis. As one can note, the flow is not impeded nor is there any pressure gradient favorability. On the other hand, Image 1B demonstrates the blood flow in the vertebral artery when there is subclavian stenosis. From the image provided, the blood flow is affected. This results in retrograde blood flow in the vertebral artery or internal thoracic artery, which is due to proximal stenosis/occlusion of the subclavian artery.
General Pathophysiology
SSS develops from blood flow diversion from the vertebral artery supplying the brain to the subclavian artery supplying the arm. SSS causes symptoms of vertebrobasilar insufficiency, especially during the vigorous exercise of the arm or sudden sharp turning of the head in the direction of the affected side. The symptoms arise due to 1) lack of blood supply because of a subclavian artery stenosis or 2) rarely malformation disease. [4] Before delving into the treatment of SSS, patient education is another facet that must be discussed. There are measures that a healthcare provider can provide prior to any treatment/surgery that can benefit patients dealing with SSS. These would be secondary measures that would come after any surgical intervention.
Diagnosis
History & Physical Examination
A comprehensive history is important in determination of risk factors that could lead to SSS. [5] Subclavian artery stenosis is often asymptomatic but can present as a blood pressure difference between the arms or on ultrasound testing of patients with coronary or carotid artery disease. [6] A complete neuro-ophthalmologic exam along with a regular comprehensive history examination can be beneficial in determining if there is a lack of blood flow to certain areas of the upper extremity (head, neck, arm). Vertebrobasilar artery insufficiency can present with symptoms that include dizziness, blurring of vision, syncope, vertigo, etc. [7] SSS occurs in patients with atherosclerosis. However, there are cases of patients who manifest symptoms related to arm claudication, which consists of exercise-induced arm pain or fatigue. [8] Most patients may appear at the onset as asymptomatic but on closer observation they may present with a variety of symptoms as stated above. SSS is also a marker for atherosclerotic diseases and increased risk for cardiovascular and cerebrovascular events.
Upon ocular examination, a patient with SSS will present with impaired vision in one of the eyes. The eye that is impaired, upon examination of the fovea will have a decibel value less than zero, which will indicate that the patient is unable to see light. Furthermore, upon OCT examination the affected eye will show retinal arterial occlusion and ischemia with thinning and loss of retinal layers in the eye. This is to be expected due to the change in blood flow that has occurred due to the stenosis of the subclavian artery.
Diagnostic Work-Up
Significant subclavian artery stenosis can be demonstrated by a subclavian artery peak systolic velocity greater than 240 cm/second on ultrasound. [9] Magnetic Resonance Angiography (MRA) and CT Angiography are both diagnostic modalities that can help in the diagnosis and evaluation of subclavian artery stenosis. [10] Color Doppler ultrasound can also be complemented with either contrast-enhanced MRA or CTA. [11] As a result, based on this cut-off will indicate the severity or grade of the SSS. This will allow the healthcare provider to understand what type of treatment to provide the patient. The velocity value will vary and there is a conundrum regarding how accurate the reading would be to diagnose SSS. Other tests should be conducted to validate the claim of a patient having SSS.
Differential Diagnosis
The differential diagnosis of SSS includes Peripheral Arterial Disease (PAD) of the Upper Extremity, Posterior Circulation Stroke, Aortic Stenosis, and Diabetic Neuropathy. [12] The patient will also present with vertigo, visual changes, and weak pulse in the upper limb.
Management
Treatment
There are a variety of treatment options based on the clinical severity. The available treatment options involve medications, endovascular treatment, or surgery. [13] The 2018 European Society of Cardiology guidelines consider percutaneous balloon stenting as the preferred approach for most cases of SSS. [14] There is also work being done to utilize low-profile medical devices to treat SSS. However, it is yet to be seen how effective these devices will be in the long-term efficacy or even short-term efficacy and what population subset will be targeted.
Another promising solution is using Percutaneous transluminal angioplasty (PTA). PTA has shown to be an effective initial treatment but also has long-term benefits. PTA is recommended for individuals who have localized obstruction of the proximal subclavian artery. Compared to other treatment methods mentioned above, PTA would be highly recommended given the clinical data and trials that have been conducted.
Prognosis
SSS can be an asymptomatic or relatively benign condition. SSS however is a marker of generalized atherosclerosis and can indicate risk for future major adverse cardiovascular events like myocardial ischemia or stroke. [15] Secondary preventive measures can help with a good prognosis. Most patients (over 95%) have sustained resolution of ischemic symptoms and do not require reintervention of the target vessel. [16]
Summary
SSS is a relatively common condition that occurs in individuals. It is a phenomenon that causes retrograde flow in a vertebral artery due to stenosis or occlusion of the proximal subclavian artery. Endovascular percutaneous balloon stenting is the preferred approach for most cases, but antiplatelet medications and endovascular or vascular surgery (e.g., bypass) are also options. The prognosis for SSS is generally good but some patients can experience vertebrobasilar distribution ischemia or infarction.
References
- ↑ Psillas, G., Kekes, G., Constantinidis, J., Triaridis, S., & Vital, V. (2007, February). Subclavian steal syndrome: Neurotological manifestations. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640015/.
- ↑ William S. Fields, M. D. (1972, November 27). Joint Study of Extracranial Arterial Occlusion. JAMA. Retrieved November 1, 2021, from https://jamanetwork.com/journals/jama/article-abstract/345610.
- ↑ Potter, B. J., & Pinto, D. S. (2014). Subclavian steal syndrome. Circulation, 129(22), 2320–2323. https://doi.org/10.1161/circulationaha.113.006653
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Costa, S. M., Stott, R. C., Terry, E., & Fitzsimmons, P. J. (2007, April). Coronary-subclavian steal: Case series and review of Diagnostic and Therapeutic Strategies: Three case reports. Angiology. Retrieved November 1, 2021, from https://pubmed.ncbi.nlm.nih.gov/17495276/.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Potter, B. J., & Pinto, D. S. (2014). Subclavian steal syndrome. Circulation, 129(22), 2320–2323. https://doi.org/10.1161/circulationaha.113.006653
- ↑ Mousa, A. Y., Morkous, R., Broce, M., Yacoub, M., Sticco, A., Viradia, R., Bates, M. C., & AbuRahma, A. F. (2017, June). Validation of subclavian duplex velocity criteria to grade severity of subclavian artery stenosis. Journal of vascular surgery. Retrieved November 1, 2021, from https://pubmed.ncbi.nlm.nih.gov/28222983/.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ Song, D., Ireifej, B., Seen, T., Almas, T., Sattar, Y., & Chadi Alraies, M. (2021, July 26). Diagnosis and management of unilateral subclavian steal syndrome with bilateral carotid artery stenosis. Annals of medicine and surgery (2012). Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8329505/.
- ↑ Aboyans, V., Ricco, J.-B., Bartelink, M.-L. E. L., Björck, M., Brodmann, M., Cohnert, T., Collet, J.-P., & Czerny, M. (2018, March 1). 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). European Heart Journal. Retrieved November 1, 2021, from https://doi.org/10.1093/eurheartj/ehx095.
- ↑ Kikkeri, N. S. (2021, July 5). Subclavian steal syndrome. National Center for Biotechnology Information. Retrieved November 1, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK554599/?report=reader.
- ↑ De Vries, J.-P. P. M., Jager, L. C., Van den Berg, J. C., Overtoom, T. T. C., Ackerstaff, R. G. A., Van de Pavoordt, E. D. W. M., & Moll, F. L. (2005, January). Durability of percutaneous transluminal angioplasty for obstructive lesions of proximal subclavian artery: Long-term results. Journal of vascular surgery. Retrieved November 1, 2021, from https://pubmed.ncbi.nlm.nih.gov/15696038/.