Retinal Hemifield Slide Phenomenon
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
The retinal hemifield slide phenomenon occurs when heteronymous hemianopic defects result in visual fields that can not be easily fused and therefore disassociate from one another, causing a nonparetic diplopia. Physiologically, nasal and temporal visual fields overlap between the right and left eyes and allows corresponding retinal points to be established. Fusion allows the two images, one from each eye to be combined into one coherent image.[1][2] Heteronymous hemianopic defects disrupts this fusion due to the absence of right and left visual field overlap and makes maintaining stable orthotropia difficult.[3] Manifestation of horizontal or vertical tropia/phoria causes the hemifields to slide horizontally or vertically respective to one another, resulting in diplopia.[1][3]
Etiology
The retinal hemifield slide phenomenon produces the visual symptom of diplopia resulting from concurrent heteronymous hemianopia and an underlying tropia/phoria. Bitemporal hemianopia is the most commonly associated visual defect with the retinal hemifield slide but the phenomenon can occur with any heteronymous hemianopic defects including heteronymous altitudinal defects (defects that respect the horizontal meridian) and binasal hemianopia.[1][4] Retinal hemifield slide phenomenon due to bitemporal hemianopia is mainly caused by masses or lesions localized at the optic chiasm.[5] In contrast, the retinal hemifield slide phenomenon due to heteronymous altitudinal visual field defects is localized to pathologies of the retina or optic nerve, such as optic neuritis and AION.[4] Thus, depending on the visual field defect involved, the retinal hemifield slide phenomenon could indicate pathologies at vastly different locations in the visual pathway. In addition, this phenomenon is described as a “nonparetic diplopia” since it is not due to restriction or paralysis of the extraocular muscles unlike other causes of diplopia.[1][6]
Bitemporal Hemianopia
The optic nerve fibers of the nasal retina (corresponding to temporal visual fields) decussate at the central optic chiasm. Therefore, lesions at the optic chiasm can result in bitemporal hemianopias.[7][8] Pituitary macroadenoma is one of the most common causes of this visual defect due to the pituitary gland’s adjacency to the optic chiasm.[8] However, other suprasellar masses such as Rathke cleft cyst, craniopharyngiomas, suprasellar meningiomas, and internal carotid artery aneurysms can also cause bitemporal hemianopias and the retinal hemifield slide phenomenon.[8][9][10][11] While chiasmal strokes are rare due to collateral circulation by the Circle of Willis, they can also cause acute bitemporal hemianopia.[8][12]
Heteronymous Altitudinal Visual Field Defect
Visual field defects that respect the horizontal meridian are associated with defects of the retina or optic nerve. There are rare case reports of non-arteritic ischemic optic neuropathy (NAION) and glaucoma causing heteronymous altitudinal visual field defects and resulting retinal hemified slide phenomenon.[4]
Binasal Hemianopia
Unlike bitemporal hemianopia, which is classically localized to the optic chiasm, true binasal hemianopia is rare and can not be localized to the chiasm typically. More common etiologies include bilateral glaucomatous damage, ischemic, inflammatory, compressive or other optic neuropathies.[1][13][14]
Ocular Manifestations
Ocular manifestations depend on the type of heteronymous hemianopia as well as the accompanying tropias (e.g., exotropia, esotropia, hypertropia, hypotropia).[1][2][3] Ocular deviations occur when a patient’s pre-existing phoria decompensates into a tropia due to fusional dysfunction between the eyes.[7] Patients with the retinal hemifield slide phenomenon may complain about a range of ocular manifestations including “doubling” strip of central vision, “missing” strip of central vision, or visual hemifields “sliding” respective to one another.[1][7]
Bitemporal hemianopia and deviations
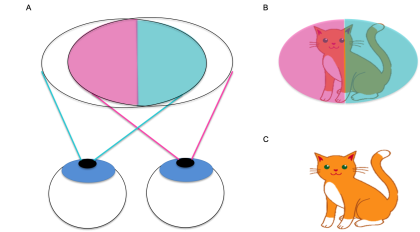
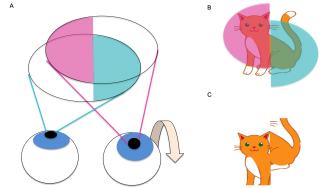
In bitemporal hemianopia, each eye has a loss of its temporal field of vision. With binocular vision, the impaired temporal visual field of each eye is partially compensated for by the contralateral eye’s intact nasal visual field (Figure 1, 2).[3] However, objects located beyond the fixation point are not visualized due to it falling in the impaired temporal fields of both eyes (post-fixational blindness).[2][7][8] Thus, patients with bitemporal hemianopia may complain of difficulty in depth perception.[3]
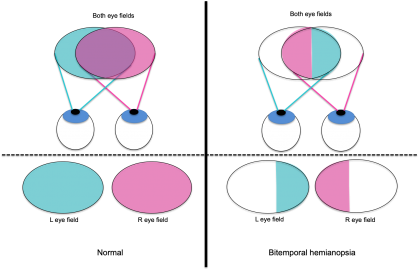
Figure 1. Left: Individual and combined visual fields of left eye (indicated in blue) and right eye (indicated in pink) in a patient with no visual field defects. Area of overlap between the right and left eye visual fields is indicated with purple. Right: Individual and combined visual fields of left eye (indicated in blue) and right eye (indicated in pink) in a patient with bitemporal hemianopia. Note the lack of overlap between the right and left eye visual fields.
Figure 2. A) Visual field of both eyes with bitemporal hemianopia (left eye visual field indicated in blue, right eye visual field indicated in pink) B) Intact visual fields of an object (cat) at the point of fixation C) Image seen by the patient with binocular vision. The impaired nasal field of each eye is compensated for by the intact temporal field of the other eye.
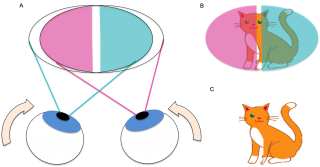
With an accompanying esotropia (or esophoria), the eye(s) deviate inwards horizontally and their corresponding intact nasal fields move away from one another, resulting in the central strip of vision falling on the impaired temporal hemifield of each eye (Figure 3A, 3B). Thus, the resulting image that the patient sees has a “missing” vertical central strip (Figure 3C).[1][2][3][7] However visual acuity is not dramatically affected like in other conditions that result in central visual field loss (e.g.. macular degeneration) because objects that fall in the region of the blind strip become visible with small movements of the eye.[7]
Figure 3. . A) Visual field of both eyes with bitemporal hemianopia and esotropia (left eye visual field indicated in blue, right eye visual field indicated in pink). Note the inward deviation of both eyes. B) Visual fields of an object (cat) at the point of fixation. There is a central vertical strip that does not fall onto either eye’s visual fields C) Image seen by the patient with binocular vision. The central strip of vision is missing.
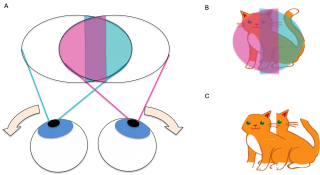
Figure 4 A) Visual field of both eyes with bitemporal hemianopia and exotropia (left eye visual field indicated in blue, right eye visual field indicated in pink, overlapping visual field indicated in purple). Note the outward deviation of both eyes. B) Visual fields of an object (cat) at the point of fixation. There is a central vertical strip that falls onto both the right and left visual fields. C) Image seen by the patient with binocular vision. The central strip of vision is duplicated, manifesting as a horizontal diplopia.
With an accompanying exotropia (or exophoria), the eye(s) deviate outwards horizontally and their corresponding intact nasal visual fields become superimposed upon one another (Figure 4A).[3][7] The central vertical strip of vision falls on the intact nasal field of both the right and left eyes (Figure 4B). Due to lack of retinal correspondence between the eyes, the central strip of vision is registered to be at different points in space between the right and left eye. The resulting image manifests as a diplopia without confusion, where there is a “doubling” of the vertical central strip (Figure 4C).[1][3][7]
Figure 5 A) Visual field of both eyes with bitemporal hemianopia and hypertropia of right eye (left eye visual field indicated in blue, right eye visual field indicated in pink). Note the upward deviation of the right eye. B) Visual fields of an object (cat) at the point of fixation. The visual field of the right eye is shifted upwards so the corresponding half of the object is perceived to be in a different location in space vertically compared to the half seen by the left eye. C) Image seen by the patient with binocular vision. The left half of the object (perceived by the intact temporal field of the right eye) is displaced downwards compared to the right half of the object (perceived by the intact temporal field of the left eye).
In hypertropia (or hyperphoria) and hypotropia (or hypophoria), the eye deviates upwards or downwards, causing the visual hemifields to “slide” vertically respective to one other (Figure 5).[1][2][7]
Heteronymous Altitudinal Visual Field Defect and Deviations
Heteronymous altitudinal visual field defects comprises of a superior hemifield defect in one eye and a inferior hemifield defect in the other.[4] Similar to bitemporal hemianopia, the presenting ocular manifestation is dependent on the type of tropia involved. However unlike bitemporal hemianopia, the retinal hemifield slide phenomenon will involve “missing” or “doubling “ of the horizontal central strip and “sliding” of the superior and inferior hemifields.[4]
In a hypertropia of the eye with the intact superior hemifield, the intact visual fields become superimposed, resulting in a “doubling “of the central horizontal strip of image. Hypotropia of the eye with the intact inferior hemifield will also result in a similar ocular manifestation.[4]
In a hypotropia of the eye with the intact inferior hemifield or a hypertropia of the eye with the superior inferior hemifield, the intact visual fields are separated from one another, resulting in a central horizontal strip of vision falling on the impaired hemifield of each eye. The resulting image has a “missing” horizontal central strip.[4]
Exotropia and esotropia of the eye results in horizontal hemifields to “sliding” horizontally respective to one another.
Diagnosis
Visual Field Defect
Perimetry is a useful tool in determining visual field defects (e.g., Humphrey Visual Field analyser or Goldman perimetry).[8] [15]Heteronymous visual field defects including bitemporal hemianopia, binasal hemianopia, and heteronymous altitudinal visual field defect in conjunction with pertinent history should increase suspicion for retinal hemifield slide phenomenon.[1]
Tropia
Extraocular motility exam would likely show full ductions and versions since there is no muscle restriction or paralysis. However ocular motility dysfunction findings does not preclude the hemifield slide phenomenon since the patient can have concurrent ocular motor dysfunction.[3] The cover-uncover test and cross-cover test determine existence of manifest deviations (tropias) and latent deviations (phorias), respectively. Prisms can determine the magnitude of these deviations both at distant and near fixation.[16]
Imaging
Depending on the suspected location of the lesion, different imaging modalities can help in the diagnosis of the underlying cause of the retinal hemifield slide phenomenon. Brain magnetic resonance imaging (MRI) with and without contrast could reveal an underlying lesion causing the retinal hemifield slide phenomenon. Lesions in proximity to the optic chiasm may be identified as the culprit in cases where bitemporal hemianopia is the associated visual field defect. [2][5][8][17]Visualization of the optic nerve via dilated fundus exam may show signs of edema, atrophy or cupping, narrowing the differential in the case of an altitudinal visual field defect. Optic computed tomography (OCT) is also a fast and noninvasive method of quantifying retinal nerve fiber layer thickness for atrophy or damage of the optic nerve.[4][8]
Management
Treatment of the retinal hemifield slide phenomenon depends on the underlying etiology. Surgical resection is the primary management when the cause is a resectable intracranial tumor like a pituitary macroadenoma when medical management has failed or is not applicable.[2][5][7] In some cases, the visual field defect and the diplopia completely resolve post-surgery.[2] However patients with residual visual defects post-surgery or in cases when the underlying cause is untreatable, further management of the visual symptoms may be appropriate. Unfortunately, specific recommendations for treatment modalities is not currently available in the literature.[16]
Orthoptic exercises such as fusional convergence exercises, pencil pushups, can aid in fusion of visual fields in cases of exotropia or exophoria.[16] Patients can also be prescribed prisms for everyday use to maintain binocular single vision.[2][16] More invasive procedures like botulism toxin injection into extraocular muscles and strabismus surgery have inconsistent results.[1][2]
Additional Resources
Hemifield Slide Phenomenon by Dr Andrew Lee. https://www.youtube.com/watch?v=YoQkthccyoc
Moran Core Lectures https://www.youtube.com/watch?v=sa8Xpfw0xKU
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 Peragallo, J. H., Bialer, O. Y., Pineles, S. L. & Newman, N. J. Hemifield Slide Phenomenon as a Result of Heteronymous Hemianopia. Neuro-Ophthalmol. 38, 82o-Ophthalmo
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Kini, A., Yennam, S., Othman, B. A. & Lee, A.G. Beware of the “Wolf in Sheep’s Clothing” in Your Eye Clinic. 3
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 van Waveren, M., Jägle, H. & Besch, D. Management of strabismus with hemianopic visual field defects. Graefes Arch. Clin. Exp. Ophthalmol. 251, 575–584 (2013).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Borchert, M. S., Lessel, S. & Hoyt, W. S. Hemifield Slide Diplopia from Altitudinal Visual Field Defects. J. Neuroophthalmol. 16, 107–109 (1996).
- ↑ 5.0 5.1 5.2 Mota, M. et al. Hemifield Slide Phenomenon from Pituitary Macroadenoma. Am. J. Ophthalmol. 3
- ↑ Elkington, S. G. Pituitary adenoma. Preoperative symptomatology in a series of 260 patients. Br. J. Ophthalmol. 52, 322–328 (1968).
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Peli, E.& Satgunam, P. Bitemporal hemianopia; its unique binocular complexities and a novel remedy. Ophthalmic Physiol. Opt. 34, 233–242 (2014).
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Foroozan, R. Visual Findings in Chiasmal Syndromes: Int. Ophthalmol. Clin. 56,1–27 (2016).
- ↑ Maniec, K. & Watson, J. C. Spontaneous Rupture, Disappearance, and Reaccumulation of a Rathke’s Cleft Cyst. Case Rep. Endocrinol. 2011, 1–3 (2011).
- ↑ Sodhi, A. K., Athappilly, G. & Marx, J. L. Woman presents with progressive decreasing vision in both eyes and new onset headaches. Case Rep. Endocrinol. 6 (2011).
- ↑ Bejjani, G. K. & Kennerdell, J. S. Visual Field Deficit Caused by Vascular Compression from a Suprasellar Meningioma: Case Report. 50, 4 (2002).
- ↑ Pula, J. H. & Yuen, C. A. Eyes and stroke: the visual aspects of cerebrovascular disease. Open Access 11
- ↑ Ashwin, P. T. & Quinlan, M. Interpreting binasal hemianopia: The importance of ocular examination. Eur. J. Intern. Med. 17, 144–145 (2006).
- ↑ Bryan, B. T., Pomeranz, H. D. & Smith, K. H. Complete Binasal Hemianopia. Bayl. Univ. Med. Cent. Proc. 27, 356–358 (2014).
- ↑ Trope, G. E. & Britton, R. A comparison of Goldmann and Humphrey automated perimetry in patients with glaucoma. Br. J. Ophthalmol. 71, 489–493 (1987).
- ↑ 16.0 16.1 16.2 16.3 Ko, T.-C., Wu, P. K. W. & Lo, B. K. K. Hemifield slide phenomenon in a patient with bitemporal hemianopia. 3
- ↑ Chen, C. S. Bitemporal Hemianopia Caused by an Intracranial Vascular Loop. Arch. Ophthalmol. 126, 274 (2008).