Seidel Test
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
History
Erich Seidel (1882-1948) was a German ophthalmologist who first described the Seidel test in 1921.
Definition
The Seidel test is used to identify full-thickness defects in the cornea or sclera by revealing leakage of aqueous humor.
Indications
- To identify an ocular leak after injury to the globe
- To determine if a corneal or scleral laceration is of full-thickness depth
- To identify a corneal perforation in the setting of infection or trauma
- To ensure appropriate wound closure intraoperatively or postoperatively
Principle
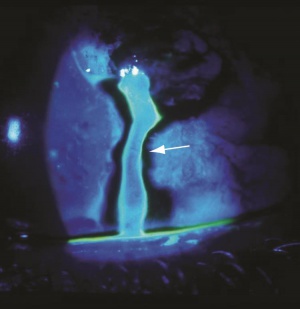
Defects in the cornea or sclera may be caused by trauma, surgery or infection. Traumatic lacerations, infectious perforations and surgical incisions are all examples of defects that can potentially violate the integrity of the globe. When evaluating a corneal or scleral defect, an assessment of it's depth is important for proper management and prognosis. Full-thickness defects of the cornea or sclera constitute an open globe injury and provide an outlet for the flow of aqueous or vitreous humor. The Seidel test is used to identify leaking aqueous during examination under cobalt blue light after instillation of fluorescein dye. When fluorescein dye is applied to the surface of the eye it appears green under cobalt blue light. Aqueous leakage from a corneal or scleral defect will dilute the dye and appear as a dark blue stream. This constitutes a positive Seidel test.
Technique
- Position the patient at the slit lamp
- Apply topical anesthetic drops
- Carefully dry the area of the suspected leak with a cellulose sponge (preferred) or cotton tip applicator
- Apply fluorescein dye to the area of the suspected leak, A fluorescein impregnated strip can be used to "paint" on the dye. Alternatively, a fluorescein drop can be instilled.
- Visualize the defect under a cobalt blue light source and evaluate for a darkened stream. The rate of flow should be noted.
- For postoperative wounds and other select cases, gentle pressure may be applied to the area adjacent to the defect to assess for flow. This must be done with extreme caution and avoided if there is any risk of expulsion of intraocular contents.
Contraindications
- Obvious globe rupture
- Hypersensitivity to fluorescein
Management
- Management of a Seidel positive defect depends on the etiology, location and size. A traumatic full-thickness laceration or perforation constitutes an open globe injury and requires prompt surgical repair. A small perforation (<2mm), or slowly leaking surgical incision may be managed with a bandage contact lens and topical antibiotic drops. Cyanoacrylate glue can also be used for small corneal defects.
Additional Resources
- Porter D, Whitman J. Slit Lamp. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/treatments/slit-lamp-2. Accessed March 25, 2019.
References
- Cain W, Sinskey RM. Detection of anterior chamber leakage with Seidel's test. Arch Ophthalmology. 1981 Nov; 99(11): 2013.