Pilomatrixoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Pilomatrixoma (pimatricoma) is a firm subcutaneous nodule often found on the head and neck of children.
Disease Entity
A pilomatrixoma is a benign, firm subcutaneous mass found under the skin. It most commonly presents as a single lump found on the face, scalp, eyelids, eyebrows, neck, or arms, but in some instances can be multiple in nature.
Disease
The majority of cases of pilomatrixoma occur in children younger than 10, but can also present in older children and adults.
Females are two times more likely as males to have a pilomatrixoma.
Etiology
Also known as benign calcifying epithelioma of Malherbe, this is a rare benign tumor that originates from the hair root matrix. It was first described by Malherbe and Chenantais in 1880.
Risk Factors
Pilomatrixomas have been found to be familial in some cases, or seen in association with inherited genetic syndromes such as familial adenomatous polyposis (Gardner's syndrome), myotonic dystrophy, or Turner Syndrome.[1] A female preponderance has been reported.
Primary Prevention
There is no primary prevention.
Diagnosis
Diagnosis is often difficult to make clinically, and therefore can only be definitively established after histopathological examination of the lesion after biopsy or surgical removal.
History
Usually presents as a slowly enlarging mass under the skin, often less than 3cm in diameter. There is typically no associated pain, overlying skin inflammation, or change in skin color. Less commonly, the lesion may become inflamed or infected, and cause discomfort at that time.
A few case reports have described lesions that presented as bruising after trauma, with some authors suggesting this could be a more aggressive variant of the lesion. In contrast, a survey by Orlando et al, described 150 cases of pilomatrixoma at a pediatric hospital that had no preceding history of trauma or inflammation.
Physical examination
Subcutaneous nodule often less than 3cm in diameter under the skin in typical locations in the eyelids, eyebrows, scalp, labella, or neck. Other locations also seen less commonly.
Nodule is round, smooth, very firm, and freely mobile from underlying bone. The overlying skin may be thin and adherent to the anterior face of the lesion.
Nontender to palpation.
Overlying skin is usually normal without blood vessels, inflammation, or ulceration.
Some reports have described red-blue or bluish-purple discoloration of the skin to be more typical of pilomatrixoma that could differentiate it from inclusion and dermoid cysts. Inclusion cysts tend to have a diffuse yellow color due to keratin within the cyst, and are softer and more fluctuant.
The skin over infantile hemangiomas in the subcutaneous tissue will often have a bluish-purple hue which can sometimes be seen with pilomatrixomas, but an infantile hemangioma would be softer than a pilomatrixoma.
Rhabdomyosarcoma can rarely present as an eyelid mass, but typically has erythema of the skin and is an extension of deeper orbital tissue involvement.
Diagnostic procedures
Pathologic evaluation of the surgical specimen is necessary to make the definitive diagnosis, although clinical findings are usually typical for pilomatrixoma.
Laboratory test
Blood tests are not indicated. Imaging such as Xray, CT or MRI are often not performed as the clinical examination is often suggestive of the lesion prior to surgery.
Differential diagnosis
- Dermoid cyst
- Epidermoid cyst
- Inclusion cyst
- Chalazion
- Lipoma
- Fibroma
- Bone cyst
- Hematoma
- Infantile hemangioma of the soft tissues
- Cholesterol granuloma
- Malignant tumor (rhabdomyosarcoma)
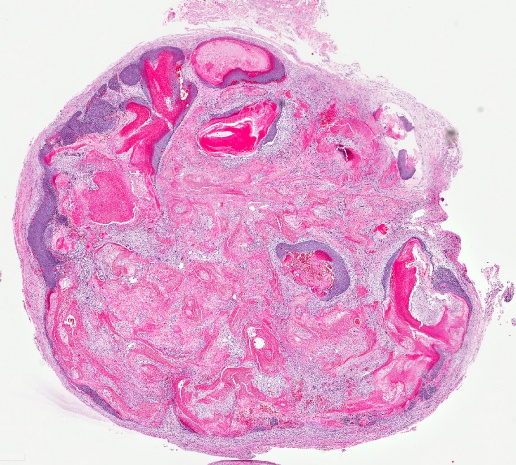
Histopathology
Histopathology demonstrates a pseudoencapsulated mass with eosinophilic acellular material with prominent ghost cells. Small foreign body giant cell granulomas and calcification can be present within the lesion. Nests of basaloid cells with little cytoplasm comprise the periphery of the lesion, and form keratinous material.
General treatment
Observation is reasonable unless the lesion enlarges and becomes symptomatic. A pilomatrixoma will not resolve spontaneously or involute; therefore, surgical excision is the treatment of choice for symptomatic or progressively enlarging lesions.
Medical therapy
No medical treatment
Surgery
Surgery is the treatment for complete removal of the lesion. This is usually curative and also allows for pathologic diagnosis of the mass.
The procedure is often performed as a day surgery, with the child going home after surgery. The lesion is removed in its entirety and sent in formalin for histopathologic evaluation.
Surgical follow up
Routine surgical postoperative care typically involves rest, cool compresses to the surgical site, and antibiotic ointment for sutures. Pain is often minimal.
Prognosis
Prognosis after surgical removal is excellent, but reports have shown a very low recurrence rate in some cases. Patients and their family should be aware that any new lesions should be evaluated appropriately. Patients with more than six lesions or with a family history of myotonic dystrophy or colon cancer should undergo additional screening.[1]
References
- Malherbe A, Chenantais J(1880) Note sur L'epitheliome calcife des glandes sebacees. Prog Med (Paris) 8:826–837.
- Moehlenbeck FW(1973) Pilomatrixoma (calcifying epithelioma). A statistical study. Arch Dermatol 108:532–534.
- Macleod AJ, Scobie WG(1991) Pilomatrixoma as a diagnostic problem: the Edinburgh experience. J Roy Coll Surg Edinb 36:261–263.
- Matthew LC, Olver JM, Cree IA. A large rapidly growing pilomatrixoma on a lower eyelid. Br J Ophthalmol 1999, 84(10):1203.
- Yoshmura Y, Obara S, Mikama T, et al.(1998) Calcifying epithelioma (pilomatrixoma) of the head and neck: an analysis of 37 cases. Br J Oral Maxillofac Surg 35:429–432.
- Orlando RG, Rogers GL, Bremer DL(1983) Pilomatixoma in a paediatric hospital. Arch Ophthalmol 101:1209–1210.
- Inglefield CJ, Muir AFK, Gray ES(1994) Aggressive pilomatrixoma in childhood. Ann Plas Surg 33:656–658.
- Rotenburg M, Laccourreye O, Cauchois R(1996) Head and neck pilomatrixoma. Am J Otolaryngol 17:133–135.
- Shields J, Shields C, Eagle R, et al.(1995) Pilomatrixoma of the eyelid. J Pediatr Ophthalmol Strabismus 32:260–261.
- Yap E, Hohberger G, Bartley G(1999) Pilomatrixoma of the eyelids and eyebrow in children and adolescents. Ophthalmic Plast Reconstr Surg 15:185–189.