Phacocele and Pseudophacocele
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
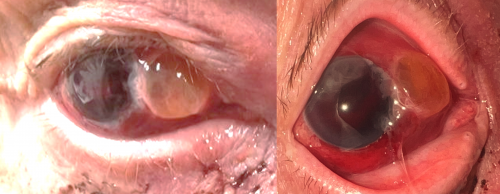
Trauma-induced dislocation of lens into the subconjunctival space.
Disease Entity
A phacocele is a rare eye condition resulting from blunt injury. It happens when the crystalline lens moves to the subconjunctival space due to a flaw in the sclera. This condition represents a small minority of all lens displacements. Both direct and indirect injuries can lead to a phacocele. When an implanted intraocular lens (IOL) is dislocated in a similar manner due to a scleral flaw, it's referred to as a pseudophacocele, which can also be a result of either direct or indirect trauma. [1]
Etiology
The force due to blunt trauma on the globe damages the zonular integrity and pushes the crystalline lens or IOL through the ruptured scleral wall into the subconjunctival space through the route of least resistance. Damage to the zonules is one of the "Seven Rings of Trauma" that can be an expected outcome of severe blunt trauma to the eye; however, a scleral defect is an crucial component in the process of allowing the lens to dislocate in the subconjuctival space.
Risk Factors
A significant risk factor is a history of scleral surgery, i.e. previous globe injury, scleral incision for cataract surgery, vitrectomy, or a trabeculectomy. Forming a conduit from the anterior chamber through the sclera to a subconjunctival space allows for high intraocular pressure in the setting of trauma to dislodge the lens into a low pressure space through the scleral channel.
Phacoceles almost exclusively happen in the adult population. It is very rare for a phacocele to occur in children due to their more elastic sclera and softer crystalline lens, although there have been cases presenting this phenomenon .
Diagnosis
History
Phacoceles and psuedophacoceles occur in the setting of blunt trauma. These patients may have had recent ophthalmic surgery and have scleral incisions that may not be completely healed.
Physical examination
Patients will have a significant decrease in visual acuity due to the dislocation and any accompanying symptoms such as hyphema, iritis, loss of iris, etc. Patients will have a visible crystalline lens or IOL in the subconjuctival space. Psuedophacocele might present as a single haptic protruding from a scleral defect as well. In the setting of a phacocele/psuedophacocele in a patient with a trabeculectomy, the lens or part of the lens. may be seen within the bleb. Slit lamp examination is sufficient for discovery of phacocele/psuedophacocele.
Management
Surgery
Surgical intervention includes exploration of the wound. Lens removal, vitrectomy, and repair of the wound should be done in all cases of traumatic phacocele or pseudophacocele. These cases should be treated as if they are open-globe injuries due to exposure of the open environment. The primary goal of phacocele/psuedophacocele repair is to extract the subluxated lens and maintaining the integrity of the globe. Infusion port placement can be used to prevent eye collapse.
Consideration of IOL implantation should be considered, but factors include risk of further inflammation, risk of infection, and accuracy of biometry measurement. Implantation of a lens at a later date is preferable. Biometry measurement may differ up to 4.0 diopters compared to a non-traumatic eye and should be considered when selecting a lens.
Other indicated steps: Abscission of prolapsed tissue, scleral fixation of newly implanted IOL (device), potential anterior segment reconstruction in the setting of severe blunt trauma.[2]
Prognosis
Patients can have full visual recovery, but is highly variable on the level of trauma and concomitant structural damage.
References
- ↑ Rajasekar, K.; Sangamithira, M.; Krishnan, Rohini; Ramakrishnan, Sivakalai; Vedalmaji, Aswathi. Traumatic phacocele – A rare case of lens dislocation. TNOA Journal of Ophthalmic Science and Research 60(2):p 195-197, Apr–Jun 2022. | DOI: 10.4103/tjosr.tjosr_13_22
- ↑ Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.

