Pediatric Vitreoretinal Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Vitreoretinal surgery in pediatric patients
Informed consent
Informed consent is a fundamental document in any surgical procedure, both in adults and children. It is required that parents or responsible caregivers of the child understand the procedures that will be performed, as well as the therapeutic implications, prognosis and possible derived complications.
Informed consent should be the first step in building a solid relationship with the patient and the parents, providing at the time an adequate surgical approach.[1]
Fundamentals in pediatric vitreoretinal surgery
Surgical anatomy
Location of entry
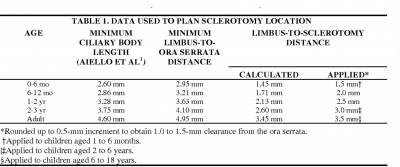
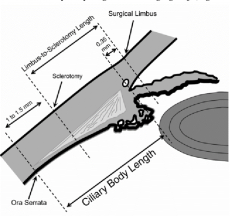
The location of the sclerotomies depends mainly on the age of the patient and the intention of a lens-sparing vitrectomy. Pars plana does not form until 6 to 9 months after delivery, and a distance of 4 mm from limbus to sclerotomies should not usually be performed before 4 years of age.[3]
When the intention is lens-sparing, a distance of 0.5 mm posterior to the limbus is required in children with retinopathy of prematurity ROP[1]
Usually 1 mm of distance from the limbus is considered for each year of the patient's life up to four years.
Transillumination of the globe wall can be used to identify the extension of the ciliary body and the entry site.
However, in not all cases, a pars plicata /pars plana approach is required. In some cases, a translimbal approach must be performd, through the root of the iri, in order to avoid entering the subretinal or suprachoroidal space. It is reserved for patients in whom a lensectomy must be performed and in whom there may be peripheral anomalies, such as anterior proliferative vitreoretinopathy PVR , stageof ROP, anteriorf ROP, traction, or persistent fetal vasculature (PFV).[1][3]Therefore, a pars plicata/pars plana approach is considered if the instruments can enter without causing iatrogenic results.
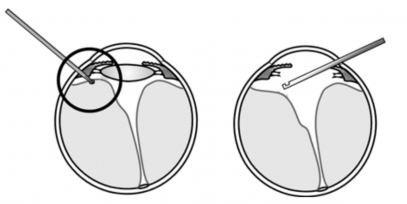
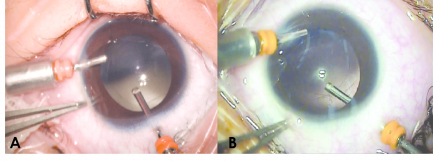
When a scleral approach is performed, it must be taken into account that children's sclera is very thin, so insertion must be perpendicular to the sclera, parallel to the visual axis.
On the contrary, an oblique insertion could cause inadvertent damage to the lens. It is recommended to suture the entry site.
Lens
Children have small axial lengths. The proportion of lens ratio compared toth eentire globe volume is higher compared to adults, being a consideration that must be taken into account in pediatric surgery. On the other hand, the pediatric response to surgical trauma is different. Children usually develop cataracts easily with the lens touch, in additio,n severe inflammatory reactions to surgery could be present.[1][7]
Vitreoretinal interface
The posterior hyaloid is firmly attached to the retinal surface in children. Furthermore, the interaction of the vitreoretinal interface is different in patients with ROP and other hereditary vitreoretinopathies. In many of these cases, vitreochisis is present, which makes its complete removal difficult.[1]
Likewise, attempting complete removal and inducing posterior vitreous detachment can lead to iatrogenic retinal tears, which are an important factor in surgical failure, especially in ROP. Complete removal of the vitreous is not recommended in patients with ROP.[7]
Surgical approaches
Vitrectomy
Surgical approaches using 2 or 3 ports have been implemented in vitreoretinal surgery. Ensuring an infusion line is essential. In many cases, the use of a 23G needle may be required. In the presence of PVR, care should be taken to segmentation of the epiretinal membranes, seeking to avoid traction. In patients with ROP, it is extremely important to avoid iatrogenic retinotomies or tears due to the high risk of failure and PVR. Likewise, the induction of posterior vitreous detachment shouldn't be a goal in pediatric vitreoretinal surgery. Rather, it seeks to release the traction of the epiretinal membranes.[1]
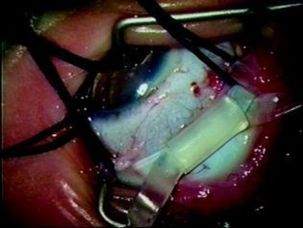
Scleral buckling
Deciding to use a scleral loop can be a bit complex, especially in young children in whom the eyeball is growing and visual development is in process. The scleral loop can be a procedure used alone or in combination with vitreoretinal surgery, especially in retinal detachment with PVR. A 2.5mm circular silicone band is commonly used.
Drainage of subretinal fluid can be ensured by transillumination to avoid access to the vortex veins. Some complications may be related to the use of a scleral buckle. These include central retinal artery occlusion, scleral growth limitation, and risk of amblyopia. In cases where eye growth occurs, division of the band is performed 3 to 6 months later.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1Hartnett ME. Pediatric retina. 3rd edition.2020
- ↑ Lemley, C.A., & H.a.n, D. (2007). An age-based method for planning sclerotomy placement during pediatric vitrectomy: a 12-year experience. Transactions of the American Ophthalmological Society, 105, 86-89; discussion 89-91.
- ↑ Jump up to: 3.0 3.1 Gan, N. Y., & Lam, W. C. (2018). Special considerations for pediatric vitreoretinal surgery. Taiwan journal of ophthalmology, 8(4), 237–242.
- ↑ Liu X, Zheng T, Zhou X, Lu Y, Zhou P, Fan F, Luo Y. Comparison between Limbal and Pars Plana Approaches Using Microincision Vitrectomy for Removal of Congenital Cataracts with Primary Intraocular Lens Implantation. J Ophthalmol. 2016;2016:8951053.
- ↑ Ranchod TM, Capone A Jr. Tips and tricks in pediatric vitreoretinal surgery. Int Ophthalmol Clin. 2011 Winter;51(1):173-83.
- ↑ Lemley, C.A., & H.a.n, D. (2007). An age-based method for planning sclerotomy placement during pediatric vitrectomy: a 12-year experience. Transactions of the American Ophthalmological Society, 105, 86-89; discussion 89-91.
- ↑ Jump up to: 7.0 7.1 Turgut B, Demir T, Çatak O. The recommendations for pediatric vitreoretinal surgery. Adv Ophthalmol Vis Syst. 2019;9(6):142‒145.
- ↑ Kychenthal B. A., Dorta S. P. (2017) Management of Stage 4 ROP. In: Kychenthal B. A., Dorta S. P. (eds) Retinopathy of Prematurity. Springer, Cham. https://doi.org/10.1007/978-3-319-52190-9_9

