Revamping Physician Workflows with Device Interoperability
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Revamping Physician Workflows with Device Interoperability
Areeba Abid, BS, Sally Baxter, MD, MSc, Thomas Hwang, MD, April Maa, MD
In the Middle Ages, merchants from across Europe, the Middle East, and Africa traveled to exchange goods and ideas, coming across people and cultures very different from their own. How did traders from three different continents communicate well enough to conduct business? They developed a shared language. No matter where they came from, these traders all understood a common vocabulary to allow them to communicate certain kinds of information, like dates, quantities, and prices. This is the origin of the term ‘lingua franca’: a standard language adopted when native languages differ.[1]
Flash forward to the modern era, where the vast majority of information transfer happens not between humans, but between computers. And just as humans speak in different languages, computer systems have different languages as well. When information is stored in one language on one software system, and another language on a different system, these systems are unable to communicate with one another.
In the daily practice of ophthalmology, these technological communication barriers are very prevalent. In your practice, you likely rely on many different devices, each storing a treasure trove of patient data, all running on different software systems. For example, your patients’ charts are managed in an EMR. Their visual field data is collected and stored on a separate machine with its own software system. And their OCT reports are on another device and yet another software system. If each of these systems speak different languages, they can’t easily “communicate”, or share their data, with each other.
This inability of devices to connect with each other, or their lack of “interoperability”, presents a myriad of hurdles throughout an ophthalmologist's daily workflow. Imagine your patient had a fundus photo done at a different office, and you want to visualize the data on your own system; it may be impossible to import the original data from the other office’s device to your own. So you end up settling for lower resolution data, like paper reports (Figure 1).
Even care coordination within your own practice can be clunky, requiring logging into many separate systems to access one patient’s data across devices. A lack of information flow across systems means that technicians have to manually type in patient names when they image them on a device, leading to transcription errors; a patient’s data may end up accidentally being split across multiple records. When OCT and VF data can’t be easily imported into progress notes, they end up being manually transcribed. The original data exists in a neighboring machine, so close and yet frustratingly time-consuming to move over. This manual transcription that so many clinicians must do daily is not only inefficient and a poor use of providers’ time, but also inevitably leads to inaccurate documentation and worse patient outcomes. It becomes possible to even inadvertently have the wrong patients' data open across different viewing systems, presenting a patient safety issue; in the worst case scenario, we might inadvertently make clinical decisions for a patient based on another patient’s data!
The inefficiencies and clunkiness of the ophthalmology workflow may seem like small problems in the grand scheme of things. But all of these issues could be simply avoided if our devices were interoperable and could easily connect with each other. If traders in flea ridden 15th-century markets could develop a shared language to communicate, then the state-of-the-art devices we use in 21st century ophthalmology should be able to communicate as well. Rather than accepting inefficiency and low-resolution information transfer as the status quo, we should push for solutions that allow our modern devices to be smoothly integrated.
This is where “data standards”, like lingua francas for digital information, become useful. They allow communication across devices and organizations seamlessly, without the need for creating additional interfaces to connect devices. These digital lingua francas are already commonplace in other industries. Any mobile phone, irrespective of its manufacturer, can message another using SMS, a standard messaging system. Any bank can send money to another bank across the world using ISO financial standards.
Many well-accepted data standards have been successfully implemented in medicine too, improving patient care and clinician workflows. For example, in the 1980s, radiologists realized they needed to be able to visualize imaging from different machines side by side. They developed a data standard called DICOM (Digital Imaging and Communications in Medicine), which enabled the effortless radiology workflows that exist today: a CT scan performed by a machine made by Company A can be easily visualized on software made by Company B, and connected directly to an EMR made by Company C. DICOM is just one of many examples of data standards and interoperability revolutionizing clinician workflows. Before these standards were created, this interoperability wasn’t feasible. Many practicing radiologists today have never even seen a hard copy of an X-ray, let alone been forced to rely on grainy, manually uploaded, photocopies of X-rays. However, this is still the status quo in ophthalmology imaging, with fundus images, OCTs, and VFAs often only accessible as 2-dimensional black and white reports, lacking the depth and interactivity of the original data.
This is because many ophthalmic imaging vendors have not fully adopted data standards in the way that general radiological imaging vendors have[2]. Vendors have traditionally argued that there is a lack of consumer demand. With this in mind, practicing ophthalmologists should advocate for the same level of interoperability that our radiology colleagues enjoy. Another challenge is that established data standards are not perfectly designed for our unique ophthalmology use cases; we haven’t fully updated our lingua franca for medical data to accommodate the sharing of fundus images, OCTs, and VFAs. We need medical data standards to be expanded to include more advanced ophthalmologic data, because those data standards are the foundation for smooth device interoperability in our offices. Fortunately, this is slowly changing. Data standards, like Fast Healthcare Interoperability Resources (FHIR) will be helpful for connecting data from various sources, including data in mobile health apps and other devices, like home tonometers, with the rest of a patient’s EHR and imaging data, improving patients’ engagement with their care and care coordination.
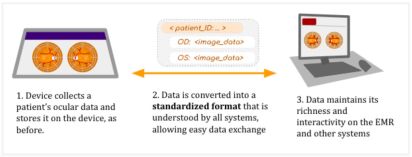
What would a modern, interoperable workflow look like? Imagine being able to sync all of a patient’s data directly on one interface, rather than scattered across several devices and proprietary viewing systems. Imagine never having to export test results as simplified PDFs or printouts ever again, and being able to interact with the original data on any machine. Imagine never having to manually transcribe test results into notes, with your devices communicating directly instead. With the adoption of data standards, this will become possible (Figure 2).
Interoperability doesn’t just offer radical improvement of our workflows; it also unlocks enormous potential for innovation. When medical data is no longer trapped on individual machines, but instead can be conveniently pooled and aggregated, researchers have access to larger, more diverse, and more useful datasets. These datasets can enable analysis of healthcare disparities across populations, allowing us to identify underserved patients and address gaps in care[3]. They can also improve the feasibility, usability, and future potential of artificial intelligence algorithms, which need to be able to tap into information stored across different systems on-demand[4]. For example, an algorithm calculating a patient-specific intravitreal injection frequency for wet AMD would need access to OCT data, vision, smoking history, etc to make reliable predictions; an AI algorithm can’t tap into those data stores to calculate risk or predictions for the clinician if the data can’t be shared across systems or pooled into a single, common dataset (Figure 3). Interoperability would enable this, streamlining our workflows, allowing for meaningful multi-site research, and enabling us to leverage the power of big data.
The implementation of data standards and interoperability has the potential to revolutionize our daily clinical practices. A modern, highly interoperable workflow minimizes errors and inefficiency, leading to improved patient outcomes. It allows for multi-device display on a single screen, which improves clinical decision making and efficiency. It eliminates tedious data transcription, improving clinician wellness and job satisfaction. It reduces burnout and maximizes the joy in patient care. The establishment of data standards is an essential step to bringing ophthalmology into the 21st century. When we understand what data standards and interoperability can do for us, we can start realizing this future.
Additional Resources
- IHE Eye Care. IHE International. https://www.ihe.net/ihe_domains/eye_care/ Accessed July 20, 2023.
References
- ↑ Mufwene, S. Sangol (2022, August 31). Lingua franca. Encyclopedia Britannica. https://www.britannica.com/topic/lingua-franca
- ↑ Lee AY, Campbell JP, Hwang TS, Lum F, Chew EY; American Academy of Ophthalmology. Recommendations for Standardization of Images in Ophthalmology. Ophthalmology. 2021 Jul;128(7):969-970. doi: 10.1016/j.ophtha.2021.03.003. Epub 2021 Apr 5. PMID: 33832778; PMCID: PMC8335850. https://pubmed.ncbi.nlm.nih.gov/33832778/
- ↑ Baxter SL, Nwanyanwu K, Legault G, Lee AY. Data Sources for Evaluating Health Disparities in Ophthalmology: Where We Are and Where We Need to Go. Ophthalmology. 2022 Oct;129(10):e146-e149. doi: 10.1016/j.ophtha.2022.06.035. Epub 2022 Sep 1. PMID: 36058733; PMCID: PMC9509471. https://pubmed.ncbi.nlm.nih.gov/36058733/
- ↑ Baxter SL, Lee AY. Gaps in standards for integrating artificial intelligence technologies into ophthalmic practice. Curr Opin Ophthalmol. 2021 Sep 1;32(5):431-438. doi: 10.1097/ICU.0000000000000781. PMID: 34231531; PMCID: PMC8373825. https://pubmed.ncbi.nlm.nih.gov/34231531/