Positive and Negative Pressure Goggles for Ophthalmic Diseases
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Overview on Intraocular Pressure, Intracranial Pressure, and Translaminar Pressure Gradient
Intraocular Pressure and Intracranial Pressure
Glaucoma is a leading cause of irreversible vision loss and is characterized by the progressive loss of retinal ganglion cells. The loss of retinal ganglion cells presents clinically as optic nerve head structural changes (“cupping”) and visual field loss. The lamina cribrosa is a connective tissue structure through which retinal ganglion cell axons pass to exit the eye and it is believed to be the main site of retinal ganglion cell axonal injury in glaucoma [1]. Elevated intraocular pressure (IOP) is a risk factor for glaucoma, however several studies found that IOP was within the “normal” range in 25-50% of individuals with glaucoma in the US [2]. Currently, the only proven method to treat the disease is by reducing IOP, either medically (e.g., topical eye drops) or surgically [3].
Signs and symptoms of increased intracranial pressure (ICP) include papilledema, transient visual obscuration, vision loss, double vision, headache, and pulsatile tinnitus [4]. Signs and symptoms of low ICP include orthostatic headache, vertigo, neck pain, emesis, and horizontal diplopia [5][6].
Translaminar Pressure Gradient and Cerebrospinal Fluid Theory of Glaucoma
The lamina cribrosa is influenced by two separate pressures- the ICP (acting anteriorly) and the IOP (acting posteriorly). The translaminar pressure gradient is the difference between these two pressures. Due to pressure changes, lamina cribrosa deforms anteriorly in IIH and posteriorly in glaucoma [7]. The impact of the circadian IOP rhythm on the progression of glaucoma remains unclear. Recent evidence suggests that an imbalance between the IOP and ICP (translaminar pressure gradient) plays a role in glaucoma development [7]. It has been hypothesized that intervals of regulating the translaminar pressure gradient may protect the optic nerve and stopping glaucoma progression.
The Role of Intraocular Pressure and Intracranial Pressure in Spontaneous Venous Pulsations
Spontaneous venous pulsation (SVP) is a pulsation of the central retinal vein which can occur in both physiological and pathological states. The SVPs can be observed with an ophthalmoscope. They are more prominent than pulsation of retinal artery. SVPs’ prevalence across individuals ranges between 87.6% [8] and 98% [9], and is decreased in glaucoma patients [10]. It is theorized that the ultimate origin of pulsation is the cardiac cycle which drives the pulsation of cerebrospinal fluid (CSF) which in turn acts as a wave generator for SVP. Indeed, the CSF pulsation causes oscillations of transmural pressure, or the difference between the IOP and retinal venous pressure [11][12].
The SVP is visible when the central retinal vein’ volume changes appreciably. For this to occur the vessel must be compliant. Compliance is a function of a vessel's volume, and it decreases at high volumes [12]. This decrease in compliance physiologically serves as a rupture preventing mechanism. When a transmural pressure oscillation occurs at high retinal vein fill volumes then the vessel will be non-compliant and the SVP will not be appreciable [12][13]. Alternatively, when an oscillation occurs across a compliant vessel, the SVP is more appreciable. Interestingly, although compliance is necessary it is not sufficient for the SVP to appear - indeed when the CSF pulsation is not transmitted to the retinal vein then the SVP will not be visible even in a compliant vessel.
The venous pulsation pressure (VPP) is the minimal IOP at which the central retinal vein’s volume is low enough for it to be compliant and thus pulsate visibly in response to CSF pulsations [14]. The rationale behind this is that IOP increases the pressure gradient between the blood in the retinal veins and the cavernous sinus thus lowering the retinal vein’s volume. As IOP decreases, more blood fills the retinal vein, increasing the volume in the vein and reducing compliance. Conversely, as IOP increases less blood is able to fill the retinal vein, volume decreases, and compliance increases.
SVP and VPP can be used as an ophthalmic biomarker of pathological states, including raised ICP [15], glaucoma and possibly spaceflight associated neuro-ocular syndrome (SANS), a neuro-ophthalmic phenomenon seen in astronauts after long-duration spaceflight [16]. Patients with raised ICP have been found to be less likely to have SVPs [15]. The two changes are thought to be caused by increased blood pressure inside the retinal vein which in turn increases the vessel’s volume beyond the range of compliance [13].
Patients with glaucoma have been found to be less likely to have SVP than non-glaucoma patients [10]. Moreover, the VPP tends to be higher in glaucoma patients [17]. The two changes are thought to be caused by increased resistance of the central retinal vein at the level of lamina cribrosa which both attenuates transmission of CSF pulsation and increases the retinal vein’s volume upstream of sclera causing the retinal venous system to become non-compliant [10]. The VPP level is thought to be predictive of disease progression [18].
Introduction to Pressurized Goggles
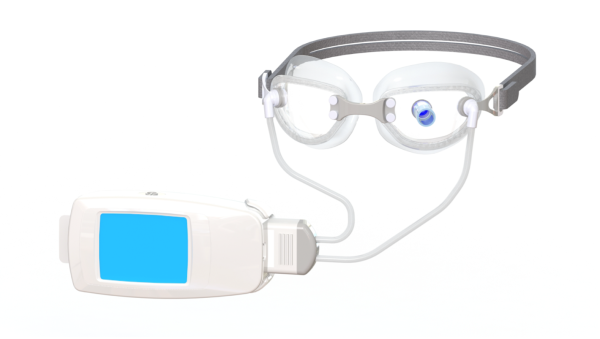
IOP varies in a diurnal pattern, with the highest magnitude measured at night. When IOP increases, ocular perfusion decreases. This is especially important for ophthalmic diseases such as glaucoma [19]. With the help of negative pressure goggles (NPGs), IOP can be lowered non-pharmacologically and non-invasively. For instance, -10 mmHg applied via NPG over the orbit by way of a vacuum can lower intraocular pressure about 6 mmHg without affecting intracranial pressure [20][21]. Alternatively, by applying positive pressure, these goggles may be able to increase intraocular pressure, normalizing the translaminar pressure gradient in elevated ICP. Current research is being conducted on goggles that add vacuum or pressure around the orbital area [22]. This provides the unique opportunity to normalize the pressure differential associated with optic nerve diseases, including but not limited to glaucoma [23], IIH, and SANS. In this section, we discuss the development of pressurized goggles and current studies.
Goggle Specifications
Specifications:
- Goggles, consisting of:
- Lenses with silicone seals
- Tubing connecting the goggles to the pump
- Head strap for support
- Adjustable nose bridge between goggle lenses
- Small, medium, and large sizes to accommodate the variations in subject facial anatomy. The design and principles of action remain constant amongst all sizes. The differences in dimensions are illustrated above
- Pump (programmed by investigators or investigator staff), which creates negative pressure inside the goggles via tubing
Trials and Studies
Several trials have been conducted to highlight the efficacy of NPGs as a viable therapeutic option for ophthalmic diseases. Samuelson et al. demonstrated that NPGs had favorable safety parameters and the potential for sustained delivery of treatment that is well-tolerated by patients. In their study, -10 mmHg was applied to one eye and ambient atmospheric pressure was applied in the contralateral eye for 8 hours in 10 patients with open-angle glaucoma. At the conclusion of the study, patient tolerability was reported, as well as interest in NPGs as a potential glaucoma treatment. Mean tolerability was 1.8 ± 0.4 (scale → 1=best, 10 = worst) and there was a positive interest response of 1.8 ± 0.5 (scale → 1=best, 10 = worst) [20]. Additionally, it has been shown that the goggles can also be used to provide accurate IOP measurements. Ferguson, et al. demonstrated that pneumatonometry can be accomplished by the excursion test method which utilizes a Tono-Pen tip cover in conjunction with the NPGs to produce precise, accurate, and reproducible measurements of IOP. In this study, 480 paired IOP measurements, with and without a Tono-Pen cover, were collected across four pressure levels of 7, 10, 20 and 30 mmHg with results solidifying that pneumatonometry with a Tono-Pen cover, in concert with NPG, is an acceptable form of IOP measurement [24]. Finally, a study conducted by Swan, et al. illustrated that among 65 subjects randomized to receive either no negative pressure or negative pressure for 60 minutes at 25%, 50%, and 75% of baseline IOP, there was a clinically statistically significant reduction in IOPs at all negative pressure settings [25]. This opens the possibility for real-world applications for ophthalmic diseases.
Currently, ophthalmic drops, laser treatments, and surgical procedures are the therapies available to control IOP [21][23]. However, these the IOP lowering of these therapies are often unpredictable and can be marred by non-compliance in the case of eye drops [23]. With the use of NPG, a more targeted and finite approach to reducing IOP is available that is both accurate and well-tolerated by patients [20].
Overview of Spaceflight Associated Neuro-Ocular Syndrome and Future Potential Utilization of Positive Pressure Goggles
SANS refers to a constellation of neuro-ophthalmic findings that are observed in astronauts after long-duration spaceflight including optic disc edema, globe flattening, hyperopic refractive shift errors, and choroidal folds [26]. The pathogenesis of SANS is not well understood. However, several hypotheses have emerged involving cephalad fluid shifts, increased ICP, ocular glymphatic system congestion, upward brain shift, and cerebral volume pulsatility [26][27][28][29].
Swimming goggles have also been investigated as a mitigation strategy for SANS. Previous studies have seen that swimming goggles that directly push on the eye can artificially increase IOP [30]. Swimming goggles with direct pressure on the eye were placed on healthy individuals in head-down tilt, a terrestrial analog for SANS. The study found that the application of swimming goggles increased IOP and the translaminar pressure gradient during head-down tilt. The study authors suggest that the slight elevation of IOP may help to safely mitigate SANS, though further studies must be conducted to understand the safety of elevating IOP over extended periods of time. Positive pressure goggles may help to increase IOP more so than regular swimming goggles, thus providing another alternative to increase the translaminar pressure gradient [31].
Summary Paragraph
Pressurized goggles may manipulate the translaminar pressure gradient and serve as a potential treatment for several ophthalmic diseases such as glaucoma. By assessing for SVPs during pressure changes, these goggles may also allow for an indirect measurement of ICP. The application of positive pressure using goggles may provide benefit as a therapeutic strategy for astronauts during long-duration spaceflight. Further validation studies are required for this emerging technology.
References
- ↑ Abe RY, Gracitelli CP, Diniz-Filho A, Tatham AJ, Medeiros FA. Lamina Cribrosa in Glaucoma: Diagnosis and Monitoring. Curr Ophthalmol Rep. 2015;3(2):74-84. doi:10.1007/s40135-015-0067-7
- ↑ Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901-1911. doi:10.1001/jama.2014.3192
- ↑ Schuster AK, Erb C, Hoffmann EM, Dietlein T, Pfeiffer N. The Diagnosis and Treatment of Glaucoma. Dtsch Arztebl Int. 2020;117(13):225-234. doi:10.3238/arztebl.2020.0225
- ↑ Pinto VL, Tadi P, Adeyinka A. Increased Intracranial Pressure. [Updated 2021 Sep 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482119/
- ↑ Foltz EL, Blanks JP. Symptomatic low intracranial pressure in shunted hydrocephalus. J Neurosurg. 1988 Mar;68(3):401-8. doi: 10.3171/jns.1988.68.3.0401. PMID: 3343612.
- ↑ Lay CM. Low Cerebrospinal Fluid Pressure Headache. Curr Treat Options Neurol. 2002 Sep;4(5):357-363. doi: 10.1007/s11940-002-0046-9. PMID: 12162924.
- ↑ Jump up to: 7.0 7.1 Berdahl JP, Ferguson TJ, Samuelson TW. Periodic normalization of the translaminar pressure gradient prevents glaucomatous damage. Med Hypotheses. 2020;144:110258. doi:10.1016/j.mehy.2020.110258
- ↑ Levin, B. E. The Clinical Significance of Spontaneous Pulsations of the Retinal Vein. Archives of Neurology 35, 37–40 (1978).
- ↑ Morgan, W. H. et al. Retinal venous pulsation in glaucoma and glaucoma suspects. Ophthalmology 111, 1489–1494 (2004).
- ↑ Jump up to: 10.0 10.1 10.2 Abegão Pinto, L., Vandewalle, E., De Clerck, E., Marques-Neves, C. & Stalmans, I. Lack of spontaneous venous pulsation: possible risk indicator in normal tension glaucoma? Acta Ophthalmologica 91, 514–520 (2013).
- ↑ Meyer-Schwickerath, R., Kleinwächter, T., Papenfuß, H.-D. & Firsching, R. Central retinal venous outflow pressure. Graefe’s Arch Clin Exp Ophthalmol 233, 783–788 (1995).
- ↑ Jump up to: 12.0 12.1 12.2 Moreno, A. H., Katz, A. I., Gold, L. D. & Reddy, R. V. Mechanics of Distension of Dog Veins and Other Very Thin-Walled Tubular Structures. Circulation Research 27, 1069–1080 (1970).
- ↑ Jump up to: 13.0 13.1 Morgan, W. H. et al. Retinal Artery and Vein Pressures in the Dog and Their Relationship to Aortic, Intraocular, and Cerebrospinal Fluid Pressures. Microvascular Research 53, 211–221 (1997).
- ↑ Morgan, W. H., Hazelton, M. L. & Yu, D.-Y. Retinal venous pulsation: Expanding our understanding and use of this enigmatic phenomenon. Progress in Retinal and Eye Research 55, 82–107 (2016).
- ↑ Jump up to: 15.0 15.1 Walsh, T. J., Garden, J. W. & Gallagher, B. Obliteration of Retinal Venous Pulsations: During Elevation of Cerebrospinal-Fluid Pressure. American Journal of Ophthalmology 67, 954–956 (1969).
- ↑ Mader, T. H. et al. Unilateral Loss of Spontaneous Venous Pulsations in an Astronaut. Journal of Neuro-Ophthalmology 35, 226–227 (2015).
- ↑ Jonas, J. B. Central retinal artery and vein collapse pressure in eyes with chronic open angle glaucoma. Br J Ophthalmol 87, 949 (2003).
- ↑ Balaratnasingam, C. et al. Value of retinal vein pulsation characteristics in predicting increased optic disc excavation. Br J Ophthalmol 91, 441 (2007).
- ↑ Konstas AG, Kahook MY, Araie M, et al. Diurnal and 24-h Intraocular Pressures in Glaucoma: Monitoring Strategies and Impact on Prognosis and Treatment. Adv Ther. 2018;35(11):1775-1804. doi:10.1007/s12325-018-0812-z
- ↑ Jump up to: 20.0 20.1 20.2 Samuelson TW, Ferguson TJ, Radcliffe NM, et al. 8 hrs Safety Evaluation Of A Multi-Pressure Dial In Eyes With Glaucoma: Prospective, Open-Label, Randomized Study. Clin Ophthalmol. 2019;13:1947-1953. Published 2019 Oct 2. doi:10.2147/OPTH.S217736
- ↑ Jump up to: 21.0 21.1 Chu N, Brambilla E, Yoo P, Ferguson TJ. Evaluation of negative pressure transfer through tissue in a benchtop cornea and eyelid model. Ther Adv Ophthalmol.
- ↑ National Space Biomedical Research Institute. Equinox Balance Goggles: The Effects of Local Orbital Pressure Changes on Intraocular Pressure. http://nsbri.org/researches/equinox-balance-goggles-the-effects-of-local-orbital-pressure-changes-on-intraocular-pressure/
- ↑ Jump up to: 23.0 23.1 23.2 Sheybani A, Scott R, Samuelson TW, et al. Open-Angle Glaucoma: Burden of Illness, Current Therapies, and the Management of Nocturnal IOP Variation. Ophthalmol Ther. 2020;9(1):1-14. doi:10.1007/s40123-019-00222-z
- ↑ Ferguson, T.J., Knier, C.G., Chowdhury, U.R. et al. Intraocular Pressure Measurement with Pneumatonometry and a Tonometer Tip Cover. Ophthalmol Ther 9, 127–137 (2020). https://doi.org/10.1007/s40123-020-00235-z
- ↑ Swan RJ, Ferguson TJ, Shah M, et al. Evaluation of the IOP-Lowering Effect of a Multi-Pressure Dial at Different Negative Pressure Settings. Transl Vis Sci Technol. 2020;9(12):19. Published 2020 Nov 13. doi:10.1167/tvst.9.12.19
- ↑ Jump up to: 26.0 26.1 Lee, A.G., Mader, T.H., Gibson, C.R. et al. Spaceflight associated neuro-ocular syndrome (SANS) and the neuro-ophthalmologic effects of microgravity: a review and an update. npj Microgravity 6, 7 (2020). https://doi.org/10.1038/s41526-020-0097-9
- ↑ Wostyn, P., Gibson, C.R. & Mader, T.H. The odyssey of the ocular and cerebrospinal fluids during a mission to Mars: the “ocular glymphatic system” under pressure. Eye (2021). https://doi.org/10.1038/s41433-021-01721-9
- ↑ Strangman GE, Zhang Q, Marshall-Goebel K, et al. Increased cerebral blood volume pulsatility during head-down tilt with elevated carbon dioxide: the SPACECOT Study. Journal of Applied Physiology (Bethesda, Md. : 1985). 2017 Jul;123(1):62-70. DOI: 10.1152/japplphysiol.00947.2016. PMID: 28360122.
- ↑ Galdamez LA, Brunstetter TJ, Lee AG, Tarver WJ. Origins of Cerebral Edema: Implications for Spaceflight-Associated Neuro-Ocular Syndrome. J Neuroophthalmol. 2020 Mar;40(1):84-91. doi: 10.1097/WNO.0000000000000852. PMID: 31633590.
- ↑ Morgan WH, Cunneen TS, Balaratnasingam C, Yu DY. Wearing swimming goggles can elevate intraocular pressure. Br J Ophthalmol. 2008 Sep;92(9):1218-21. doi: 10.1136/bjo.2007.136754. Epub 2008 Jul 11. PMID: 18621792.
- ↑ Scott JM, Tucker WJ, Martin D, et al. Association of Exercise and Swimming Goggles With Modulation of Cerebro-ocular Hemodynamics and Pressures in a Model of Spaceflight-Associated Neuro-ocular Syndrome. JAMA Ophthalmol. 2019;137(6):652-659. doi:10.1001/jamaophthalmol.2019.0459