Parkinson Sign
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Parkinson Sign
Disease Entity
Disease
Parkinson sign is a constellation of symptoms characterized by an isolated palsy of cranial nerve VI accompanied by an ipsilateral, post-ganglionic Horner's Syndrome. Clinical recognition of this sign is important as it offers precise localization of the lesion to the ipsilateral cavernous sinus.
Etiology
The etiology of Parkinson sign is tied to compression or inflammation of the posterior cavernous sinus. This could be secondary to a mass lesion (e.g. meningioma, schwannoma, lymphoma, metastasis), vascular pathology (e.g. internal carotid artery (ICA) dissection, ICA aneurysm, ICA thrombosis), inflammatory disorders (e.g. Tolosa-Hunt Syndrome), trauma, or giant cell arteritis.
Risk Factors
Risk factors for Parkinson sign depend on the etiology. Smoking, long-standing hypertension, a family history of cancer or vascular disease, advanced age, or a hypercoagulable state may place patients at greater risk for developing a pathologic process leading this syndrome.
Relevant Anatomy
The anatomy of the sympathetic chain, cranial nerve VI, and the cavernous sinus are crucial to understanding Parkinson sign and its value for lesion localization.
Sympathetic Chain Anatomy
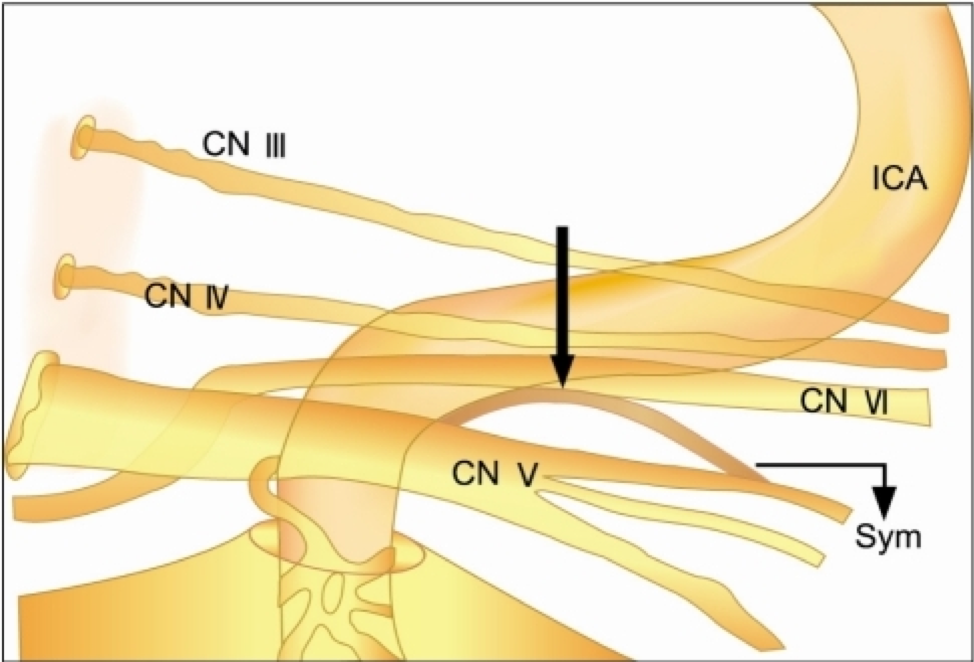
The sympathetic chain is a three-neuron pathway that originates in the hypothalamus. It descends through the brainstem until it synapses in the Ciliospinal Center of Budge in the spinal cord at the level of C8-T2. From here, the second order neuron exits the spinal column, passes over the lung apex, and ascends through the cervical chain until it synapses with the third order neuron in the superior cervical ganglion. The third order neuron travels superiorly, forming a plexus around the ICA and moving into the cavernous sinus. In the posterior cavernous sinus, the sympathetic chain leaves the ICA to briefly join CN VI before joining the ophthalmic division of CN V (V1) and exiting the cavernous sinus to run through the superior orbital fissure (Figure 1). From there, one branch follows the nasociliary nerve to become the long ciliary nerves innervating the pupillary dilator muscle. Another branch, forming the sympathetic root of the ciliary ganglion, follows the ophthalmic artery, passes through the ciliary ganglion without synapsing, forms part of the short ciliary nerves, and innervates Müeller’s muscle and the lower lid retractor. Still other fibers pass through the optic canal.
Cranial Nerve VI Anatomy
CN VI originates in the abducens nucleus in the caudal, dorsal pons just below the 4th ventricle. From the nucleus, it travels antero-superiorly before exiting the brainstem at the pontomedullary groove and entering the subarachnoid space. It then travels within Dorello’s canal to enter the dura inferior to the posterior clinoid process and subsequently enters the cavernous sinus. Here, it runs just lateral to the ICA before entering the orbit through the superior orbital fissure and innervating the lateral rectus muscle.
Figure 1: A depiction of the posterior portion of the cavernous sinus, demonstrating oculosympathetic fibers leaving the sympathetic plexus around the ICA and moving onto CN VI before exiting on the ophthalmic branch of CN V (V1). Copyright: Open-access image, unaltered from original. License: https://creativecommons.org/licenses/by-nc/3.0/ Original: https://openi.nlm.nih.gov/detailedresult.php?img=PMC3223717_kjo-25-459-g005&req=4
Pathophysiology
Parkinson sign results when both the sympathetic chain and CN VI are disrupted simultaneously. These paths intersect in the cavernous sinus, which gives this sign great localizing value.
Diagnosis
Diagnosis can be made clinically by observation of an anisocoria that is more pronounced in the dark, accompanied by ptosis and isolated abduction ophthalmoplegia ipsilateral to the smaller pupil. If the Horner's Syndrome component of the diagnosis is questionable, sympathetic denervation can be confirmed by reversal of the anisocoria upon apraclonidine administration or by failure of the miotic pupil to dilate upon cocaine administration. The Horner's Syndrome can be confirmed to be third-order by lack of dilation of the miotic pupil upon administration of hydroxyamphetamine. A third-order Horner's Syndrome with a concomitant ipsilateral abduction ophthalmoplegia confirms the presence of Parkinson Sign and localizes the lesion to the ipsilateral cavernous sinus.
Signs
Miosis (anisocoria more pronounced in the dark), partial ptosis (of upper and lower lids) ipsilateral to the miotic pupil, facial anhidrosis, and inability to abduct the affected eye
Symptoms
Patients may present with horizontal diplopia, headache, eye pain or retroorbital pressure sensation, and/or blurred or decreased vision (secondary to ptosis).
Differential Diagnosis
A lesion in the pons could also affect both the descending sympathetic chain and the abducens nerve, however, it would be extremely unlikely that it not also involve the facial nerve (since the facial nerve wraps around the abducens nucleus). Additionally, this would produce a first-order Horner's Syndrome, so a hydroxyamphetamine test would be negative, ruling out Parkinson sign.
Work-up and Management
After identification, neuroimaging should be ordered as soon as possible. This may include magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) scans of the brain to visualize the cavernous sinus, and then possible additional imaging based on the suspected etiology. Inflammatory markers like erythrocyte sedimentation rate (ESR) and C reactive protein (CRP), and complete blood count (CBC) may also be ordered to look for giant cell arteritis or hematologic malignancy. After identification of the lesion, management will depend on the etiology.
Prognosis
Prognosis depends on the etiology of the lesion.
References
1. Boisvert CJ, MD, Tran NA, Al Othman B, MD (2016). Anisocoria. American Academy of Ophthalmology, EyeWiki. Retrieved March 3, 2019, from: https://eyewiki.aao.org/Anisocoria
2. Ebner, R. N., Ayerza, D. R., & Aghetoni, F. (2014). Sixth nerve palsy + ipsilateral Horner's Syndrome = Parkinson's Syndrome. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society, 29(1), 63-6. 3. Kang, N. H., Lim, K. H., & Sung, S. H. (2011). Horner's syndrome with abducens nerve palsy. Korean journal of ophthalmology : KJO, 25(6), 459-62.
4. McDougal, D. H., & Gamlin, P. D. (2015). Autonomic control of the eye. Comprehensive Physiology, 5(1), 439-73.
5. Nguyen V, Varacallo M. Neuroanatomy, Cranial Nerve 6 (Abducens) [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430711/
6. Tsuda H, Ishikawa H, Kishiro M, et al.: Abducens nerve palsy and postganglionic Horner syndrome with or without severe headache. Intern Med 2006, 45:851–855.
7. V.Y., V., G., P., V., G., V., L., D., K., & M.K., G. (2014). Parkinson syndrome: A precise localization for abducens palsy. Journal of the Neurological Sciences.