Retinal Displacement Following Rhegmatogenous Retinal Detachment Repair
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Retinal Displacement is an abnormality in which the retina is shifted relative to the retinal pigment epithelium (RPE).1 This phenomenon occurs after repair of retinal detachment (RD) and is diagnosed using fundus autofluorescence (FAF) imaging. Retinal displacement was described for the first time by Shiragami et al. in 2010, after repair of rhegmatogenous retinal detachment (RRD) with pars plana vitrectomy (PPV) and gas tamponade.2 This abnormality should be suspected in patients who have undergone anatomically successful RRD repair but experience symptoms of distortion such as metamorphosia, dysmetropia, and aniseikonia.3
Risk Factors
i. RRD involving more than 1 quadrant2,4
ii. Macula-off RRD2,3
iii. Use of gas tamponade during repair4,5
iv. Repair with PPV as compared with scleral buckling and pneumatic retinopexy6
Pathophysiology
The pathophysiology of retinal displacement is not well elucidated. Some evidence suggests that retinal displacement may be a result of subretinal fluid flowing underneath the retina due to the tamponade used. The thin elastic retina may stretch due to the buoyant force of the tamponade.7,8 A computer simulation model has suggested that the size of retinal displacement may be related to the size of gas tamponade used as the gas stretches the retina by displacing subretinal fluid after RRD repair.9 This hypothesis may be supported by the observation that the retina is typically displaced inferiorly due to head positioning and gravity. Some studies have suggested that face-down positioning may decrease displacement as face-down positioning encourages fluid flow in all directions rather than just inferiorly.7 However the results from studies are mixed. 6
Primary Prevention
Further study is needed to elucidate strategies to decrease the rate of retinal displacement. Some studies have suggested that face-down position was associated with a reduction in the rate and amplitude of postoperative retinal displacement after macula involving retinal detachment repair. This is because face-down positioning encourages flow of posterior subretinal fluid in all directions rather than just inferiorly.There are mixed results regarding the use of silicone oil to decrease the incidence of retinal displacement. The use of silicone oil as a tamponade or a small expansile gas bubble in the case of pneumatic retinopexy have a lower contact area and contact pressure leading to an overall decreased buoyant force.7
Diagnosis
History
Patients who report unsatisfactory functional outcomes after RRD repair despite successful anatomic reattachment should be suspected of having potential retinal displacement. Patients may report symptoms of metamorphosia, dysmetropia, and aniseikonia.3,6
Physical Examination
When a patient presents with visual distortion after RRD repair, it is important to conduct a comprehensive exam to ensure that there is not any underlying pathology causing these changes.Visual acuity, pupillary examination, intraocular pressure measurements, and visual field testing should be conducted. Visual acuity should remain stable when retinal displacement is present.Slit lamp examination of the anterior segment should be completed to rule out cataract as a source of visual distortion. Anterior vitreous examination to check for signs of pigment and vitreous hemorrhage should be done. Thorough fundus examination should be done to ensure that there is not repeat detachment of the retina. In theory the direct visualization of the retina might reveal displacement of the blood vessels, especially in relation to their normal orientation. This might be appreciated as a noticeable shift in the course of arterioles or venules compared to their usual anatomical trajectory. Additionally, areas of fibrosis, scarring, or retinal folds may also be visible which can contribute to retinal displacement.
Clinical Diagnosis
Direct visualization of the retina can reveal displacement of the blood vessels, especially in relation to their normal orientation. This can be appreciated as a noticeable shift in the course of arterioles or venules compared to their usual anatomical trajectory. Additionally, areas of fibrosis, scarring, or retinal folds may also be visible. Moreover, the timing of the onset of symptoms following the surgery is key to differentiating this condition from other complications. Patients may report visual distortion or shifts in vision, such as straight lines appearing wavy, particularly when vascular displacement involves the macula. Metamorphopsia, a visual distortion where straight lines appear wavy or curved, is typically measured through a variety of clinical tools. The Amsler grid is a common, quick, subjective method where patients self-report distorted areas. For more precision, M-CHARTS quantify the distortion by presenting lines with varying spacing, giving a numerical measurement of the degree of metamorphopsia. Preferential Hyperacuity Perimetry (PHP) provides an objective, computerized assessment of subtle distortions, commonly used in macular diseases. Emerging technologies like virtual reality (VR) offer potential future methods for more immersive real-time assessments.10
Diagnostic procedures
Ancillary Testing
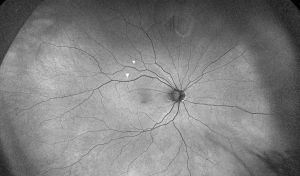
The diagnosis of retinal displacement is made by the presence of hyperautofluorescent lines on FAF imaging. These lines may be referred to as “retinal vessel printings” (RVPs) or retinal pigment epithelial vessel ghost lines” and are thought to indicate the original location of retinal vessels before retinal detachment.7
Differential diagnosis
1) Epiretinal Membrane (ERM) formation after RD repair
2) Retinal re-detachment especially in the periphery
3) Subretinal fluid accumulation post RD repair
4) PVR (Proliferative Vitreoretinopathy)
Management
General treatment
In cases where the displacement is minimal and not causing significant vision loss, careful monitoring may be recommended. If conditions like epiretinal membranes, macular holes, or PVR are present, additional treatments may be required, including surgical options tailored to these specific issues.
Additional Resources
Add text here
References
1. Shaheen AR, Iyer PG, Flynn HW, Yannuzzi NA. Retinal displacement following repair of rhegmatogenous retinal detachment. Oman J Ophthalmol. 2023;16(2):205-210. doi:10.4103/ojo.ojo_187_22
2. Shiragami C, Shiraga F, Yamaji H, et al. Unintentional Displacement of the Retina after Standard Vitrectomy for Rhegmatogenous Retinal Detachment. Ophthalmology. 2010;117(1):86-92.e1. doi:10.1016/j.ophtha.2009.06.025
3. Lee E, Williamson TH, Hysi P, et al. Macular displacement following rhegmatogenous retinal detachment repair. Br J Ophthalmol. 2013;97(10):1297-1302. doi:10.1136/bjophthalmol-2013-303637
4. Codenotti M, Fogliato G, Iuliano L, et al. Influence of intraocular tamponade on unintentional retinal displacement after vitrectomy for rhegmatogenous retinal detachment. Retina. 2013;33(2):349-355. doi:10.1097/IAE.0b013e318263d180
5. dell’Omo R, Scupola A, Viggiano D, et al. Incidence and Factors Influencing Retinal Displacement in Eyes Treated for Rhegmatogenous Retinal Detachment With Vitrectomy and Gas or Silicone Oil. Investigative Ophthalmology & Visual Science. 2017;58(6):BIO191-BIO199. doi:10.1167/iovs.17-21466
6. Mahmoudzadeh R, Swaminathan S, Salabati M, et al. Retinal Displacement Following Rhegmatogenous Retinal Detachment Repair. Ophthalmic Surgery, Lasers and Imaging Retina. 2024 Jul 1:1-7. doi: 10.3928/23258160-20240528-01.
7. Brosh K, Francisconi CLM, Qian J, et al. Retinal Displacement Following Pneumatic Retinopexy vs Pars Plana Vitrectomy for Rhegmatogenous Retinal Detachment. JAMA Ophthalmology. 2020;138(6):652-659. doi:10.1001/jamaophthalmol.2020.1046
8. Mason RH, Minaker SA, Marafon SB, Figueiredo N, Hillier RJ, Muni RH. Retinal displacement following rhegmatogenous retinal detachment: A systematic review and meta-analysis. Survey of Ophthalmology. 2022;67(4):950-964. doi:10.1016/j.survophthal.2022.01.002
9. Farahvash A, Marafon SB, Juncal VR, Figueiredo N, Ramachandran A, Muni RH. Understanding the mechanism of retinal displacement following rhegmatogenous retinal detachment repair: A computer simulation model. Acta Ophthalmologica. 2022;100(5):e1163-e1171. doi:10.1111/aos.15050
10. Simunovic MP. Metamorphopsia and its quantification. Retina. 2015 Jul 1;35(7):1285-91. doi: 10.1097/IAE.0000000000000581

