Refractive Surgery Enhancements
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Refractive surgery constitutes of elective vision correction options to reduce the refractive error for an otherwise healthy subject. The currently relevant options can be divided into (a) substractive (excimer ablation, lenticule extraction), (b) additive (phakic IOL implantation) and (c) exchange based (refractive lens replacement).
Refractive surgery has become consistent and reliable in the recent times. There is a high satisfaction rate among patients and the visual outcomes have been fairly standardized due to better fluence , improved laser beam configurations and delivery models, knowledge of operative suite environment control, iris recognition and eye tracking, and customized algorithms.
However, there is still a subset of patients who either do not achieve satistfactory uncorrected vision after refractive surgery due to under- or overcorrection (with all the techniques), regression (with excimer ablation) or increase in myopia (with implanted lenses).
Causes and risk factors of post surgery refractive error
Causes and risk factors of post surgery refractive error [1] [2] [3]
There can be multiple causes of early residual error: improper refraction/data entry, learning curve, decentered ablation or blocked ablation, and fluence issues, to include a few. Over correction may be often due to incorrect pre-operative measurement, over or under done algorithm adjustment, or intra-operative dehydration of the cornea. Implantable collamer lens rotation can lead to unexpected astigmatism.To add to this, even advanced IOL formulas may be off the mark in extremes of axial length for lens exchange. Late changes can be due to increase in axial myopia, lenticular myopia, corneal reshaping or also due to pregnancy or endocrinal disorders. It is imperative to rule out post lasik ectasia in these cases as it could mimic post lasik regression especially in the early stages of ectasia when there are only subtle changes in topography. The above information is useful as it would help in deciding for refractive surgery enhancement.
Indications for refractive surgery enhancement
The indications for refractive surgery enhancement include
- Realistic patient and surgeon expectation: the primary aim of refractive surgery is to make a candidate free of refractive correction for most of his personal and professional work. If the patient is happy with a mild, occasional refractive correction at challenging but rare tasks, enhancement may not be needed in spite of residual refractive error. There is a strong role of preoperative and postoperative counseling here. However, if the refractive error/ post operative aberration profile is affecting the patient‘s daily activities, an enhancement should be strongly considered.
- A stable residual refractive error: First and foremost, the refractive error must be stable for at least 3 months. Some cases would be worth waiting six or more months, especially with borderline residual beds.
- Explainable and correctable visual deficit due to the refractive error: The residual refractive error should be able to explain the difference between the postoperative visual acuities: corrected and uncorrected. The aim should be to assess the spectacle corrected visual acuity and try to match it after the enhancement. In the simplest of cases, refraction may suffice. For example, a patient with a postoperative residual error of -1 D spherical which improves his current uncorrected vision from 20/40 to 20/20 fits the bill. However, a patient with a 20/120 UDVA, improving with correction of -1D to only 20/60 does not. There have to be other causes including retinal issues such as macular lesions to these situations other than just refractive error. In some cases with very distorted aberration profiles, the spectable correction may not be able to get the patient back to the preoperative BCVA. However in such cases also , the visual acuity will be fairly commensurate with the lower order aberration profile.
- Enough buffer for the enhancement: There should be enough scope of the additional surgical intervention. For example, there should be enough residual bed if a flap relift is planned. For cases with bioptics with the first surgery being a phakic IOL implantation or IOL exchange, the cornea should be healthy enough to allow an excimer ablation. Often phakic IOLs are done for high myopia. In such cases a top-up excimer ablation of 1-2 dioptres can be done if the cornea permits. However, in cases with thin/suspect/keratoconic corneas undergoing ICL, the corneal ablation would be a contraindication.
- No systemic or ocular contraindication for surgery: The enhancement should be considered as a full surgery like the first correction, and a detailed reassessment of the eye including ruling out retinal lesions from the first surgery is a good practice.
Decision making algorithm
There are multiple studies using methds like flap reflit (manually or after femtosecond side cut), surface ablation over a LASIK, wavefront or non wavefront guided ablation to include a few.[4] [5] [6][7] [8] [9] [10] [11] [12] [13] [14] However, there is no published strong meta-analysis in literature establishing a clear cut prefered practice pattern when it comes to enhancement. The actual decision making algorithm can defer from surgeon to surgeon and with the availability or experience with a particular enhancement method.
However the guiding principles are the same:
- Stable refraction
- Correct elucidation of cause of error
- Maximum possible correction performed safely.
- Proper counselling
- No contraindication for the chosen method of enhancement
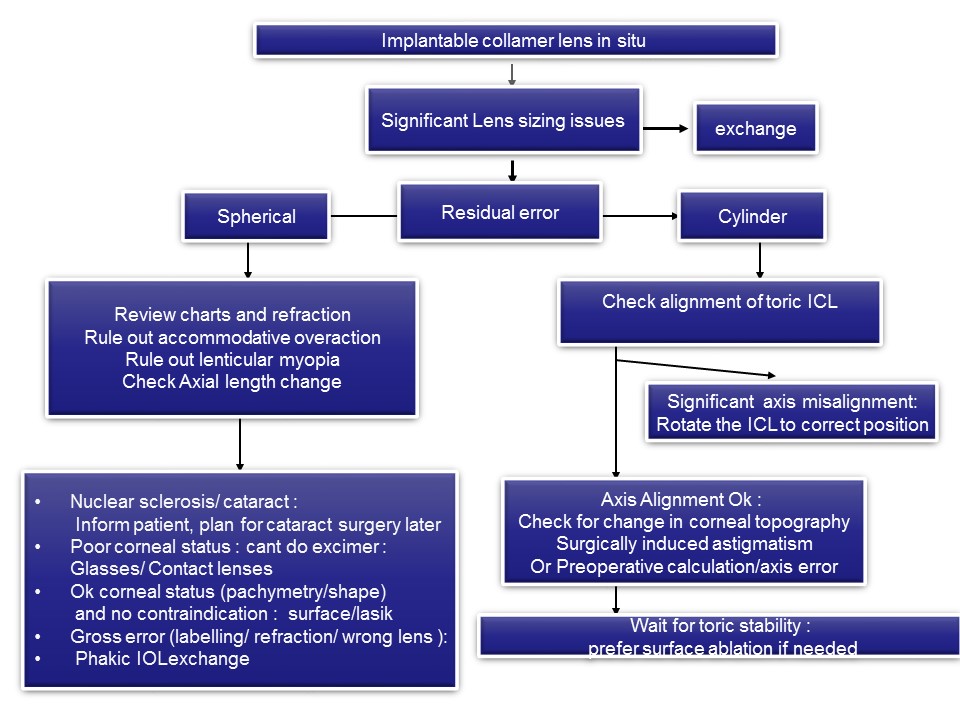
Example method for post phakic IOL implantation enhancement
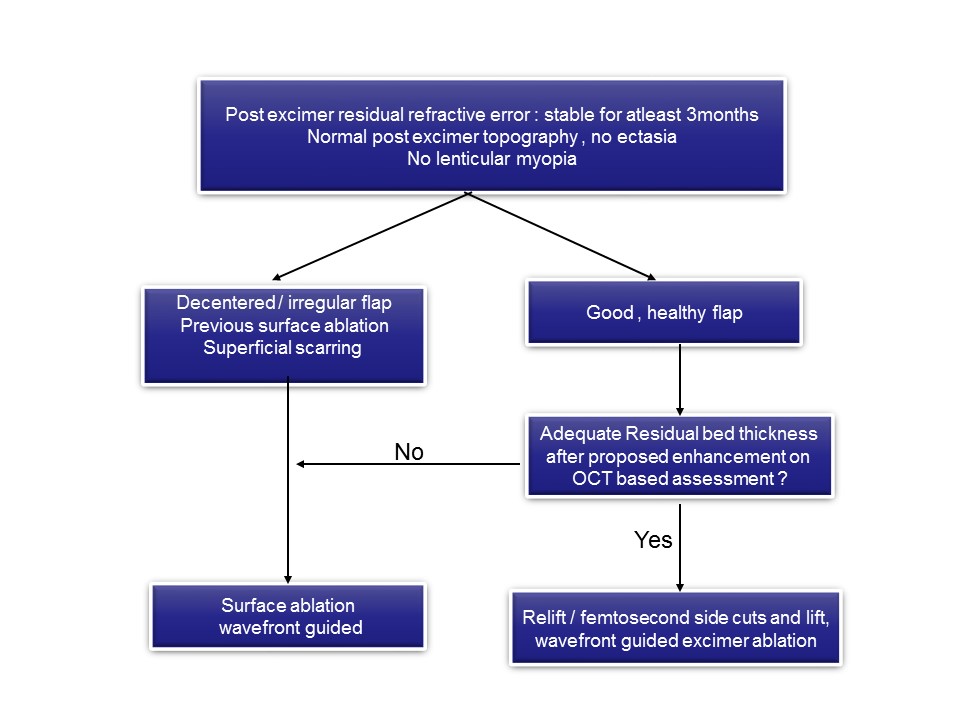
Example post excimer ablation enhancement algorithm
Case Examples
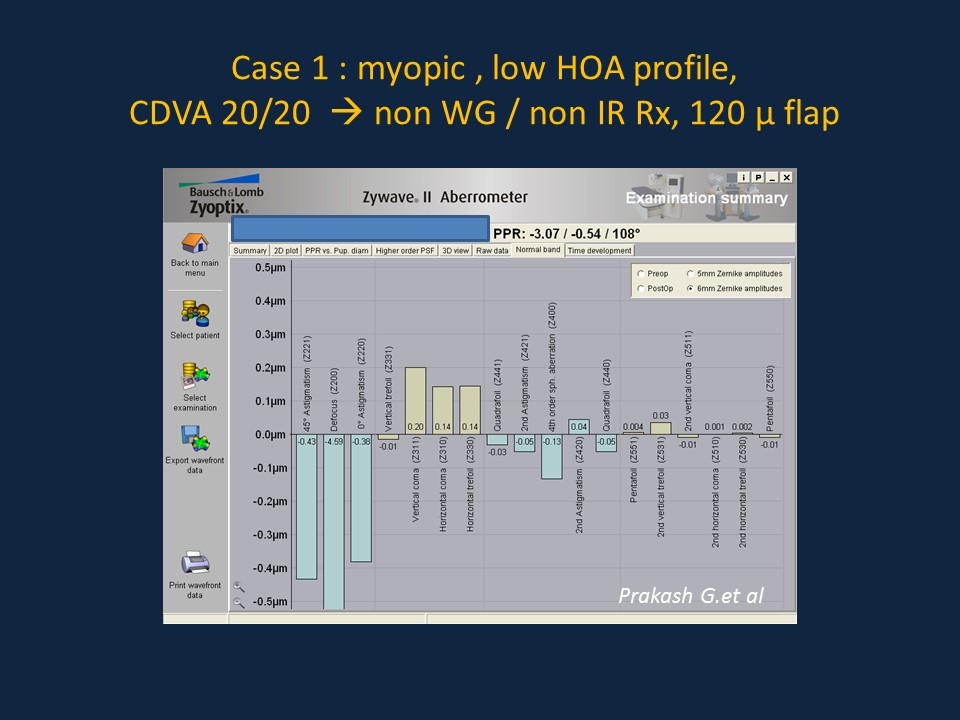
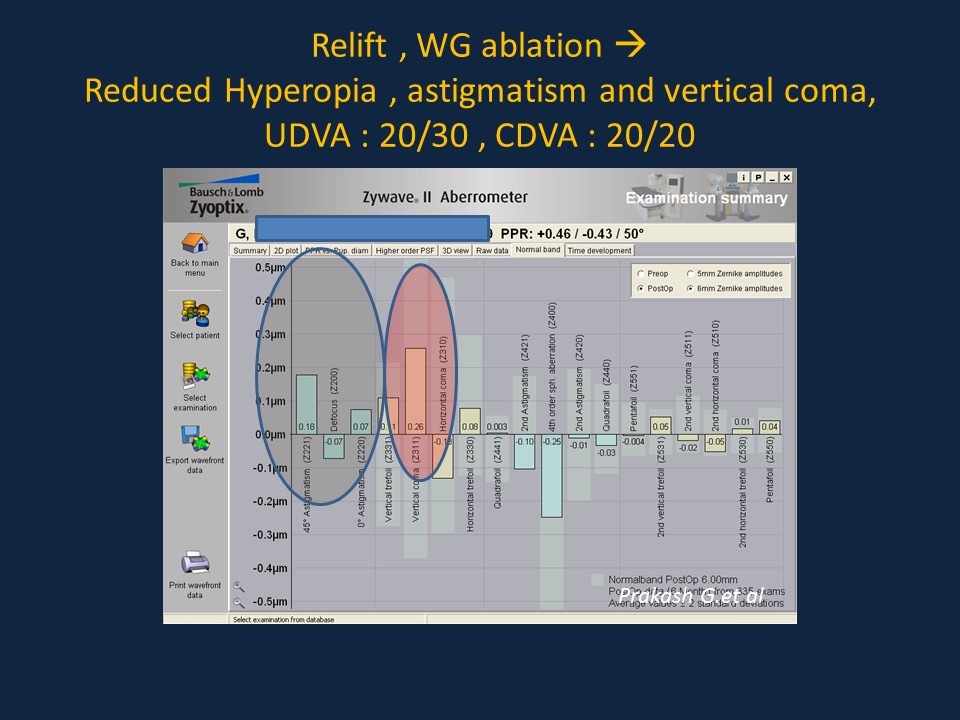
Case 1
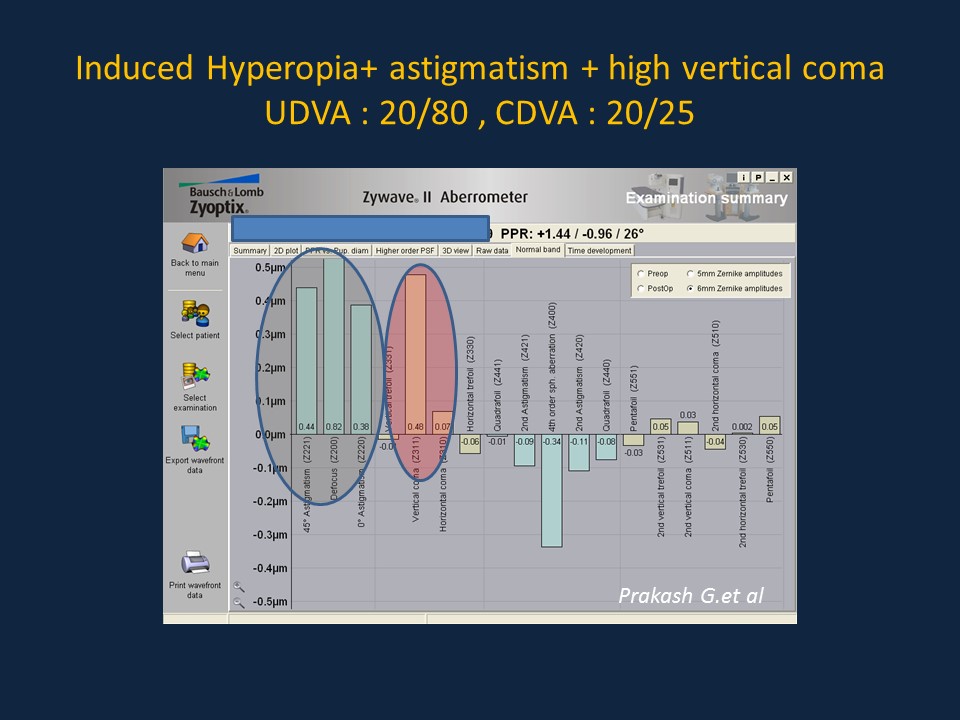
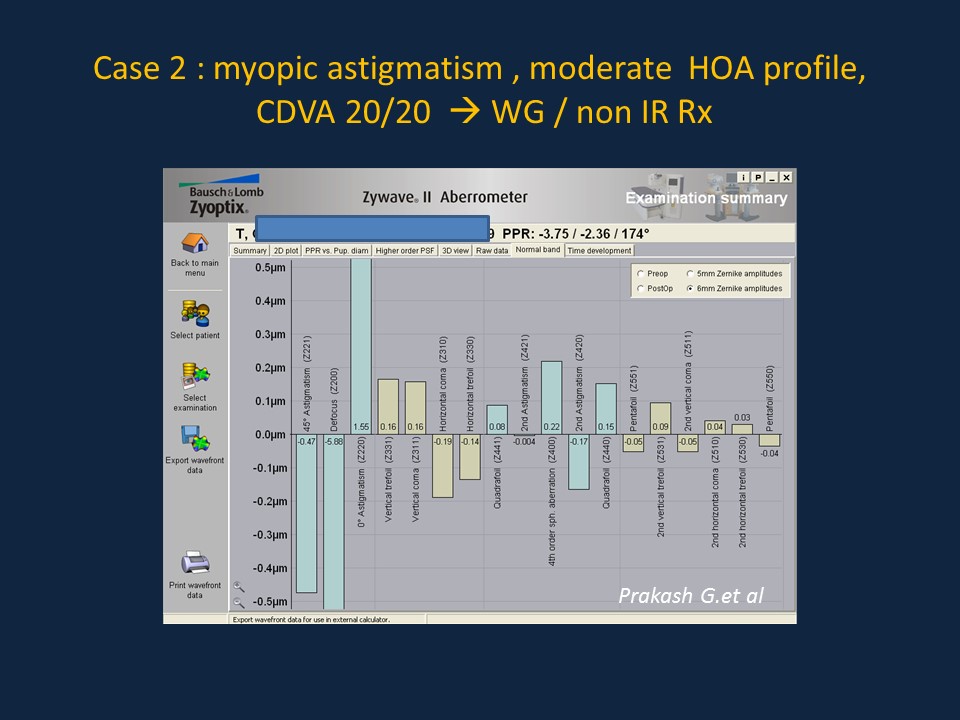
Case 2
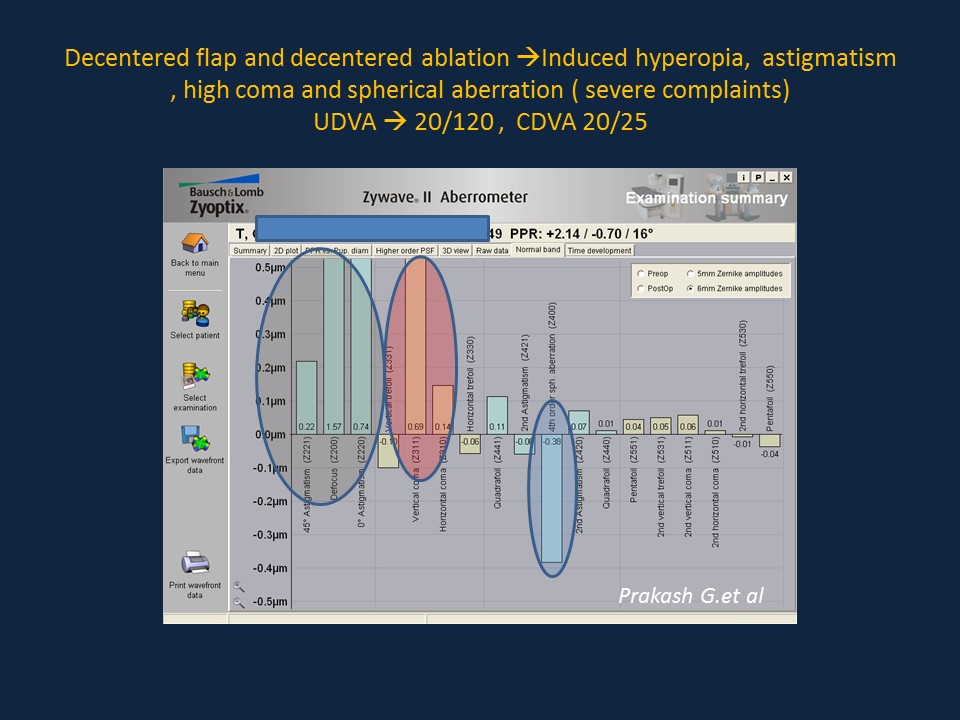
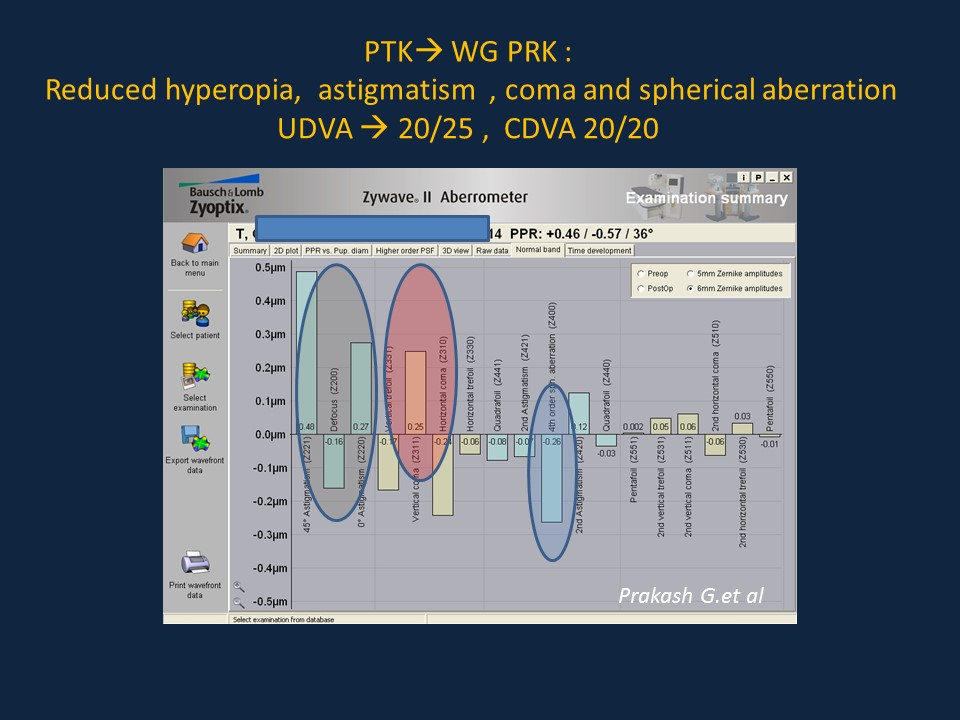
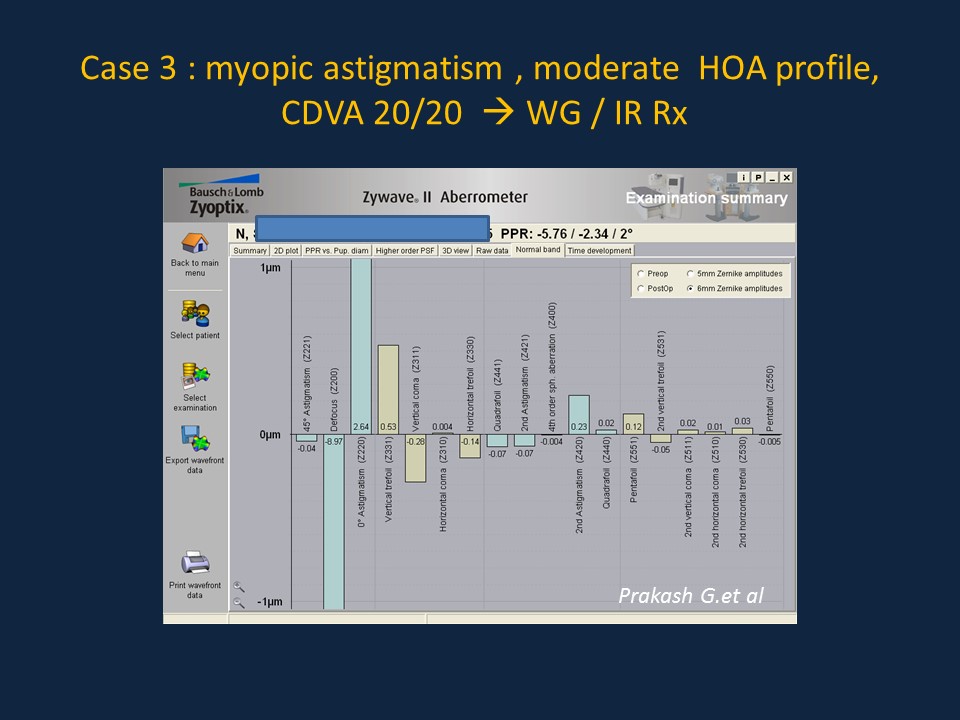
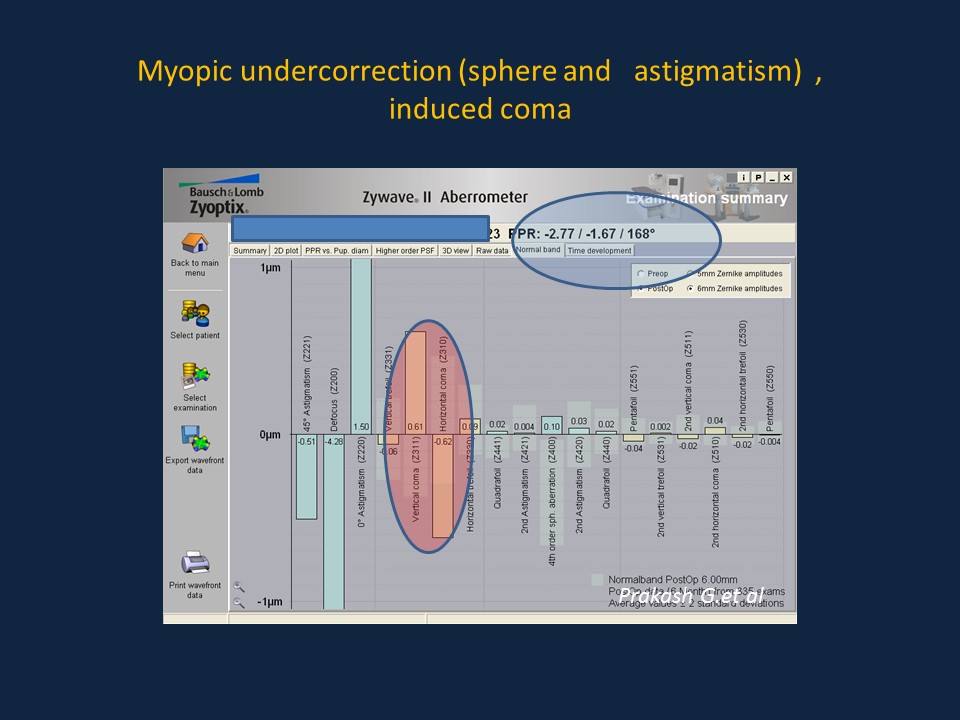
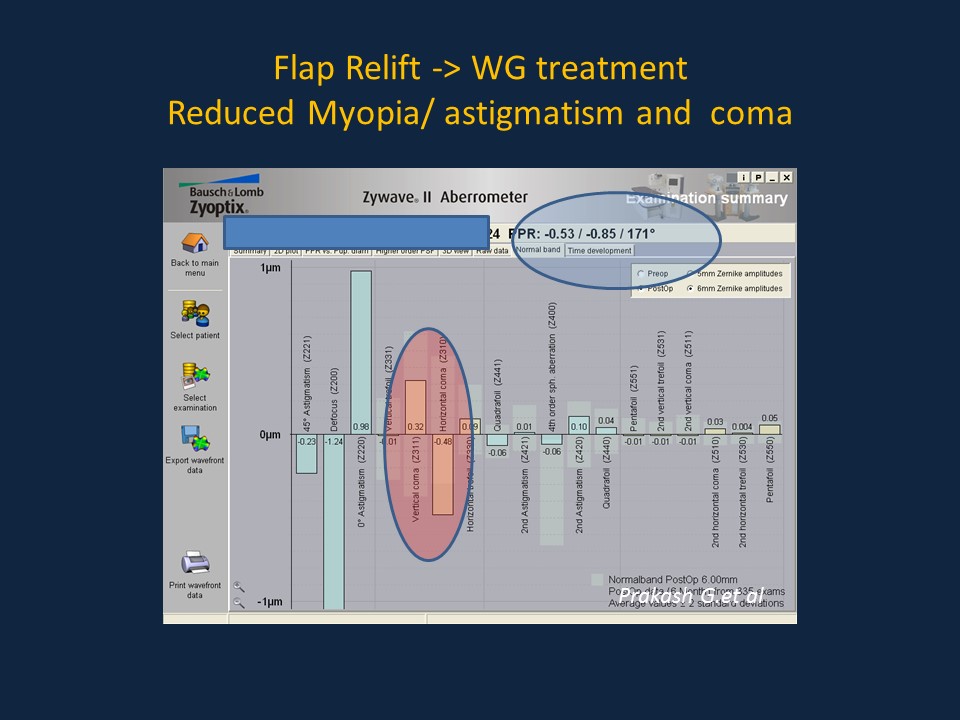
Case 3
Prognosis
In cases with judicious planning and selection of technique, the results are typically satisfactory after the enhancement procedure.
Additional Resources
- Agarwal A and Prakash G .Multi-optional algorithm helpful for LASIK enhancement.Ocular Surgery News .April 10 , 2012. Accessed online from http://www.healio.com/ophthalmology/refractive-surgery/news/print/ocular-surgery-news/%7Bbd89305b-2a4a-4885-abb5-24f3cb209977%7D/multi-optional-algorithm-helpful-for-lasik-enhancement
- Kent C . Chasing Perfection: Strategies For Enhancing LASIK . Review of Ophthalmology,, July 2009. Accessed online from http://www.revophth.com/content/d/features/i/1214/c/22878/
References
- ↑ Sharma N, Balasubramanya R, Sinha R, Titiyal JS, Vajpayee RB. Retreatment of LASIK. J Refract Surg. 2006 Apr;22(4):396-401.
- ↑ Randleman JB, White AJ Jr, Lynn MJ, Hu MH, Stulting RD. Incidence, outcomes, and risk factors for retreatment after wavefront-optimized ablations with PRK and LASIK. J Refract Surg. 2009 Mar;25(3):273-6.
- ↑ Mori T, Yokoyama S, Kojima T,et al . Factors affecting rotation of a posterior chamber collagen copolymer toric phakic intraocular lens. J Cataract Refract Surg. 2012 Apr;38(4):568-73.
- ↑ Parikh NB. Management of residual refractive error after laser in situ keratomileusis and photorefractive keratectomy. Curr Opin Ophthalmol. 2014 Jul;25(4):275-80.
- ↑ Vaddavalli PK, Diakonis VF, Canto AP, Culbertson WW, Wang J, Kankariya VP, Yoo SH. Complications of femtosecond laser-assisted re-treatment for residual refractive errors after LASIK. J Refract Surg. 2013 Aug;29(8):577-80.
- ↑ Khor WB, Afshari NA. The role of presbyopia-correcting intraocular lenses after laser in situ keratomileusis. Curr Opin Ophthalmol. 2013 Jan;24(1):35-40.
- ↑ Pietilä J, Huhtala A, Mäkinen P, Uusitalo H. Laser in situ keratomileusis enhancements with the Ziemer FEMTO LDV femtosecond laser following previous LASIK treatments. Graefes Arch Clin Exp Ophthalmol. 2013 Feb;251(2):597-602.
- ↑ Albarrán-Diego C, Muñoz G, Ferrer-Blasco T. Subjective refraction before LASIK enhancement in bioptics procedures with refractive multifocal intraocular lenses. J Refract Surg. 2011 Aug;27(8):556-7.
- ↑ Netto MV, Wilson SE. Flap lift for LASIK retreatment in eyes with myopia. Ophthalmology. 2004 Jul;111(7):1362-7.
- ↑ Santhiago MR, Smadja D, Zaleski K, Espana EM, Armstrong BK, Wilson SE. Flap relift for retreatment after femtosecond laser-assisted LASIK. J Refract Surg. 2012 Jul;28(7):482-7.
- ↑ Al-Mezaine HS, Al-Amro SA, Al-Fadda A, Al-Obeidan S. Outcomes of Retreatment after Aborted Laser In Situ Keratomileusis due to Flap Complications. Middle East Afr J Ophthalmol. 2011 Jul;18(3):232-7.
- ↑ McAlinden C, Moore JE. Retreatment of residual refractive errors with flap lift laser in situ keratomileusis. Eur J Ophthalmol. 2011 Jan-Feb;21(1):5-11.
- ↑ Alió JL, Piñero D, Muftuoglu O. Corneal wavefront-guided retreatments for significant night vision symptoms after myopic laser refractive surgery. Am J Ophthalmol. 2008 Jan;145(1):65-74.
- ↑ Toda I, Kato-Asano N, Hori-Komai Y, Tsubota K. Dry eye after LASIK enhancement by flap lifting. J Refract Surg. 2006 Apr;22(4):358-62.