Pseudoexfoliative Glaucoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Summary
Pseudoexfoliative syndrome (PXF/PEX) is a systemic condition characterized by the deposition of a protein-like material within the anterior segment of the eye, most notably on the anterior lens capsule, and other organs. Both genetic and environmental factors may play a role in its pathogenesis. It is commonly seen in older individuals and within certain ethnicities. This condition may present unilaterally and bilaterally and is known to be a major risk factor for secondary open angle glaucoma. Pseudoexfoliative glaucoma is seen in up to 50% of eyes with PXF. In contrast to POAG, this disease runs a more aggressive clinical course with high IOP at onset, faster rates of progression, poor response to medical therapy, and increased need for surgical intervention. This brief review will discuss the pathophysiology, clinical course and signs, differential diagnosis, and treatment strategies of this disease
Disease Entity
- Pseudoexfoliation Syndrome and Exfoliative Syndrome are used interchangeably
- Pseudoexfoliative Glaucoma(PXG) and Exfoliative Glaucoma are used interchangeably
Disease
Pseudoexfoliation syndrome (PXF/PEX) is a systemic condition characterized by the deposition of white dandruff-like material, called exfoliation material, within the anterior segment of the eye and other organs such as the heart, lungs and kidneys. The deposition of this material in the trabecular meshwork can result in aqueous outflow obstruction, raised intraocular pressure (IOP) and glaucoma. In fact, pseudoexfoliative glaucoma is the most common form of secondary open angle glaucoma. Not all patients with PXF develop glaucoma and it is difficult to predict which patients are more susceptible. Approximately 20% of patients with newly diagnosed exfoliation have either glaucoma or increased IOP.
Overall, 50% of patients with exfoliation syndrome are ultimately diagnosed with glaucoma. Patients with PXF glaucoma tend to present with advanced visual field loss and cupping. This is in part due to the fact that it is often unilateral and slowly progressive. Recent evidence also suggests that the rate of progression in PXF glaucoma is greater than in primary open angle glaucoma (POAG) or normal tension glaucoma (NTG). The term true exfoliation or capsular delamination refers to a separation of superficial layers of the lens capsule from the deeper layers as a result of heat or infrared radiation. Glaucoma is not common feature of true exfoliation or capsular delamination.
Etiology
Recent genetic studies (first in Iceland, and subsequently in the United States, Germany, Italy and South Africa) have greatly advanced our understanding of the etiology of PXF. The lysyl oxidase-like protein 1 (LOXL1) gene is important for elastin metabolism. Defects in elastin metabolism have been postulated to result in synthesis of pseudoexfoliative material. It has been found that single nucleotide polymorphisms in the LOXL1 gene are strongly associated with the development of PXF and secondary glaucoma. However, the risks alleles are not consistent between populations. The high-risk alleles seen in Icelandic and USA populations were protective in a South African population. To date no risk allele has been identified that is consistent across all populations. Also, within a population the majority of people carrying the high-risk alleles do develop PXF, suggesting that other factors contribute to the onset of disease.
Risk Factors
The following have been shown to be risk factors for PXF:
- Older age (most cases occurring in late 60s and 70s)
- Scandinavian and Mediterranean race
Pathophysiology
Pseudoexfoliative material can be identified pre-clinically with transmission electron microscopy which shows fibrillar elastotic material. Histochemically, pseudoexfoliative material is glycoconjugates surrounding a protein core. These aggregates are synthesized intracellularly in multiple different cell types in the anterior segment including non-pigmented ciliary epithelial cells, trabecular endothelial cells and pre-equatorial lens epithelial cells. This is thought to be a result of oxidative stress. The material is then released into the extracellular space and deposited around the cells that produced the material, and also other structures such as the zonules, pupillary margin and anterior lens surface. The accumulation of pseudoexfoliative material in the extracellular matrix of tissues results in altered metabolism and hence disturbed structure and function. The trabecular meshwork becomes clogged resulting in reduced aqueous outflow, raised IOP and secondary glaucoma. Excessive pigment liberation seen in these eyes may be the result of fundamental defect in the iris or may be liberated from the iris as a result of rubbing of iris pigment epithelium against the rough lens capsule. The blockage of trabecular spaces by pigment may also be a contributing facor for secondary glaucoma. It remains unclear why some eyes are more likely to develop glaucoma compared with others. It may be due to the amount of pseuoexfoliative material present, and that metabolic activities (including synthetic and digestive enzymes) of the trabecular meshwork may vary among patients. It may also be that juxtacanalicular tissue porosity and composition( collagen and extracellular matrix) may vary among patients.
Zonules become weak, which can result in lens instability and dehiscence. Accumulation in the iris tissue results in poor pupillary dilatation and impairment of the blood-aqueous barrier. The combination of all these features makes cataract surgery in patients with PXF more difficult, with an increased incidence of complications and postoperative inflammation.
Primary Prevention
At present, there are no strategies for primary prevention of PXF. However, awareness of PXF can help prevent the complications of PXF. IOP should be monitored annually in patients with PXF and no signs of glaucoma. This would allow early treatment and prevention of glaucoma, or at least reduced risk of developing advance glaucoma. PXF should be carefully looked for in anyone undergoing cataract surgery. Extra precautions may then be taken to minimize the risk of operative complications.
Diagnosis
The diagnosis of PXF is primarily clinical.
History
The majority of patients are asymptomatic, and PXF is often an incidental finding. It is not uncommon for patients with PXF glaucoma to present with advanced disease in one eye, in which case they may have become aware of a gradual reduction in vision. Rarely, there is an acute rise in IOP which may cause symptoms of ocular pain, blurring of vision and seeing haloes.
Signs
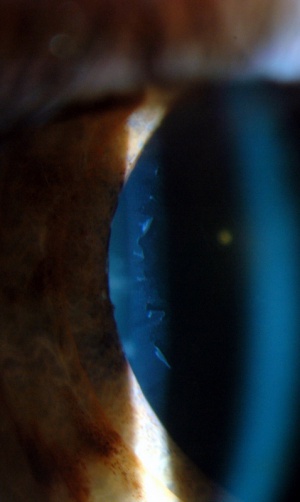
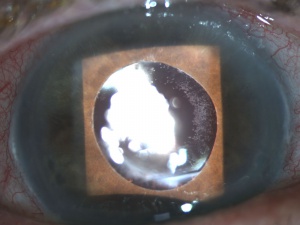
The classic sign of PXF is the visualization of white pseudoexfoliative material on the pupil margin and on the anterior lens surface (with a clear intermediate zone due to rubbing off by the iris). This is most easily seen after dilatation, and is therefore sometimes overlooked (Figures 1-6). Approximately 20% of the cases can be missed in undilated eyes. The material may be seen on the conjunctiva, corneal endothelium, lens zonules, ciliary processes, and trabecular meshwork. In pseudophakic and aphakic eyes, it may be deposited on intraocular lens and the vitreous face, respectively.
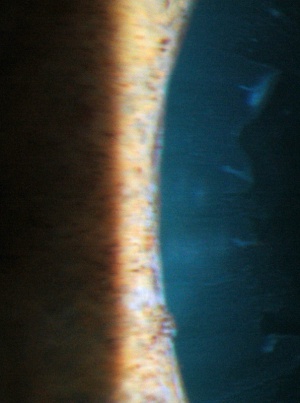
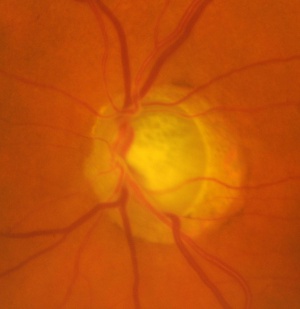
Photos Courtesy of Anthony Khawaja, MBBS, Royal Free Hospital,London, UK and Sarwat Salim, MD, FACS, University of Tennessee, Memphis, TN, USA
Figure 1: Left eye of a patient with PXF glaucoma. Note the the white pseudoexfoliative material on the central anterior lens capsule, surrounded by a clear zone (caused by iris rubbing)
Figure 2: Left eye of a patient with PXF glaucoma. Note the white pseudoexfoliative material on the periphery of the lens capsule and the inner clear zone caused by iris rubbing. This would not be visualized through an undilated pupil.
Figure 3: Left eye of a patient with PXF glaucoma. Note the pseudoexfoliative material on the pupil margin.
Figure 4: Increased and uneven trabecular meshwork pigmentation in PXF.
Figure 5: Pseudoexfoliative material on pupillary margin.
Figure 6: Pseudoexfoliative material on intraocular lens.
Peripupillary iris transillumination and pigmented ruff atrophy may be seen. Pupil dilatation is often poor. Flourescein angiography and ultrastructural studies have shown hypoxia of the the iris, and hypoperfusion may be a factor in development of exfoliation syndrome. Hypoxia can cause atrophy of the iris pigment epithelium , stroma, and muscles.
Gonioscopy most commonly reveals an open anterior chamber drainage angle. Unlike pigmentary glaucoma, there appears to increased, but uneven TM pigment distribution. The melanin dispersion is from atrophy of the iris pigment epithelium. Actual pseudoexfoliative material may be noted on the TM. Another feature of the angle is the presence of pigment anterior to Schwalbe’s line, known as Sampaolesi’s line. In unilateral cases, it is important to pay attention to increased TM pigmentation in the fellow eye without signs of exfoliation because this may be earliest detectable sign of disease process in the contralateral eye. Although most eyes with pseudoexfoliation syndrome or glaucoma have open angles, approximately 9-18% of eyes can have occludable angles and patients may develop an acute attack of angle closure glaucoma.This may be due to zonular laxity leading to anterior displacement of the iris-lens diaphragm and secondary angle closure. One way of distinguishing this from primary angle closure is the relatively deep anterior chamber on the other (likely less affected) side. There may be associated phacodonesis. Other evidence of narrow angle includes Iris bombe configuration,posterior synechiae, and vossius ring on the lens capsule
Nuclear sclerotic cataract is more common in patients with PXF.
In eyes with secondary raised IOP, there may be the usual signs of glaucomatous optic neuropathy (Figure 7).
Figure 7: Left eye of a patient with PXF glaucoma. Note the classic appearances of glaucomatous optic neuropathy including a large cup:disc ratio, nasally displaced vessels and beta-zone peripapillary atrophy.
Differential diagnosis
The differential diagnosis includes:
- POAG
- Primary angle-closure glaucoma (PACG)
- Pigment dispersion syndrome (PDS)
- True exfoliation or capsular delamination
- Amyloidosis
PXF glaucoma may be misdiagnosed as POAG if the pseudoexfoliative material is overlooked. It is important to distinguish these conditions, as PXF glaucoma may need to be followed more closely and treated more aggressively as it is known to progress more rapidly. Patients with exfoliation syndrome do not have the same response to topical corticosteroids as do chronic open angle glaucoma patients. Also on histology, eyes with PXFdo not have excess tendon sheath/plaque material compared to eyes with POAG. These differences indicate that it is a separate entity from POAG. In cases of PXF with secondary angle closure due to zonular laxity, the key to distinguishing it from PACG is the asymmetry in anterior chamber depth, as well as the presence of pseudoexfoliative material. It is very important to distinguish between the two conditions, as the treatment is different. Miotic drops may exacerbate angle closure secondary to PXF. PDS is more common in younger, myopic patients, and is often bilateral. The pattern of iris transillumination and angle pigmentation is different (see section Pigmentary Glaucoma). Glaucoma is rare with true exfoliation or capsular delamination. Amyloid material may appear white and flaky and be deposited in the anterior segment, but this condition is less common and systemic manifestatons are often present.
Management
The only proven treatment for glaucoma is lowering of IOP. This is true for PXF glaucoma. The aim is to prevent or slow down further glaucomatous optic nerve damage.
Medical therapy
Medical therapy for PXF glaucoma is more difficult when compared with treatment for POAG. Although the IOP reduction may be greater initially with a chosen agent, the 24 hour IOP characteristics and high IOP fluctuations make it more challenging to reach the predetermined target pressure. As a result, adjunctive therapy with other medications or laser treatment is often necessary. These patients also require earlier surgical intervention due to medically uncontrolled glaucoma.
Medical therapy for PXF secondary angle-closure is different than PACG if the underlying problem is zonular laxity. Dilating drops (e.g. atropine) are required as opposed to miotics.
Surgery
Laser trabeculoplasty has been reported to be particularly effective in PXF glaucoma, due to the relatively pigmented angles. However, the duration of IOP lowering is limited with more than half of patients failing after 5 years. Please see the section Laser Trabeculoplasty: ALT vs SLT.
Cataract surgery is often required in patients with PXF due to the increased incidence. There is also an increased risk of complications due to poor pupil dilatation and zonular weakness. Vitreous loss is 5-10 times more common in these eyes. Slow and gentle surgery, possibly with the aid of capsular staining and iris hooks, is required. The hooks may help with small pupils, and may also be placed into the capsular bag in cases with zonular laxity. A primary chopping technique may reduce stress on already weak zonules. Insertion of a capsular tension ring may reduce the risk of intra-operative and late post-operative intraocular lens / bag dislocation. A larger capsulorhexis should be made at the time of surgery to prevent anterior capsule opacification and contraction. These eyes are more likely to develop postoperative inflammation and posterior capsule opacification.
There is also a higher complication rate for trabeculectomy in patients with PXF glaucoma compared with POAG. However, success rates are similar. Given the increased incidence of cataract, combined cataract and glaucoma surgery is sometimes considered (see Techniques for Combined Cataract and Glaucoma Surgery).
Prognosis
Overall, 50% of patients with PXF are ultimately diagnosed with glaucoma.
Therefore annual assessment is required. Patients who do develop PXF glaucoma are thought to have a worse prognosis than patients with POAG, with faster rates of progression, poorer response to medications and an increased need for surgery.
References
- Denniston A, Murray P. Oxford Handbook of Ophthalmology. Oxford, United Kingdom: Oxford University Press; 2006:276-277.
- Rhee D. Glaucoma: Color Atlas and Synopsis of Clinical Ophthalmology. New York, NY: McGraw-Hill; 2002:204-229.
- Schacknow P, Samples J. The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care. New York, NY: Springer; 2010:399-420.
- Stamper R, Lieberman M, Drake M. Becker-Shaffer’s Diagnosis and Therapy of the Glaucomas. 8th Edition. New York, NY: Mosby; 2009:239-265.