Pattern Strabismus
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Pattern strabismus is defined as a difference in the magnitude of a horizontal deviation between up and downgaze. It is also known by its alternative term “alphabet patterns”. [1]
Types of Pattern Strabismus
- V pattern
- A pattern
- Y pattern
- X pattern
- Lambda pattern
Definitions
V pattern
- Definition - difference in measurement between up gaze and down gaze of at least 15 prism diopters
- Example: V pattern exotropia has a greater magnitude of deviation in up gaze than down gaze. (Figure 1)
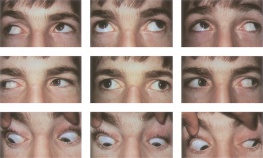 Figure 1: V-pattern exotropia.[2]
Figure 1: V-pattern exotropia.[2] - Example: V pattern esotropia has a greater magnitude of deviation in down gaze than up gaze. (Figure 2)
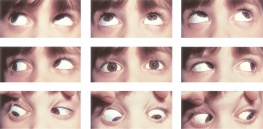 Figure 2: V-pattern esotropia. [3]
Figure 2: V-pattern esotropia. [3]
A pattern
- Definition - difference in measurement between up gaze and down gaze of at least 10 prism diopters
- Example: A pattern exotropia has a greater magnitude of deviation in down gaze than up gaze. (Figure 3)
 Figure 3: A-pattern exotropia.[4]
Figure 3: A-pattern exotropia.[4] - Example: A pattern esotropia has a greater magnitude of deviation in up gaze than down gaze.
Y pattern
- Definition - exodeviation that is greater in up gaze as compared to primary gaze and down gaze. This is thought to be due to anomalous innervation to lateral rectus muscles in up gaze
X pattern
- Definition - exodeviation that is present in primary gaze and increases in up gaze and down gaze. It occurs in long-standing exotropias due to the leash effect of tight lateral rectus muscles
Lambda pattern
- Definition - alignment is ortho in up gaze and primary gaze, with an exodeviation in downgaze
Epidemiology
- An A or V pattern is found in 15-25% of all horizontal strabismus cases. V pattern is the most common overall. [5]
Etiology
There are several conditions or etiologies associated with pattern strabismus. These include:
Oblique muscle dysfunction
- inferior oblique muscle overaction – V pattern
- superior oblique muscle overaction – A pattern
Orbital pulley system abnormalities
- simulate oblique muscle overaction – A or V pattern
- craniofacial anomalies – V pattern
Ocular torsion
- extorsion displaces the superior rectus muscle temporally and inferior rectus muscle nasally – V pattern
- intorsion displaces the superior rectus muscle nasally and inferior rectus muscle temporally – A pattern
Restricted horizontal rectus muscles
- contracture of the lateral rectus muscles in large angle exotropia – X pattern
Anomalous innervation
- occurs alone or with congenital cranial dysinnervation disorders – Y pattern
Selective innervation of superior or inferior compartments of the horizontal rectus muscles
- contributing factor to A or V pattern
Diagnosis
- The presence of a pattern strabismus is assessed by measuring alignment in approximately 25 degrees for up gaze (chin down) and 35 degrees for down gaze (chin up) from the primary gaze position. The patient should be wearing the appropriate refractive correction to minimize an accommodative component. It is important to note any compensatory head positions, such as chin up or down. For example, a chin up position may be seen with an A pattern esotropia.
Management
- If the pattern is clinically significant and/or there is an anomalous head position, strabismus surgery is recommended. Any horizontal deviation should be addressed during the procedure. [6]
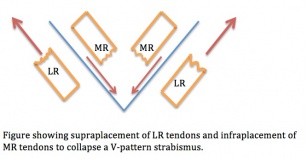
V pattern
- with overaction of the inferior obliques – weakening of the inferior obliques
- without overaction of the inferior obliques – vertical transposition of the horizontal rectus muscles
- muscles are transposed one-half to full tendon width with the medial rectus muscle moving toward the “apex” of the pattern and the lateral rectus muscle toward the open end of the pattern. A helpful mnemonic is MALE – medial rectus muscle to the apex, lateral rectus muscle to the empty space. For example, the medial rectus muscles would be moved downward in a V pattern.
- with dissociated vertical deviation – anterior transposition of the inferior oblique muscles
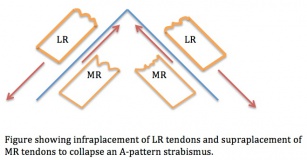
A pattern
- with overaction of the superior obliques – weakening of the superior obliques
- without overaction of the superior obliques – vertical transposition of the horizontal rectus muscles
Y pattern
- superior transposition of the lateral rectus muscles
X pattern
- recession of the lateral rectus muscles
Lambda pattern
- weakening of the superior oblique muscles
Additional Resources
Readers are referred to a brief lecture on pattern strabismus in the video below:
References
- ↑ von Noorden, Campos EC. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. Sixth edition. ST Louis: Mosby; 2002: 396-413.
- ↑ American Academy of Ophthalmology. Figure 1: V-pattern exotropia. https://www.aao.org/image/v-pattern-exotropia Accessed June 1, 2020
- ↑ American Academy of Ophthalmology. V-pattern esotropia. https://www.aao.org/image/v-pattern-esotropia Accessed June 1, 2020
- ↑ American Academy of Ophthalmology. A-pattern exotropia with overaction of the superior oblique muscles OU. https://www.aao.org/image/apattern-exotropia-with-overaction-of-superior-obl-2 Accessed June 1, 2020
- ↑ Basic Clinical Science Course. American Academy of Ophthalmology. “Pattern Strabismus.” Basic Clinical Science Course: 2020-2021,107-113 (2020).
- ↑ Basic Clinical Science Course. American Academy of Ophthalmology. “Pattern Strabismus.” Basic Clinical Science Course: 2020-2021,107-113 (2020).