Sebaceous Carcinoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Sebaceous carcinoma is a rare, highly malignant, and potentially lethal tumor of the skin, which most commonly occurs in the eyelid. The neoplasm arises from sebaceous glands, such as those of the meibomian glands in the tarsus, the Zeis glands of the eyelashes, the caruncle, and the skin of the eyebrow. The lesion occurs more often in the upper eyelid, most likely due to the presence of a greater number of meibomian glands (~50 glands in upper eyelids, ~25 in lower).
Sebaceous carcinoma can also occur in other body areas in 25% of cases including other areas of the head and neck and other areas of skin with hair, even genitalia [1].
Muir-Torre Syndrome (MTS) is an important consideration when a patient is diagnosed with sebaceous carcinoma. MTS is an autosomal dominant condition of sebaceous tumors associated with gastrointestinal, endometrial, and urologic tumors (without any predisposing factors). The sebaceous tumors included in this syndrome are: sebaceous adenoma, basal cell epithelioma with sebaceous differentiation, and sebaceous carcinoma. Cohen et al. reported that 24% of 120 MTS patients had sebaceous carcinoma. The sebaceous carcinomas in MTS are less aggressive and less likely to metastasize than solitary sebaceous carcinoma [2].
Prevalence
A review of 5504 eyelid skin tumors by a single ophthalmologist in Switzerland from 1989-2007 showed the following:
| Benign (84%) | |
|---|---|
| Squamous cell papilloma (26%) | |
| Seborrheic keratosis (21%) | |
| Melanocytic nevus (20%) | |
| Hidrocystoma (8%) | |
| Xanthoma/xanthelasma (6%) | |
| (chalazia not included in study, #3340) | |
| Malignant (16%) | |
| Basal cell carcinoma (86%) | |
| Squamous cell carcinoma (7%) | |
| Sebaceous carcinoma (3%) |
Of note, of the 29 total patients with sebaceous carcinoma (29/5504 = 0.5%), only 1 was diagnosed clinically. [3]
Risk Factors
Periocular sebaceous carcinoma occurs more frequently in women, but extra ocular sebaceous carcinoma has been reported more in men. The upper eyelid accounts for the majority of cases. Older age is a risk factor, as the reported median age at presentation has ranged between 57 and 72 years. However, tumors can arise in younger individuals who have been treated with periocular radiotherapy. The role of immunosuppression is unclear, but solid organ transplantation increases the risk of sebaceous carcinoma [4]. In addition, other immunosuppressed states such as lymphoma may increase the likelihood of periocular sebaceous carcinoma [5].
Diagnosis
History
A high index of suspicion is critical for the diagnosis of sebaceous carcinoma. Clinical suspicion should be higher when a patient has an atypical presentation of a typical diagnosis. For example: atypical or recurrent chalazia in the upper lid, yellow thickening of the eyelid, keratoconjunctivitis or blepharoconjunctivitis unresponsive to treatment, or persistent blepharitis.
Physical examination
Sebaceous carcinoma is yellow in appearance (from the lipid within the neoplastic cells). It arises at the sebaceous glands, usually at the lid margin and can extend to the palpebral conjunctiva. Therefore, it is important to evert the lid, as seen in the third picture below.
Sebaceous Carcinoma is one of the great masqueraders--it can mimic other, more benign, lesions. It can mimic chalazia, chronic blepharitis, basal cell carcinoma, squamous cell carcinoma, superior limbic keratoconjunctivits, and ocular cicatricial pemphigoid.
The clinical diagnosis of sebaceous carcinoma is difficult. A study of 4 oculoplastic ophthalmologists in Canada examined 358 cases of periocular lesions--of which 2 were sebaceous carcinoma. The clinical diagnosis of these two lesions were: basal cell carcinoma and a vague diagnosis (e.g. lesion or mass). [6]
Symptoms
The sebaceous carcinoma mass is usually painless.
Diagnostic procedures
One of the hallmark features of sebaceous carcinoma is pagetoid spread--spreading of malignant cells to epithelium that appears to be separate from main tumor. Therefore, it is important to obtain a wide excisional biopsy of the primary lesion and map biopsies of the conjunctiva (including the palpebral conjunctiva in both lids and four quadrants of the bulbar conjunctiva). It is important to mark the margins when submitting a specimen to pathology. Communicate with the pathologist the importance of evaluating the margins for disease.
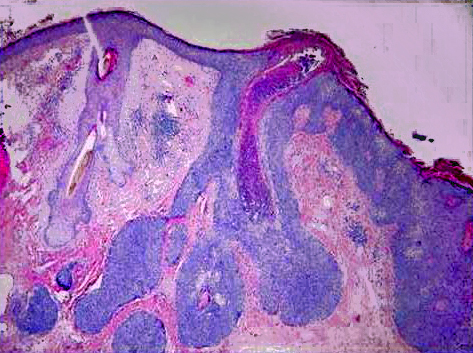
Histopathology
The histopathology varies depending on the differentiation of the tumor. In well differentiated lesions, there is a lobular arrangement and vacuolization of the cytoplasm cells centrally.
Cells present will include sebaceous and undifferentiated cells. There may be variation in nucleus shape and size with high mitotic activity indicated by mitotic figures. Special stains can be used to help distinguish sebaceous carcinoma: oil red-O, Sudan IV, epithelial membrane antigen, Leu-m1 immunostains. [1]
Below are examples of sebaceous carcinoma. The first image shows an eyelid margin with normal sebaceous glands at the inferior margin, the invasive sebaceous carcinoma, and a hair follicle in between. The 2nd and 3rd images are high power images of the carcinoma (with mitotic figures in deep purple) and normal sebaceous glands.
Differential diagnosis
The differential diagnosis includes any benign or malignant condition of the eyelid skin, including:
Benign
- Chalazion
- Blepharitis
- Seborrheic keratosis
- Actinic keratosis
- Cyst
- Squamous papilloma
- Xanthelasma
- Nevus
- Verruca
Malignant
- Basal cell carcinoma
- Squamous cell carcinoma
- Malignant melanoma
- Merkel cell tumor
- Lymphoma
- Metastasis
Management
General treatment
The mainstay of treatment is surgical excision. It is important to ensure a full thickness specimen, and to consider obtaining map biopsies of the conjunctiva. If invasive, orbital exeteration may be indicated. Staging is assessed using the TNM definitions as provided by the eight edition of the American Joint Committee on Cancer recommendations.
Surgery
Mohs micrographic surgery or complete circumferential peripheral and deep margin assessment (CCPDMA) are first line treatments for sebaceous carcinoma. Detailed history taking, age-appropriate cancer screening, and immunohistochemical staining with MLH1, MSH2, or MSH6 is helpful in identifying which patients should be referred to a geneticist for work-up of MTS.[7] Topical mitomycin or cryotherapy may improve outcomes where positive conjunctival margins exist, or in the setting of conjunctival recurrence after repeat Mohs or CCPDMA or pagetoid spread [8] .
Wide local excision may also be considered in some cases. When sebaceous cell carcinoma invades the orbit, exenteration may be considered. This is especially true for large, deeply invasive lesions, or significant bulbar conjunctival involvement. Sentinel lymph node biopsies can be considered for periocular tumors Stage T2c or higher. (T2c: tumor 10 to 20 mm in greatest dimension involving the full thickness of the eyelid) [9].
Prognosis

Sebaceous carcinoma prognosis relies on several factors, including size, location, treatment approach, and tumor stage. [11]. According to the American Joint Committee on Cancer, T category of T2b or worse correlated with regional lymph node metastasis [10]. In a recent meta-analysis of 1333 patients with eyelid sebaceous carcinoma, metastasis was reported in 12.1% of periocular cases, recurrence occurred in 15.9%, and tumor related mortality was 6.2%. [12].
Additional Resources
- http://emedicine.medscape.com/article/1101433-overview
- http://www.eyecancer.com/Patient/Condition.aspx?nID=17&Category=Eyelid+Tumors&Condition=Sebaceous+Carcinoma+of+the+Eyelid
References
- ↑ Jump up to: 1.0 1.1 Buitrago, William and Aaron Joseph. Sebaceous carcinoma: the great masquerader. Dermatologic Therapy. Vol 21, 2008, 459-466.
- ↑ Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med 1991: 90: 606-613.
- ↑ Deprez, Manuel and Uffer, Sylvie. Clinicopathological Features of Eyelid Skin Tumors. A Retrospective Study of 5504 Cases and Review of Literature. Am J Dermatopathol 2009; 31:256-262.
- ↑ Hoss E, Nelson SA, Sharma A. Sebaceous carcinoma in solid organ transplant recipients. Int J Dermatol 2017: 56: 746-749.
- ↑ Brewer JD, Shanafelt TD, Call TG. Increased incidence of malignant melanoma and other rare cutaneous cancers in the setting of chronic lymphocytic leukemia. Int J Dermatol 2015: 564: e287-e293.
- ↑ Hillson, Harvey, Hurwitz, Lie, Oestreicher, Pashby. Sensitivity and specificity of the diagnosis of periocular lesions by oculoplastic surgeons. Can J Ophthalmol 1998;33:377-83.
- ↑ Brady, K. L., & Hurst, E. A. (2017). Sebaceous carcinoma treated with Mohs micrographic surgery. Dermatologic Surgery, 43(2), 281-286.
- ↑ Owen, J. L. et al. (2019). Sebaceous carcinoma: Evidence-based clinical practice guidelines. Lancet Oncol, 20, e699-e714.
- ↑ Kibbi N, Worley B, Owen JL, et al. (2020) Sebaceous carcinoma: controversies and their evidence for clinical practice. Arch Dermatol Res. 312(1):25-31
- ↑ Jump up to: 10.0 10.1 Esmaeli B, et al (2012) American Joint Committee on Cancer T category for eyelid sebaceous carcinoma correlates with nodal metastasis and survival. Ophthal 119(5): 1078-82
- ↑ Dowell-Esquivel, C., Lee, R., DiCaprio, R.C. et al. (2024) Sebaceous carcinoma: an updated review of pathogenesis, diagnosis, and treatment options. Arch Dermatol Res 316, 55
- ↑ Desiato VM et al (2021) Sebaceous carcinoma of the eyelid: a systematic review and meta-analysis. Dermatol Surg 47(1):104–110
- Orbit, Eyelids, and Lacrimal System, Section 7. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2009.
- Ophthalmic Pathology and Intraocular Tumors, Section 4. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2009.