Radial Keratotomy: Complications Management
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Hundreds of thousands of patients have undergone radial keratotomy (RK) for the correction of myopia since its introduction in the 1970s. Other refractive procedures have largely supplanted RK, and it is now very rarely performed. Although the rate of complications from RK is difficult to ascertain, Salz performed a review of 935 eyes from the Prospective Evaluation of Radial Keratotomy (PERK) study in 1984, and concluded that RK was safe with a relatively low rate of complications.[1] His findings were supported by another survey of 62,814 cases performed by Marmer, published in 1987, who found that less than 1% of patients experienced a decrease in visual acuity after RK.[2] However, long- term sequelae of patients who have undergone RK include diurnal fluctuations and progressive hyperopic shift that have continued to affect RK patients years after surgery.
Diurnal Fluctuation
Up to 60% of RK patients complain of diurnal fluctuations.[3] Most post-RK corneas gradually steepen as the day progresses, with the greatest variability in vision within the first few hours after awakening attributed to nocturnal flattening of the cornea.[3] Unfortunately, there is no effective treatment to compensate for diurnal fluctuations, as multiple pairs of glasses throughout the day may not be practical.
In regards to long- term results, at postoperative year three, the PERK study found that 58% of eyes had refractive error within 1.00D of emmetropia; 26% where under corrected and 16% were overcorrected by over 1.00D.[4] Furthermore, 12% of eyes continued to change by 1.00D or more between postoperative year one and three, indicating the lack of stability in these eyes.[4] Between six months and ten years after RK, 43% of eyes were found to have shifted in the hyperopic direction by 1.00D or more, demonstrating continued change even ten years after surgery.[5] Although there is no definitive treatment for long- term instability, the option of contact lenses, such as soft and rigid gas permeable designs, and spectacles may be helpful in achieving acceptable visual acuity.
Corneal perforations
Corneal perforations during RK are classified as micro and macro.
Micro perforations usually occurred in the inferotemporal cornea with an incidence of 2.3%.[6]
Macro perforations could be devastating, resulting in loss of the anterior chamber and requiring termination of the procedure. If the surgeon encountered a macro perforation, often 10-0 nylon sutures were required for wound closure and stabilization of the eye. Operating on a relatively dry field permitted timely detection of any leakage of aqueous humor and early recognition of a small perforation was critical in preventing macro perforations.[3] Factors that contribute to corneal perforations include inexperience with the knife blade, centripetal incisions, intraocular pressure (IOP) elevation during incisions, reincisions, prolonged corneal dehydration intraoperatively, corneal thickness measurement errors, and unexpected movements by the patient.
Self-sealing perforations were treated with cycloplegics (to dilate the pupil and prevent adherence of the iris to the perforation site), topical aqueous suppressants, topical antibiotics, and an ocular shield. Eye patching was not recommended to avoid compression of the cornea and opening of the incisions. However, a bandage contact lens could be used to seal the wounds.
Complications of corneal perforations included damage to the endothelium, Descemet membrane scarring, iridocorneal adhesions if there was a flat anterior chamber, laceration of the lens capsule, endophthalmitis, astigmatism, and epithelial ingrowth.
Incorrectly placed incisions & optical zone decentration
Incisions across the visual axis can induce scarring and irregular astigmatism causing a significant visual impact, especially if the optical zone is small. An unintended incision through the visual axis can result from patient movements, an unexpected Bell reflex, inexperience with the knife and forceps, and a dry corneal surface. The combined (Genesis) incision technique was designed to avoid this complication by using a centrifugal partial thickness cut followed by a centripetal cut to the optical zone made by a diamond blade.
Intersecting incisions can lead to corneal flaps, wound gape, and poor healing. To approximate the wound edges, interrupted 10-0 nylon sutures can be used and are typically left in place for 10 to 12 weeks.
If a transverse incision to treat astigmatism is incorrectly placed, it can result in an undesirable refractive outcome. Reincisions can result in irregular astigmatism and hypertrophic scars.
Other complications related to corneal incisions include limbal scarring, fibrovascular ingrowth if incisions extended beyond the clear cornea, corneal vascularization (especially in contact lens wearers), and epithelial inclusions of debris and deposits.
Refractive errors
Overcorrection
The Prospective Evaluation of Radial Keratotomy (PERK) trial defined overcorrection as a refractive error of greater than +1.00D, which occurred with an incidence between 0.80% and 33%.[4] In myopic patients, there is better adaptation with undercorrection than with overcorrection. The reasons being in overcorrection, a sudden demand for increased accommodation- convergence translated into a greater demand for functional divergence.[3]
Immediate postoperative overcorrection after RK was attributed to wound gaping and flattening of the cornea, which usually resolved within a few weeks. Due to the inherent poor predictability of corneal wound healing, patients sometimes ended up overcorrected without a clear explanation or were emmetropic after surgery, but ended up significantly overcorrected several years later.
Risk factors for overcorrection included too small of a clear zone, incisions that were too deep, radial incisions to the limbus, multiple enhancement procedures, not taking into account preoperative cycloplegic refractions, and postoperative ocular massage.
Overcorrection can be treated with spectacles, contact lenses, or suturing the incisions. Refractive surgery after RK has been described to be safe and effective, though Sierra et al. suggested photo refractive keratotomy rather than laser in sit keratomileusis (LASIK) in treating RK- induced hyperopia to minimize the risk for epithelial ingrowth.[7]
Undercorrection
In the PERK study, approximately 80% of patients experienced regression of intended effect between 0.5D and 4.25D.[8] Causes for undercorrection included regression secondary to natural wound healing, inaccurate calculations or surgery performed, and other patient variables such as flat corneas, low intraocular pressures, and formation of corneal scarring. Surgical treatments for undercorrection include additional incisions or opening and deepening the initial incisions made.
Astigmatism
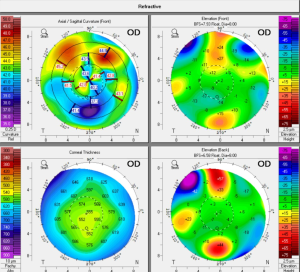
Astigmatism can be residual (not corrected by surgery) or induced (increased after surgery). This may occur if fewer incisions are made, if the incisions are asymmetric in respect to the visual axis or have a variable deepness, or if the optical zone is decentered. Irregular astigmatism is more frequent with repeated surgeries or incisions that extend too far into the visual axis. The majority of these refractive aberrations are self-limited and improve within the first six weeks. Refraction and corneal topography should be stable before placing additional incisions. Residual astigmatism can be treated with contact lens or glasses. Irregular astigmatism may be improved with the use of a rigid, gas permeable contact lens, particularly reverse geometry lenses. If there is significant visual impairment secondary to irregular astigmatism and corneal scarring, penetrating keratoplasty can be considered.
Premature presbyopia
In a previously myopic patient who achieved emmetropia or a patient who is overcorrected after RK, the loss of accommodative reserve required the use of spectacles for near work.
Contact lens intolerance
With shorter incisions (1 mm away from the limbus), the risk of corneal vascularization and fibrovascular ingrowth is reduced. Chronic contact lens wear is associated with irritation, hypoxia, wound stretching, and progressive hyperopia.
A soft lens with high oxygen transmissibility is recommended to decrease the incidence of neovascularization of the incisions, which is a common findings in post- RK patients.[9]
In patients with irregular astigmatism, rigid gas-permeable lenses with peripheral curves matching the patient’s preoperative parameters with a careful trial assessment are recommended.[10] A properly fitted contact lens may also be helpful for complaints of glare secondary to irregular astigmatism.[11]
Infectious keratitis
Most cases of infections keratitis occurred in the immediate postoperative period (days to weeks after RK). The most frequent organisms isolated were pseudomonas, staphylococcus aureus, and staphylococcus epidermis. The infiltrate is usually located within a keratotomy incision. There are several case reports of severe keratitis after RK that necessitated a penetrating keratoplasty.[12]
Delayed bacterial or fungal keratitis was a rare complication of RK that can occurred one to three years after surgery, likely due to the slow healing process after radial keratotomy.[3] Long-term prophylactic antibiotics were not routinely recommended. Extended wear contact lens and chronic corticosteroid usage may have increased the risk of infectious keratitis. Infectious keratitis can also be associated with cataracts, elevated intraocular pressure, and infectious crystalline keratopathy.
Herpes simplex keratitis
Surgical trauma can stimulate the recurrence of infection and impede wound healing. Several cases of herpes simplex keratitis have been reported after RK.[13]
Cataract
Cataract surgery can be safely performed after RK. Ophthalmologists are increasingly seeing more post- RK patients present for cataract surgery. Intraocular lens (IOL) calculations are challenging due to difficulties in determining the true corneal curvature of these aberrated corneas and the effective lens position in these patients. Multiple formulas, such as the Double-K Holladay 1 method and the Barrett True K formula have been proposed to improve the accuracy of IOL power calculations.[14]
Traumatic rupture of keratotomy scars
An increased risk of rupture from direct trauma exists as the cornea is weaker at the areas of the keratotomy incisions. Patients should be aware that their cornea is weakened from RK and avoid high- risk activities without appropriate eye protection.
Epithelial ingrowth
Corneal epithelial ingrowth can occur through a perforation. Management depends on the extent of the ingrowth. Epithelial ingrowth after LASIK performed on post- RK has been described, and fibrin glue may be helpful in preventing recurrence.[15]
Retinal detachment and maculopathy
Although cases of retinal detachment after refractive keratotomy have been reported, there is no evidence that this surgery predisposed to retinal detachment.
References
- ↑ Salz JJ: How safe is radial keratotomy? J Refrac Surg 3:188-189, 1987
- ↑ Marmer RH: Radial keratotomy complications. Ann Ophthalmol 19:409-411, 1987
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Rashid ER, Waring GO. Complications of radial and transverse keratotomy. Survey of Ophthalmology 1989;34:73-106.
- ↑ Jump up to: 4.0 4.1 4.2 Waring GO, Lynn MJ, Culbertson W, et al. Three-year Results of the Prospective Evaluation of Radial Keratotomy (PERK) Study. Ophthalmology 1987;94:1339-54.
- ↑ Waring GO, 3rd, Lynn MJ, McDonnell PJ. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol 1994;112:1298-308
- ↑ Waring GO, Lynn MJ, Gelender H, et al. Results of the Prospective Evaluation of Radial Keratotomy (PERK) Study One Year After Surgery. Ophthalmology 1985;92:177-307.
- ↑ Krachmer J, Mannis M, Holland E: CORNEA, 2nd ed.Elsevier Mosby, 2005, 1770-1780.
- ↑ Lynn MJ. Waring GO, Arentsen J, et al: Prospective Evaluation of Radial Keratotomy (PERK) Study: Results four years after surgery (abstract). Invest Ophthalmol Vis Sci (Suppl)29:310,1988
- ↑ Yeung KK, Olson MD, Weissman BA. Complexity of contact lens fitting after refractive surgery. Am J Ophthalmol 2002;133:607-12.
- ↑ Krachmer J, Mannis M, Holland E: CORNEA, 2nd ed.Elsevier Mosby, 2005, 1149-1161.
- ↑ Binder PS: Optical problems following refractive surgery. Ophthalmology 93:739-745, 1986
- ↑ Lewicky A, Salz J: Special report: Radial keratotomy survey. J Refrac Surg 2:32-33, 1986
- ↑ Santos CI: Herpes keratitis after radial keratotomy (Letter to the Editor). Am J Ophthalmol 93:370,1982
- ↑ Ma JX, Tang M, Wang L, Weikert MP, Huang D, Koch DD. Comparison of Newer IOL Power Calculation Methods for Eyes With Previous Radial Keratotomy. Investigative ophthalmology & visual science 2016;57:OCT162-8.
- ↑ Anderson NJ, Hardten DR. Fibrin glue for the prevention of epithelial ingrowth after laser in situ keratomileusis. Journal of Cataract & Refractive Surgery 2003;29:1425-9.