Solar Retinopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Solar retinopathy (also known as, photic retinopathy, foveomacular retinitis, solar retinitis, and eclipse retinopathy) refers to a photochemical toxicity and resultant injury to retinal tissues, usually occurring at the fovea. This entity is commonly associated with sungazing or eclipse viewing, and often results in mild-to-moderate visual acuity deficit and/or central or paracentral scotomata. Recovery is spontaneous in nature and occurs over the course of 3-6 months after the inciting event, though visual recovery may be incomplete and patient may suffer from permanent visual acuity deficits and central or paracentral scotomata.
Disease Entity
- ICD9: 363.31 Solar Retinopathy
- ICD10: H31.029 Solar Retinopathy, unspecified eye
Disease
Solar (or photic) retinopathy refers to an entity sustained during and/or after prolonged or high intensity exposure of the foveomacular retinal tissue to light energy.
Etiology
To some degree, solar retinopathy has been recognized since the times of Classical Greece[1]. While this disease is classically associated with sungazing and eclipse viewing, a number of reports have found phototoxic foveomaculopathy to occur secondary to a myriad of other mechanisms, including from welding, ophthalmic operating microscopes[2][3], endoillumination techniques utilized during vitreoretinal surgeries[4], occupational hazards such as welding arcs[5] and laser pointers[6], and even photographical illumination mechanisms[7].
Risk Factors
Aside from sustained or high-intensity light exposure, common factors predisposing patients to phototoxic injury to the retina include[8]:
- Young age
- Clear intraocular lens
- Photosensitizing drugs: tetracycline, psoralens [5].
- Mental impairment, psychiatric disease or influence of illicit drugs [3]
Protective factors include the following[8]:
- High refractive error
- Cataract
- Darkly pigmented fundi
General Pathology
Histopathalogic analysis of rhesus monkey retinae after prolonged light exposure helped characterize the histopathologic changes observed in photoxic retinopathies. As early as day 2 post-exposure, major changes were observed mainly in the retinal pigmented epithelium (RPE). RPE disruption was evident throughout the exposed area, sometimes associated with choroidal damage. Pigmentary changes of the RPE were noted as macrophages were observed engulfing melanosomes in the subretinal space. Resolution of these findings can be seen by 10 days after injury.[9]
In 1993, ultrastructural pathologic changes of solar retinopathy were explored by Hope-Ross, et al., who had the cooperation of a 65-year-old man scheduled for enucleation for choroidal melanoma.[10] The patient agreed to stare into the sun 6 days prior to enucleation. Findings included photoreceptor changes, including vesiculation and fragmentation of photoreceptor lamellae, presence of whirls within disc membranes, mitochondrial swelling and nuclear pyknosis. RPE cells in the affected area showed plasma membrane changes, smooth endoplasmic reticulum swelling, and changes in lipofuscin granule structure.[10]
Pathophysiology
The mechanism by which retinal tissue damage occurs in solar retinopathy is photomechanical in nature. Photochemical retinal injury is believed to be a product of free radical formation. Two mechanisms of free radical formation have been proposed. First, absorption of light energy by a molecule causes an electron to enter an “excitation state”, with free radical formation being a means by which such an electron can return to the “ground state” energy level. In returning to the “ground state” energy level, an excited state electron splits a bond within another molecule, forming a free radical.[11] Second, light energy absorption can cause excitation of and direct transfer of energy from an intraretinal chromophore – flavoproteins, heme proteins, melanosomes, lipofuscin, and photoreceptors themselves – to oxygen, creating a reactive oxygen species.[11] Furthermore, the photochemical injury to the retinal tissues may be thermally enhanced[6].
Primary Prevention
Prevention of solar retinopathy is in fact the mainstay of therapy. Primary prevention of solar retinopathy includes refraining from direct sungazing or eclipse viewing.
Diagnosis
Diagnosis is made based on history and examination findings including physical/biomicroscopic examination of the fundus, as well as diagnostic imaging, such as fluorescein angiography, OCT, or fundus autofluorescence.
History
Obtaining a good history is important for making a clinical diagnosis of solar or photic retinopathy. Sungazing, eclipse viewing, occupational hazards such as welding without a welding helmet or welding goggles, exposure to lasers or laser pointers, or recent cataract extraction or other ophthalmologic operative procedures may be endorsed by the patient or may require pointed interrogation. Furthermore, cognizance on the part of the ophthalmologist of solar and other astronomical phenomena, such as solar eclipse, may aid in teasing out pertinent history from patients that raise suspicion for solar retinopathy.
Symptoms
Symptoms commonly present within hours of exposure and include blurry vision and central or paracentral blind spot in one, or more commonly, both eyes. Additional complaints may include dyschromatopsia, metamorphopsia, micropsia or frontotemporal headache
Signs
Decreased visual acuity, usually to a level of 20/25 - 20/100, but possibly worse depending on the extent of exposure.[8]
Physical Examination
A full 8-point examination should be performed on all patients presenting with visual complaints.
Fundus biomicroscopic changes tend to be bilateral, however mild cases may show no fundus abnormalities. More moderate to severe cases show dynamic fundus changes. In the first few days after injury, the fundus may display a yellow-white spot at the fovea. Subsequently, this spot may take on a more reddish hue. This red spot is often surrounded by a halo of pigment. Approximately 2-3 weeks after the injury, a small 100-200 µm lamellar hole or foveal depression can be seen. [8]
Diagnostic Imaging
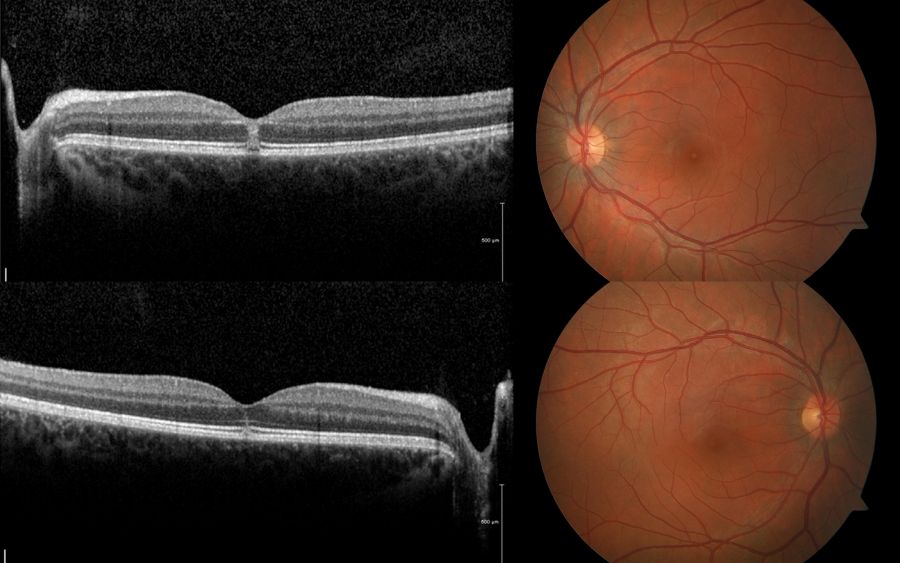
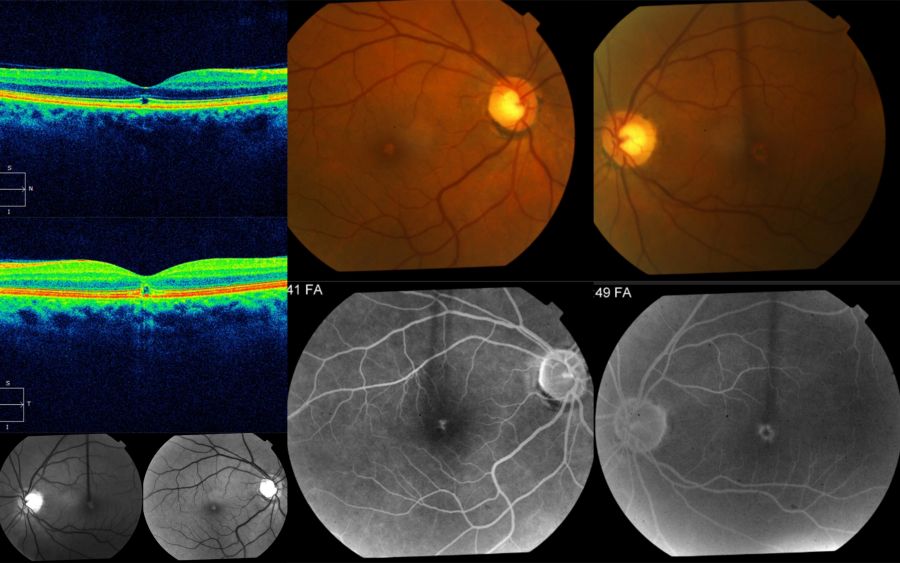
Optical Coherence Tomography
As shown below, OCT imaging in solar retinopathy usually demonstrates focal disruption of the RPE and outer retinal bands subfoveally, with an otherwise normal retinal architecture and contour. Focality of changes in the outer retinal is a common trait of this condition. When patients are examined very early (within a week), OCT may shows hyperreflective focal areas at the center of the fovea involving mostly the outer retina (but can rarely involve full thickness of the retina).
Punctate RPE transmission or window defects may be seen in fluorescein angiography due to the damage to the underlying RPE. However, these findings are not consistently seen in all cases of solar retinopathy. On fundus autofluorescence, one may notice a well-circumscribed, hypoautofluorescent central area surrounded by a ring of hyperautofluorescence.
Management
No known beneficial treatment exists for solar retinopathy, although entities such as steroids have been tried without consistent evidence of effectiveness. Prevention is through education is paramount.
Medical Follow-up
Regular follow-up through the acute phase of disease is at the discretion of the physician.
Prognosis
The bulk of visual acuity improvement has been noted to take place in the first 1 and 6 months after the photoxic event.[8][12] [13] Despite more moderate vision loss at presentation, most patients ultimately return to a visual acuity level of 20/20-20/40.[8] Improvement has been shown to be achieved earlier and more robustly in patients with visual acuity of 0.2 logMAR (20/30 Snellen visual acuity) at presentation.[14] Furthermore, a correlation was found between initial visual acuity and fundoscopic appearance 2 weeks after the phototoxic event.[14] Unfortunately, metamorphopsia and central or paracentral scotomata, including those that show some improvement initially, may become permanent.[8][13]
References
- ↑ Yannuzi LA, Fisher YL, KruegerA, et al. Solar Retinopathy: A photobiological and geophysical analysis. Tr. Am. Ophth Soc. 1987; 85:120-158.
- ↑ Michels M, Sternberg P, Operating microscope-induced retinal phototocicity: pathophysiology, clinical manifestations and prevention. Surv Ophthalmol. 1990; 34:237-252.
- ↑ Jump up to: 3.0 3.1 Long VW, Woodruff GH. Bilateral retinal phototoxic injury during cataract surgery in a child. J AAPOS. 2004; 8(3):278-9.
- ↑ Yang C, Shao D, Ding X, et al. Chronic phototoxic maculopathy caused by welding arc in occupational welders. Can J Ophthalmol. 2012; 47(1):45-50.
- ↑ Jump up to: 5.0 5.1 Michels M, Lewis H, Abrams GW, et al. Macular phototoxicity caused by fiberoptic endoillumination during pars plana vitrectomy. Am J Ophthalmol. 1992; 114(3):287-96.
- ↑ Jump up to: 6.0 6.1 Robertson DM, Lim TH, Salomao DR, et al. Laser pointers and the human eye: a clincopathologic study. Arch Ophthalmol. 2000; 118(12):1687-1691.
- ↑ Tarigopula S, Chod R. Unpublished Case. St. Louis University Eye Institute. St. Louis University, St. Louis, MO.
- ↑ Jump up to: 8.0 8.1 8.2 8.3 8.4 8.5 8.6 American Academy of Ophthalmology. "Solar Retinopathy." Section 12: Retina and Vitreous. Singapore, 2013-2014. 332-334.
- ↑ Ham, WT, Ruffolo JJ, Mueller HA, et al. Histologic analysis of photochemical lesions produced in rhesus retina by short-wave-length light. Invest Ophthalmol Vis Sci. 1978; 17(10):1029-35.
- ↑ Jump up to: 10.0 10.1 Hope-Ross MW, Mahon GJ, Gardiner TA, et al. Ultrastructural findings in solar retinopathy. Eye (London). 1993; 7:29-33.
- ↑ Jump up to: 11.0 11.1 Youseff PN, Sheibani N, Albert DM. Retinal light toxicity. Eye (Lond). 2011; 25(1):1-14.
- ↑ MacFaul PA. Visual prognosis after solar retinopathy. Brit. J. Ophthal. 1969; 53: 534-41
- ↑ Jump up to: 13.0 13.1 Rothkoff L, Kushelevsky A, Blumenthal M. Solar retinopathy: visual prognosis in 20 cases. Isr J Med Sci. 1978; 14(2):238-43.
- ↑ Jump up to: 14.0 14.1 Atmaca LS1, Idil A, Can D. Early and late visual prognosis in solar retinopathy. Graefes Arch Clin Exp Ophthalmol. 1995; 233(12):801-4.

