Pseudopapilledema
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Pseudopapilledema is defined as anomalous elevation of one or both optic discs without edema of the retinal nerve fiber layer[2]. Papilledema, on the other hand, is a swelling of the optic disc due to increased intracranial pressure. It is important to distinguish pseudopapilledema from true papilledema, which can be the first sign of disease process with the potential for vision loss, neurological impairment, or death. Patients thought to have papilledema are often subjected to lumbar puncture, MRI, and extensive laboratory studies to find the underlying cause. In this article, we will cover multiple causes of pseudopapilledema and how to differentiate them from true papilledema.
Etiology
Pseudopapilledema can be caused by a number of local and systemic processes.
Optic nerve head drusen
Optic nerve head drusen is the most common cause of pseudopapilledema, occurring in 0.34%-2.4% of individuals[3][4]. A complete review of optic disc drusen can be found on the optic disc drusen page. Drusen consists of extracellular deposits of calcium, hyaline, and other proteins caused by impaired axoplasmic flow resulting in extrusion of drusen or degeneration of the retinal ganglion cell nerve fiber axons[5]. Over time, the drusen can result in elevation of the optic nerve head. Deeper, “buried” drusen are not visible with fundoscopy and maybe difficult to differentiate from papilledema. Optic nerve head drusen can be inherited as part of a genetic syndrome with other ocular or systemic manifestations. For example, disc drusen may be associated with retinitis pigmentosa[3], Usher syndrome[3], pseudoxanthoma elasticum[3], angioid streaks[3], Noonan syndrome[3], Alagille syndrome[6], megalencephaly[3], and migraine headaches[3].
Congenital anomalies
Congenital anomalies of the optic disc may also mimic papilledema by causing portions of the disc to elevate. Myelinated nerve fibers refers to the atypical myelination of intraocular nerve fibers, occuring in 0.3-0.6% of the population by ophthalmoscopy[3]. The presence of myelin may elevate adjacent portions of the optic disc and obscure the disc margin and underlying retinal vessels, simulating papilledema. Hypoplastic optic discs are common and may be anomously elevated[3]. In tilted optic discs, a typically bilateral condition, the superotemporal optic disc is elevated, mimicking optic disc swelling, while the inferonasal disc is posteriorly displaced[3]. Bergmeister’s papillae is a congenital variant of the optic nerve in which an incompletely regressed hyaloid artery can obscure the optic nerve and give the impression of papilledema[5]. Epipapillary glial tissue may be associated with Bergmeister’s papillae and produce anterior traction that elevates the disc[7]. The morning glory disc anomaly is a congenital, typically unilateral funnel-shaped excavation of the posterior fundus that incorporates the optic disc, causing the disc to be markedly enlarged and appear elevated in some patients[3].
Small optic discs, 1.95 ± 0.33 mm3 (compared to normal optic disc size of 2.69 ± 0.70 mm3), can cause the appearance of pseudopapilledema[8]. In a crowded disc, a normal number of ganglion cell or optic nerve axons converge at a small optic disc to course through a smaller-than-average scleral canal, which can create indistinct margins. Small and crowded discs are commonly associated with hyperopia due to shortened axial length. Orbital hypotelorism has been associated with pseudopapilledema and situs inversus of the vessels[7].
Masses
Optic disc infiltration by neoplastic or inflammatory cells, or scleral infiltration, can cause elevation of the optic disc[3]. Peripapillary masses, such as astrocytic hamartomas, have been implicated[5].
Vitreopapillary traction
Vitreopapillary traction is characterized by traction of the optic disc due to different causes such as a fibrocellular membrane or an incomplete posterior vitreous detachment[9]. It usually occurs in conjunction with diabetes mellitus or other forms of retinovascular disease. Traction on the optic head can lead to elevation of the disc, obscuration of disc margins and peripapillary hemorrhage, and can therefore be mistaken for true optic disc swelling[9].
Systemic causes
Patients with Down syndrome can have optic disc elevation without obscuration of vessels[7]. Disc drusen has been noted as the cause in some cases[10]. However, patients with Down syndrome may develop true optic disc edema from pseudotumor cerebri or another etiology[7]. Therefore, optic disc elevation should not be presumed to be due to a benign condition until elevated intracranial pressure is ruled out by further workup[7].
Leber’s hereditary optic neuropathy can mimic papilledema in the acute phase, during which the optic disc may appear hyperemic and swollen[11]. There is no true disc edema in LHON[11]. Kenny syndrome, characterized by dwarfism, hypocalcemia, and tetany, can present with pseudopapilledema from a number of causes, including high hyperopia, crowded disc, and optic disc drusen[7]. Linear nevus sebaceous syndrome has been associated with pseudopapilledema[7]. Pseudopapilledema without drusen has been described in several cases of Alagille syndrome (arteriohepatic dysplasia)[7].
Diagnosis
History
A thorough history is key to distinguish papilledema, pseudopapilledema, and bilateral optic disc swelling without increased intracranial pressure. Patients with true papilledema will often present with progressive headaches, nausea, vomiting, and other neurologic symptoms such as positional headaches, transient visual obscurations (TVOs), pulsatile synchronous tinnitus, and binocular diplopia[5]. A history of headaches unrelieved by analgesics or nighttime awakening could raise the suspicion for increased ICP[12]. The possibility of pseudopapilledema can be considered in a patient with apparent optic disc swelling and no clinical symptoms or signs of increased intracranial pressure. Occasionally, patients with ODD will notice transient visual obscurations due to transient ischemia from vascular compression by the space-occupying lesion, but other symptoms of increased pressure will be absent. Patients with pseudopapilledema may also present with clinical findings indicative of a systemic process, as with Down syndrome, Alagille syndrome, and Kenny syndrome. To assess for bilateral optic disc swelling without increased intracranial pressure, questions could be asked about a recent history of a rash, tick bite, or migrating musculoskeletal pain (i.e., Lyme disease), risk of sexually-transmitted disease (i.e., syphilis) and a history of cat scratches (i.e., cat scratch disease), and a recent viral illness (i.e., optic neuritis)[12].
Physical examination
A thorough physical exam can be used to distinguish true papilledema from pseudopapilledema.
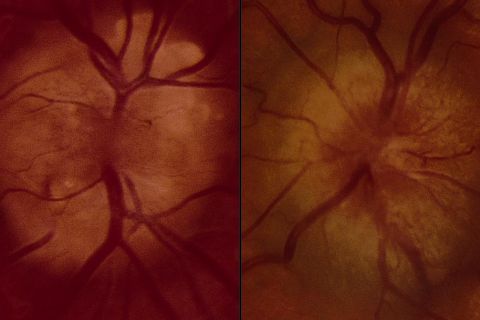
Fundoscopic examination
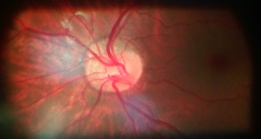
The distinction between true papilledema and pseudopapilledema can sometimes be made on the basis of ophthalmoscopic findings[13]. In true papilledema, swelling of the peripapillary nerve fiber layer causes an obscured view of underlying retinal vessels. The appearance of vessels in the peripapillary nerve fiber layer is the most important distinguishing feature between pseudopapilledema and papilledema[13]. Splinter hemorrhages may also be seen in true papilledema. Spontaneous venous pulsations (SVPs), a reassuring sign that there is no raised intracranial pressure, may also indicate pseudopapilledema[5]. However, SVPs may be absent in up to 10% of normal individuals[11]. Peripapillary subretinal hemorrhages often signify pseudopapilledema[13]. Optic disc drusen may show a “lumpy bumpy” disc appearance with visible retinal vessels.
Diseases associated with optic disc drusen may present with characteristic physical exam findings. For example, patients with retinitis pigmentosa may have waxy pallor of the nerve, attenuated vessels, and peripheral bone spicules; patients with pseudoxanthoma elasticum can have angioid streaks and peau d’orange skin changes; and patients with Alagille syndrome will present with a characteristic facial appearance[5].
Vision
Depending on the etiology, patients with pseudopapilledema may present with visual field deficits. Peripheral visual field defects develop in the majority (71-75%) of eyes with disc drusen, and they are commonly asymptomatic[3][5]. Congenital anomalies of the optic nerve can also produce characteristic patterns of visual field loss; for example, tilted disc syndrome can present with bitemporal hemianopia, myelinated nerve fibers may cause relative scotomas, and optic nerve hypoplasia can present with visual acuity ranging from 20/20 to no light perception, with affected eyes showing visual field deficits[3].
In contrast, in patients with papilledema, sometimes the only abnormality is mild to moderate enlargement of the physiologic blind spot[3]. In patients with severe papilledema, visual field deficits are common[3]. Most patients with severe papilledema have visual dysfunction, including decreased color vision, visual field defects, and abnormal contrast sensitivity[3]. Visual acuity may be affected last[3].
Diagnostic procedures
A-scan and B-scan ultrasonography
B-scan ultrasonography may show a hyperechoic signal corresponding to disc drusen. It can also allow for confirmation of vitreopapillary traction[3]. In patients with papilledema, B-scan ultrasonography will show a distended optic nerve sheath.
The 30-degree test
A-scan combined with B-scan can be used to measure change in optic nerve sheath diameter (ONSD) with the eye in various positions (e.g., in primary gaze versus 30 degrees of gaze). When the eye rotates to the 30 degree eccentric gaze position, the CSF fluid within the sheath redistributes itself posteriorly, reducing the ONSD. Usually a reduction of ONSD of more than 10% from primary position to 30 degrees from fixation is considered positive for fluid in the sheath and a marker of potential increased ICP.
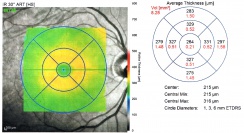
Optical coherence tomography (OCT)
OCT can demonstrate fluid accumulation in papilledema. It can also show the presence of vitreous traction on the optic nerve. Drusen will appear as hyporeflective masses with hyperreflective borders on EDI-OCT, and there are some suggestions that EDI-OCT might be the most sensitive testing modality for optic disc drusen. Small hyperreflective bands have been seen on OCT and are believed to represent nascent optic disc drusen.[14] In pseudopapilledema, an OCT may show a “lumpy-bumpy” internal contour while in true papilledema the internal contour is smooth. OCT in papilledema can show thickening of the peripapillary retinal nerve fiber layer and thinning of the macular ganglion cell complex.[15] Peripapillary hyper-reflective ovoid mass-like structure (PHOMS) can sometimes be observed in patients with pseudopapilledema, however PHOMS may also be seen in a wide variety of conditions (including papilledema).
Optical Coherence Tomography Angiography (OCTA)
OCTA is a rapid form of non-invasive imaging of peripapillary and macular vascular structures. OCTA can potentially be used to differentiate pseudopapilledema with papilledema, as eyes with pseudopapilledema typically have a lower vessel density.[15]
Fluorescein angiography (FA)
Intravenous fluorescein angiography is one of the best tests for the diagnosis of true optic disc edema, although it is typically only used in cases where other testing is equivocal[5][16]. Capillary leakage will be present in papilledema, but not in pseudopapilledema[11]. In patients with optic disc drusen, FA will show a true nodular hyperfluorescence corresponding to the location of the visible drusen.
Lumbar puncture
Pseudopapilledema will reveal normal opening pressure, as opposed to elevated pressure in true papilledema. Lumbar puncture can also be used to evaluate for neoplastic invasion of the optic nerve head. CSF cell count, protein, and glucose may show signs of infection or inflammation.
Magnetic resonance imaging (MRI) and Magnetic resonance venography (MRV)
When suspecting true papilledema, MRI of the brain and orbit with and without contrast including fat suppression sequences could be ordered. Infiltration by neoplastic cells will be evident on MRI as an enhancement. MRI will also detect a mass causing true papilledema or enlargement of the ventricles. In a patient with papilledema and high intracranial pressure, high resolution MRI will show distended subarachnoid space, widened optic nerve sheath, empty sella and flattening of the posterior globe. MRV is recommended in suspected papilledema to evaluate for dural venous sinus thrombosis.
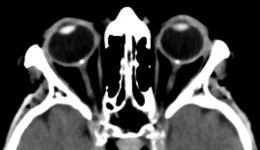
Computed tomography (CT)
Optic disc drusen will show calcifications on CT, although it is not routinely used for diagnosis. CT may also detect a mass causing true papilledema or enlargement of the ventricles.
Laboratory or serologic testing
Laboratory testing may be ordered to evaluate for infection or toxic/metabolic causes of bilateral disc swelling.
Differential diagnosis
The differential diagnosis of pseudopapilledema includes causes of true papilledema and causes of optic disc swelling without increased intracranial pressure.
Causes of papilledema[11]:
- Expanding mass lesion (e.g. brain tumor)
- Cerebral edema due to stroke
- Intracranial hemorrhage
- Compression of the ventricular system in the posterior fossa
- Venous sinus thrombosis
- Infectious etiology (e.g. cryptococcal meningitis)
- Pseudotumor cerebri
Causes of bilateral optic disc edema without raised intracranial pressure:
- Hypertensive emergency[11]
- Diabetic papillopathy[11]
- Toxic insult[11]
- Metabolic or nutritional deficiency[11][12]
- Optic perineuritis (caused by infectious or inflammatory conditions)[3]
- Other causes: optic neuritis, ischemia, compression from orbital tumors
Management
Distinguishing papilledema from pseudopapilledema can be tricky, but is important to avoid invasive and unnecessary workup for increased intracranial pressure. Anomalies suggestive of pseudopapilledema can be suspected when any elevated, noncongested disc is seen with no physiologic cup, and with nondilated veins and arteries passing over its surface[2]. Patients with optic disc anomalies are recommended to be evaluated frequently by an ophthalmologist, who will monitor for changes such as hemorrhages of the disc or enlargement of scotomas[2]. If the disc anomalies are unchanging and pseudopapilledema is established, the patient can be informed about that to avoid future medical confusion. Management of pseudopapilledema varies by etiology[5]. Patients with systemic disorders should be managed appropriately for their symptoms.
Additional Resources
References
- ↑ American Academy of Ophthalmology. Pseudopapilledema and papilledema. https://www.aao.org/image/pseudopapilledema-papilledema-2 Accessed May 26, 2020.
- ↑ Jump up to: 2.0 2.1 2.2 Hoyt, WF, Pont, ME. Pseudopapilledema: Anomalous Elevation of the Optic Disk. JAMA. 1962;181(3):191-196. doi:10.1001/jama.1962.03050290013003
- ↑ Jump up to: 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 Miller, NR, Newman, NJ, Biousse, V, Kerrison, JB, et al. Walsh and Hoyt’s Clinical Neuro-Ophthalmology Sixth edition. 2005;1(6).
- ↑ Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002;47(6):515-32
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Freund P, Margolin E. Pseudopapilledema. StatPearls Publishing. 2019 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538291/
- ↑ El-Koofy NM, El-Mahdy R, Fahmy ME, et al. Alagille syndrome: clinical and ocular pathognomonic features. Eur J Ophthalmol. 2011;21(2);199-206.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Brodsky, MC. Pediatric neuro-ophthalmology, third edition. Springer New York. 2016. https://doi.org/10.1007/978-1-4939-3384-6
- ↑ Chiang, J, Wong, E, Whatham, A, et al. The usefulness of multimodal imaging for differentiating pseudopapilloedema and true swelling of the optic nerve head: a review and case series. Clinical and Experimental Optometry. 2015;98(1):12-24.
- ↑ Jump up to: 9.0 9.1 Houle, E, Miller, NR. Bilateral Vitreopapillary Traction Demonstrated by Optical Coherence Tomography Mistaken for Papilledema. Case Reports in Ophthalmological Medicine. 2012. https://doi.org/10.1155/2012/682659.
- ↑ Schneier A, Heidary G, Ledoux D. Optic Nerve Appearance in Patients With Down Syndrome. J Pediatr Ophthalmol Strabismus. 2013; 50: 60. doi: 10.3928/01913913-20121214-01
- ↑ Jump up to: 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 11.8 Prasad, S, Volpe, NJ, Balcer, LJ. Approach to Optic Neuropathies. The Neurologist. 2010;16(1):23-34.
- ↑ Jump up to: 12.0 12.1 12.2 Lee, AG, Beaver, HA. Acute Bilateral Optic Disk Edema with a Macular Star Figure in a 12-Year-Old Girl. Survey of Ophthalmology. 2002;47(1):42-29.
- ↑ Jump up to: 13.0 13.1 13.2 Balcer, LJ, Prasad, S. Chapter 15: Abnormalities of the Optic Nerve and Retina. From Beck, RW, Smith, CH. Neuro-Ophthalmology: A Problem-Oriented Approach. 1988.
- ↑ Fraser JA, Bursztyn LLC. Optical coherence tomography in optic disc drusen. Ann Eye Sci 2020;5:5.
- ↑ Jump up to: 15.0 15.1 Fard MA, Sahraiyan A, Jalili J, et al. Optical Coherence Tomography Angiography in Papilledema Compared With Pseudopapilledema. Invest Ophthalmol Vis Sci. 2019;60(1):168-175. doi:10.1167/iovs.18-25453
- ↑ Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol. 2012;32(1):17–22. doi:10.1097/WNO.0b013e31823010b8