Recurrent Corneal Erosion
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Recurrent Corneal Erosion (RCE) syndrome is a common, recurrent condition caused by abnormal epithelial adhesion to the underlying basal lamina. The spontaneous breakdown of the corneal epithelium can lead to the sudden onset of ocular pain, blurred vision, tearing, and photophobia, typically upon awakening.[1][2][3]
Conservative and surgical treatments are available depending on the severity and duration of the corneal erosions.
Etiology
- Trauma is the most common cause of RCE.[2]
- Corneal dystrophies such as
- epithelial basement membrane dystrophy,
- Reis- Buckler dystrophy,
- lattice dystrophy,
- macular dystrophy,
- granular dystrophy, and
- Fuchs endothelial corneal dystrophy;
- previous corneal infections;
- meibomian gland dysfunction;
- diabetes mellitus;
- ocular rosacea;
- band keratopathy;
- nocturnal lagophthalmos; and,
- dry eye syndrome have all been implicated in the pathogenesis of RCE.[2]
Risk Factors
- Mechanical trauma from foreign bodies, fingernails, tree branches, paper cuts, accounts for 45-64% of cases according to studies.[3][4]
- Corneal dystrophies like anterior basement membrane dystrophy (ABMD, aka Cogan dystrophy or map-dot-fingerprint dystrophy) are associated with 19–29% of cases.[3]
- Patients with diabetes, dry eye syndrome, and ocular rosacea are at potential risk to develop RCE.[5]
Pathophysiology
Injury to the corneal surface can result in an epithelial defect. Healing occurs in three distinct phases characterized by epithelial cell migration, proliferation, and differentiation.[6] Trauma to the corneal epithelium induces the migration of the remaining epithelial cells adjacent to the injury site toward the defective area. Changes in cell–cell and cell–matrix (fibronectin–integrin system) interactions and modulation of the extracellular matrix by newly expressed proteolytic enzymes play important roles.
Patients with RCE demonstrate a faulty, loose adherence of the epithelium to the underlying stroma following the initial injury, that can be sheared off upon awakening with the opening of the eyelids.[7] Recurrent erosions occur secondary to inflammation from the inciting insult, which causes disruption of the epithelial basement membrane and proper extracellular adhesions of the hemidesmosomes. In affected patients, in vivo confocal microscopy demonstrates defects of the adhesion complex, deposits in basal epithelial cells, sub basal microfolds and streaks, damaged sub basal nerves, aberrant basement membrane, and altered morphology of the anterior stroma.[8]
Increased levels of toxic free fatty acids, interleukin-1, and matrix metalloproteinases (MMPs) in patients suffering from meibomian gland dysfunction, ocular rosacea, and recurrent erosions is thought to result in faulty adhesion complexes and abnormal basement membrane formation.[2]
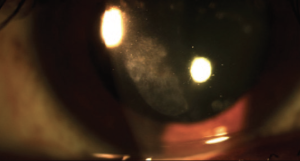
Diagnosis
RCE is diagnosed with slit lamp examination. Findings range from normal exam to mild irregularities of the cornea (such as epithelial microcysts) to large areas of loose epithelium or epithelial defects, which can be delineated with fluorescein staining. Intrinsic abnormalities of corneal epithelial adhesions such as from corneal dystrophies tend to present bilaterally and symmetrically. In cases of previous trauma, the area of erosion usually corresponds to the location of the previous injury.
In a study done by Hykin et al., the site and size of the erosion was measured by dividing the cornea into twelve sectors and measuring how many sectors were involved. This allowed the corneal erosion to be classified as small (0-3 sectors), moderate (4-6 sectors), large (7-9 sectors), or very large (10-12 sectors). According to their findings, the lower half of the cornea was the most frequently affected location.[3]
Signs and Symptoms
Chandler classified RCE into two forms: (1) Microform erosions tend to be milder in symptoms and shorter in duration but occur with increased frequency. (2) Macroform erosions can persist for days at a time, and are usually associated with a history of trauma.[4]
- Mild to severe pain, particularly upon awakening
- Foreign body sensation
- Photophobia
- Blurred vision
- Lacrimation
Differential diagnosis
- Band keratopathy
- Corneal ulcers (bacterial, fungal, or herpetic)
- Neurotrophic keratitis
- Corneal foreign body
- Limbal stem cell deficiency
- Corneal dystrophies (epithelial, stromal, or endothelial)
- Chemical and thermal burns
- Dry eye syndrome
- Floppy eyelid syndrome
- Salzmann’s nodular degeneration
Management
RCE treatment may be either medical or surgical and should be individualized for each patient dependent on slit lamp findings and clinical history. The primary goal is to facilitate re- epithelialization and reestablishment of the basement membrane complex.[2]
Medical therapy
- Lubrication: As first line therapy or a mainstay of treatment in the prevention of RCE, the use of preservative-free artificial tears and ointment (hypertonic or paraffin) is recommended frequently during the day and before bedtime to keep the ocular surface moist. However, patients with ABMD have an increased risk of prophylactic failure.[3][5][6] Autologous serum tears and cyclosporine 0.05% as second- line therapies in patients who failed lubrication and patching have been shown to be effective in preventing recurrences.[9][10]
- Patching & cycloplegia: During acute episodes of corneal erosion, instillation of a topical cycloplegia with a temporary patch is effective in promoting healing of the ocular surface.[11]
- Antibiotics and pain relievers: Topical antibiotics are commonly prescribed to prevent bacterial infections in patients with epithelial defects. Oral pain relievers such as ibuprofen may be helpful in reducing ocular discomfort during acute episodes.
- Anti- inflammatories:
- It has been reported that doxycycline, a MMP-9 inhibitor,[12] in combination with topical corticosteroids, reduces the frequency of RCE.[13] The recommended dose of doxycycline is 50 mg orally two times daily.
- Topical corticosteroids (methylprednisolone 1%, prednisolone acetate 1%, or fluorometholone 0.1%) can be used two or three times a day for 3 weeks.[14]
- Topical cyclosporine 0.05%, an IL-2 inhibitor, has been associated with a decrease in RCE episodes in a small case-series.[10]
- Hypertonic saline solution or ointment: Use of hypertonic saline (especially used at bed time) has been shown to be effective in both acute and chronic RCE.[15][16]
Conservative Treatment
- Bandage Contact Lens: A Hydrogel soft contact lens can be left in place while the epithelium heals and stabilizes. The provider should counsel the patient on the signs and symptoms of infection. Fraunfelder et al. reported that 75% of patients with RCE treated for three months with an extended- wear BCL remained recurrence free at one year.[17] Topical antibiotic should be used as prophylaxis against infection.[1][2][17][5]
- Punctal Occlusion: Punctal occlusion is safe, quick, and reversible, and helps increase retention of eyedrops on the ocular surface.[5] Punctal occlusion can be considered in patients with dry eye syndrome. Temporary occlusion with collagen plugs, which usually dissolves in four to seven days, can be helpful. However, if the corneal erosion is chronic, permanent occlusion with silicon plugs is recommended. The patient should be aware that plugs may extrude or migrate over time.
Surgery
- Anterior Stromal Micro puncture: Anterior stromal micro puncture is a procedure that can be performed with the patient at the slit lamp. Anesthetic drops are administered (proparacaine) and a 25- gauge needle with a 1mL syringe is used to create micro punctures less than 1mm apart over the area of loose epithelium.[18][19] The use of cobalt blue light and fluorescein staining helps visualize the area of treatment. Nd:YAG laser micro puncture using 0.4mJ – 0.5mJ pulses, applied to the region of abnormal Bowman layer through an intact epithelium has also been described.[20] Micro puncture treatment is thought to incite a fibrocystic response, resulting in stimulation of basement membrane production. Epithelial adherence is improved by scar tissue induction between the epithelium and the anterior stroma of the cornea. Zauberman et al. reported that the use of micro puncture with a 25- gauge needle had an effectiveness in 62.9% in eyes with RCE after a single treatment.[18]
- Diamond Burr Polishing: Involves epithelial debridement with a cellulose sponge or blade and diamond burr polishing of Bowmans membrane. A bandage contact lens is then used for 4 -5 days along with a topical antibiotic and steroid.[1]
- Excimer Laser Phototherapeutic Keratectomy (PTK): After removal of the central epithelium, an excimer laser is used to ablate the cornea uniformly, creating an ablation depth of 5–6um. In a study conducted by O'Brart, 73% of patients suffering from RCE reported resolution of their symptoms at their final visit.[21]
- Topical insulin has been described to promote re- epithelialization in patients with RCE.[22]
Complications
- Corneal haze and scarring
- Infectious keratitis particularly in the setting of prolonged use of bandage contact lenses and topical steroids
- Decreased vision
Prognosis
With adequate treatment and prompt diagnosis, prognosis is excellent. Patients should be educated on the signs and symptoms of recurrent erosions so they can seek medical attention when appropriate. Prophylaxis treatment in patients with risk factors should be considered in order to minimize long-term complications.
References
- ↑ Jump up to: 1.0 1.1 1.2 Suri K, Kosker M, Duman F, Rapuano J, Nagra P, Hammersmith K. Demographic Patterns and Treatment Outcomes of Patients With Recurrent Corneal Erosions Related to Trauma and Epithelial and Bowman Layer Disorders. Am J Ophthalmol 2013;156:1082–1087
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 Ramamurthi S, Rahman MQ, Dutton GN, Ramaesh K. Pathogenesis, clinical features and management of recurrent corneal erosions. Eye 2006;20(6):635–644.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Hykin PG, Foss AE, Pavesio C, Dart JK. The natural history and management of recurrent corneal erosion: a prospective randomised trial.Eye 1994; 8(Part 1): 35–40.
- ↑ Jump up to: 4.0 4.1 Chandler PA. Recurrent Erosion of the Cornea*. American Journal of Ophthalmology 1945;28:355-63.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 Thakrar R, Hemmati H. Treatment of Recurrent Corneal Erosions. EyeNet. Available at http://www.aao.org/eyenet/article/treatment-of-recurrent-corneal-erosions
- ↑ Jump up to: 6.0 6.1 Findley FM. Recurrent corneal erosions. J Am Optom Assoc 1986;57:392-6.
- ↑ Dohlman CN. Healing problems in the corneal epithelium. Jpn J Ophthalmol 198 1 ;25: 13 1-4.
- ↑ Rosenberg ME, Tervo TM, Petroll WM, Vesaluoma MH.In vivo confocal microscopy of patients with corneal recurrent erosion syndrome or epithelial basement membrane dystrophy.Ophthalmology 2000;107(3):565–573.
- ↑ Ziakas NG, Boboridis KG, Terzidou C, et al. Long-term follow up of autologous serum treatment for recurrent corneal erosions. Clin Exp Ophthalmol 2010;38:683-7.
- ↑ Jump up to: 10.0 10.1 Napoli PE, Braghiroli M, Iovino C, Demarinis G, Fossarello M. A study of refractory cases of persistent epithelial defects associated with dry eye syndrome and recurrent corneal erosions successfully treated with cyclosporine A 0.05% eye drops. Drug Des Devel Ther 2019;13:2001-8.
- ↑ Lin SR, Aldave AJ, Chodosh J. Recurrent corneal erosion syndrome. Br J Ophthalmol 2019;103:1204-8.
- ↑ Sobrin L, Liu Z, Monroy DC, et al. Regulation of MMP-9 activity in human tear fluid and corneal epithelial culture supernatant. Invest Ophthalmol Vis Sci 2000;4:1–7.
- ↑ Hope-Ross MW, Chell PB, Kervick GN, McDonnell PJ, Jones HS. Oral tetracycline in the treatment of recurrent corneal erosions. Eye 1994;8:384 –388.
- ↑ Dursun D, Kim M, Solomon A, Pflugfelderand S. Treatment of Recalcitrant Recurrent Corneal Erosions With Inhibitors of Matrix Metalloproteinase-9, Doxycycline and Corticosteroids. Am J Ophthalmol 2001;132: 8–13.
- ↑ Tsatsos M, Matsou A, Soultanidis M, Athanasiadis IK. Safety and Efficacy of Hypertonic Sodium Chloride 5% Ointment for Recurrent Corneal Erosion Syndrome. Cureus. 2022 Dec 21;14(12):e32796. doi: 10.7759/cureus.32796. PMID: 36694530; PMCID: PMC9858893.
- ↑ Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019 Feb 11;13:325-335. doi: 10.2147/OPTH.S157430. PMID: 30809089; PMCID: PMC6376883.
- ↑ Jump up to: 17.0 17.1 Fraunfelder FW, Cabezas M. Treatment of recurrent corneal erosion by extended-wear bandage contact lens. Cornea 2011;30(2):164–166.
- ↑ Jump up to: 18.0 18.1 Zauberman N, Artornsombudh P, Elbaz U, Goldich Y, Rootman D, Chan C. Anterior Stromal Puncture for the Treatment of Recurrent Corneal Erosion Syndrome: Patient Clinical Features and Outcomes. Am J Ophthalmol 2014;157:273–279
- ↑ Maréchal-Courtois C, Duchesne B. [Recurrent corneal erosion]. Bull Soc Belge Ophtalmol. 1993. 247(1):13-5
- ↑ Katz HR, Snyder ME, Green WR, Kaplan HJ, Abrams DA. Nd:YAG laser photo-induced adhesion of the corneal epithelium. Am J Ophthalmol. 1994 Nov 15. 118(5):612-22.
- ↑ O’Brart DP, Muir MG, Marshall J. Phototherapeutic keratectomy for recurrent corneal erosions. Eye 1994;8:378–83.
- ↑ 1. Esmail A, Ibrahim M, Nage S. Efficacy of topical insulin for recurrent epithelial corneal erosions. Ir J Med Sci. May 4 2023;doi:10.1007/s11845-023-03373-y

