Retinal Manifestations of Leukemia - Leukemic Retinopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction:
Ocular involvement of Leukemia is relatively common and vital to assess for as ocular symptoms may be the first indication of manifestation, relapse, or early worsening of the condition. In particular, Leukemic Retinopathy is the most common ocular manifestation of Leukemia. [1]
Disease Entity:
• Leukemia is a myeloproliferative disorder caused by an abnormal proliferation of immature leucocytes. Intraocular involvement in leukemia can be up to 90%.
• Both acute and chronic leukemia can cause ocular manifestations.
• Retina is the most common ocular tissue to be involved in leukemia.
• Leukemic retinopathy was first described by Liebriech in 1861 [2]
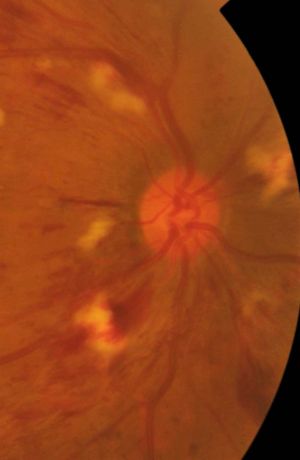
• Retinal manifestations are usually due to indirect complications of leukemia especially due to hematological abnormalities (Figure 1)
Pathophysiology:
Ocular complications of leukemia can either be [3][4]:
1. Primary or Direct due to infiltration of the orbit, iris, choroid, optic nerve, and other tissues by leukemic tumour cells
2. Indirect/ Secondary
- Hematological abnormalities such as anemia and thrombocytopenia, leading to intraretinal hemorrhages, white-centered retinal hemorrhages, cotton-wool spots, macular hemorrhages, subhyaloid hemorrhages, and vitreous hemorrhages.
- CNS involvement through infiltration of the optic nerve, causing papilledema due to high intracranial pressure, and cranial nerve palsies.
- Opportunistic infections
- Chemotherapy related; high doses of glucocorticoids can cause ocular hypertension, cataracts, diplopia, and various other disorders.
Pathogenesis: [5]
Leukostasis Retinopathy:
Prolonged leukocytosis increased number of circulating platelets --> Increased whole blood viscosity --> Reduced blood flow and vascular stagnation --> Peripheral capillary dropout and microaneurysm formation --> Proliferative retinopathy
Systemic History:
• History of leukemia or any other malignancies- acute/chronic
• History of any other systemic illnesses
• History of treatment such as chemotherapy
Ocular History:
• Visual loss - Onset, Duration
• Unilateral/bilateral
• Floaters
• Visual field defects
Signs: [3]
1. Dilated and tortuous veins – early manifestations due to hematological disturbances [6]
2. Retinal hemorrhages at all levels – especially in the posterior pole, and extension to the vitreous
• Preretinal hemorrhages
• Superficial hemorrhages
• Dot and blot hemorrhages
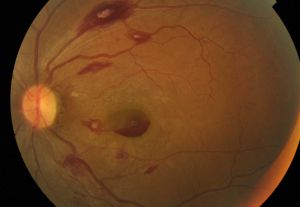
• White centered hemorrhages/ Roth Spots (Figure 2)
• Sub-ILM hemorrhages
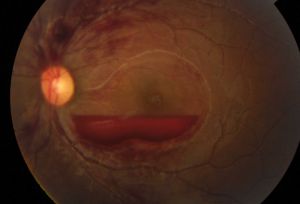
• Subhyaloid hemorrhage (Figure 3)
• Vitreous hemorrhage
ROTH SPOTS [7] (Figure 2)
White centered hemorrhages known as ‘Roth spots’ result from retinal capillary rupture and extrusion of whole blood. This is followed by platelet adhesion to the damaged endothelium initiating a coagulation cascade and formation of a white lesion in the centre of the hemorrhage which is a platelet-fibrin thrombus. In leukemia, the white centre could correspond to an accumulation of leukemic cells.
3. Cotton wool spots (Figure 4)
Secondary to clusters of cells occluding retinal arterioles, not usually associated with hematological parameters
4. Leukemic Infiltrates:
• It is generally associated with high blood counts, fulminant disease and early mortality.
• Usually, but not always seen with surrounding hemorrhage [8]
• Grey-white streaks along vessels caused by local perivascular infiltrates.
• Large grey, white nodules of varying sizes in the retina.
• Subretinal infiltrates- referred to as subretinal hypopyon
• Optic nerve infiltration
• Choroidal infiltrates – Serous retinal detachments, RPE detachments, discrete choroidal masses
• Vitreous infiltrates: Internal limiting membrane acts as an effective barrier for leukemic cells infiltration. But they can rarely invade the vitreous from the optic disc. Can be associated with vitreous hemorrhage. [8]
5. Vascular occlusions- Bilateral CRVO due to hyperviscocity (Figure 5)
6. Peripheral Microaneurysms- due to viscosity of elevated WBC count, does not correlate with hemoglobin or platelet level
7. Peripheral neovascularization similar to sickle cell anemia seen in CML- capillary closure associated with chronic elevated WBC count causing focal ischemia
8. Retinal detachments
9. Vitreous infiltrates
10. Choroidal infiltrates
11. Opportunistic infections – CMV retinitis, Ocular toxoplasmosis, Viral retinitis
12. Optic nerve involvement
13. Occular Hypertension [1]
Diagnosis:
- History of leukemia
- Detailed fundus evaluation
- Laboratory tests
- Complete blood count – to look for anemia, thrombocytopenia, pancytopenia
- Peripheral blood smear- for blast cells
- Bone marrow biopsy – infiltration by blast cells
- Flow cytometry and immunophenotyping
Management:
Patients should be treated for the underlying leukemia by chemotherapy, immunotherapy or radiotherapy. While there is no direct curative treatment for leukemic retinopathy, such approaches can help diminish the systemic disease. Chemotherapy is the primary treatment modality and depends on the type of leukemia, as well as the phase of progression. ALL treatment consists of various combinations of vincristine, prednisone, and L-asparagine, while AML is treated with Daunorubicin, cytarabine, and thioguanine. CML on the other hand, is initially treated with busulfan or hydroxyurea. If chemotherapy fails to diminish intraocular leukemic infiltrates, direct radiation therapy is recommended. Leukopheresis and allogeneic bone marrow transplant are also sometimes necessary depending on severity and disease progression. [9]
As traditional systemic treatment approaches may have limited penetrance into the vitreous, intravitreal injections have recently been explored as adjunctive treatments. Specifically, intravitreal injections of dexamethasone, anti-vascular endothelial growth factor, and methotrexate are being examined. One retrospective cohort study on 11 eyes treated with methotrexate injections showed improvement in inflammatory reactions and tumor cell infiltration in all treated eyes. Although retinal hemorrhages were not resolved, there was considerable improvement of other symptoms suggesting such approaches may be beneficial. [10]
Prognosis:
The 5-year survival rate was found to be significantly lower in those with leukemic retinopathy on presentation than in those without ophthalmic involvement (21.4% vs. 45.7%).
Patients with clinical leukemic retinopathy may have more aggressive systemic disease that might lead to a worse prognosis. [11]
References:
- ↑ 1.0 1.1 de Queiroz Mendonca, C. et al. Ocular manifestations in acute lymphoblastic leukemia: A five-year cohort study of pediatric patients. Leuk. Res. 76, 24–28 (2019).
- ↑ Liebreich: Atlas, 1863, as quoted inW.S. Duke-Elder Text-book of Ophthalmology vol. III, Mosby, St Louis (1941), Article 2740
- ↑ 3.0 3.1 Sharma T, Grewal J, Gupta S, Murray PI. Ophthalmic manifestations of acute leukaemias: the ophthalmologist's role. Eye. 2004 Jul;18(7):663-72.
- ↑ Reddy, S. C. & Jackson, N. Retinopathy in acute leukaemia at initial diagnosis: correlation of fundus lesions and haematological parameters. Acta Ophthalmol. Scand. 82, 81–5 (2004).
- ↑ Rosenthal AR. Ocular manifestations of leukemia: a review. Ophthalmology. 1983 Aug 1;90(8):899-905.
- ↑ Ballantyne AJ, Michaelson IC. Textbook of the Fundus of the Eye. Williams and Wilkins: Baltimore, 1970; 290–292.
- ↑ Allen RA, Straatsma BR. Ocular involvement in leukaemia and allied disorders. Arch Ophthalmol 1961; 66: 490–508.
- ↑ 8.0 8.1 Kuwabara T, Aiello L. Leukaemic military nodule in retina. Arch Ophthalmol 1964; 72: 494–497.
- ↑ Lihteh Wu, M. D. (2020). Ophthalmologic manifestations of Leukemias Treatment & Management: Medical Care, Consultations. Ophthalmologic Manifestations of Leukemias Treatment & Management: Medical Care, Consultations. Retrieved from https://emedicine.medscape.com/article/1201870-treatment.
- ↑ Vishnevskia-Dai, V., King, S. S., Lekach, R., Fabian, I. D., & Zloto, O. (2020). Ocular manifestations of leukemia and results of treatment with intravitreal methotrexate. Scientific reports, 10(1), 1-7.
- ↑ Retina E-Book: 3 Volume Set By Charles P. Wilkinson, David R. Hinton, SriniVas R. Sadda, Peter Wiedemann, Stephen J. Ryan