Orbital Varices
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Orbital varices are venous malformations of the orbit caused by vascular dysgenesis [1]. They consist of a plexus of thin-walled distensible low flow vein-like vessels that are commonly intrinsic to the normal circulation [2]. They are considered to be hamartomatous.
Epidemiology
Orbital varices are a rare condition, accounting for 0-1.3% of all histopathologically proven orbital masses [3]. Orbital varices are usually diagnosed between the ages of 10-30 years. However, they can be seen in every age group, even in neonates[3]. Most cases occur unilaterally. Males and females are affected equally [4].
Classification
The Orbital Society created a classification of vascular lesions into three categories based on flow:
- No flow (type I): Lymphangiomas
- Venous flow (type II): Varices
- Arterial flow (type III): Arteriovenous malformations
Orbital varices are considered a type II vascular malformation, containing venous flow. Orbital varices can also be divided into primary and secondary types. Primary orbital varices are confined to the orbit and are not associated with an AVM. Secondary orbital varices are acquired in association with a carotid-cavernous fistula, dural arteriovenous fistula, or intracranial arteriovenous malformation [3].
Pathophysiology
The pathophysiology of this condition is not well understood. Localized weakening of the vein wall may be the inciting event, leading to stagnant blood flow in the vein. The orbital veins lack valves, and therefore pooling of blood is increased, resulting in thrombosis. The thrombosis recanalizes over time, however the resistance to blood flow results in proximal dilation of the vein, producing a varix [3]. This lesion most commonly involves the superior ophthalmic vein, but other veins of the orbit can also be affected.
Risk factors
Risk factors for primary orbital varices are not well established. Secondary orbital varices are associated with carotid-cavernous fistula, dural arteriovenous fistula, and intracranial arteriovenous malformation [3].
Diagnosis
A diagnosis of orbital varices should be explored if a patient reports intermittent proptosis that is position dependent and increased with Valsalva maneuver. Another presentation that should prompt an orbital varix workup is enophthalmos. Imaging should be obtained to assist with diagnosis, however the varices may not be seen if they are not distended, so valsalva maneuvers should be employed.
Symptoms
Most patients will experience positional proptosis with a head-down position, and intermittent proptosis that is exacerbated by coughing, straining, the Valsalva maneuver, or compression of the jugular veins. This occurs because the orbital venous system is connected to the systemic venous circulation. Some small nondistensible orbital varices will not cause positional proptosis because they have none or negligible connection to the systemic circulation [3]. Some patients may complain of intermittent diplopia. Occasionally, the varix can present acutely, with onset of painful proptosis, compressive optic neuropathy with decreased visual acuity, resulting from thrombosis or hemorrhage of the affected vein.
Physical Exam
Visual acuity, pupillary examination, extraocular movements, intraocular pressure measurement, and Hertel exophthalmometry are important parts of the initial ophthalmic examination to evaluate patients with symptoms of intermittent or acute onset proptosis.
Exam can show unilateral intermittent non-pulsatile proptosis with maneuvers that increase venous pressure, without an associated bruit [2]. Long-standing lesions can be associated with enophthalmos at rest, possibly due to atrophy of surrounding orbital fat or chronic distension[5]. Rarely, large lesions involving the superior ophthalmic vein may present as a lacrimal mass. One case study reported the finding of ipsilateral pupil enlargement during Valsalva’s maneuver in a patient with an orbital varix, that resolved as the proptosis resolved [6]. This was attributed to compression of the ciliary ganglion by the engorged varices, inhibiting tonic pupillary constriction.
A patient with a thrombosed orbital varix can have decreased visual acuity, severe pain, and increased proptosis.
Complications
Possible complications of orbital varices includes thrombosis (pain, increased proptosis, decreased vision), acute orbital hemorrhage, and decreased vision due to optic nerve compression [2]. A case of orbital hemorrhage due to ruptured varix following retrobulbar anesthesia during cataract surgery was reported in a patient with a previously unknown history of orbital varix [7]. A case series examined imaging studies of 233 patients diagnosed with orbital varices and found that 9 patients (4%) had abnormalities of the neighboring orbital walls. Four cases exhibited pitting of the adjacent orbital wall, 3 cases showed enlargement of the superior orbital fissure, and 2 cases had multiple orbital roof defects[8]. One case study reported an orbital varix associated with blepharospasm[9].
Imaging
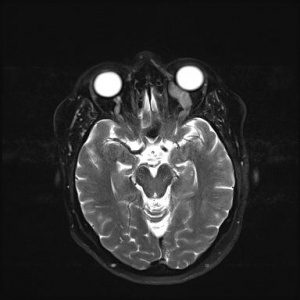
CT and MRI both demonstrate an irregular mass, usually in the posterior orbit, or a tortuous, dilated vessel that tapers toward the orbital apex and lacks internal septae [3].
In some cases, the varix is not seen on CT or MRI, but will become apparent if the patient performs a Valsalva maneuver during the scan. If there is no thrombosis or hemorrhage, the varix is hypointense on T1 and T2-weighted MRI compared to the extraocular muscles. The varix can demonstrate heterogeneous signal intensity consistent with blood in different stages of breakdown. If thrombosis is present, it appears hyperdense on pre-contrast CT. On ultrasound, varices are seen as anechoic tubes, with Color Doppler Imaging displaying increased venous flow with occasional flow reversal with Valsalva. On plain X-ray and CT, phleboliths (foci of calcification) may be seen.
Imaging can also reveal orbital expansion (more common in children), or an orbital wall defect[8]. There is a 10% rate of non-contiguous intracranial vascular malformations, therefore careful evaluation of the brain is required[3].
Histology
Histopathological studies show vascular channels lined with endothelial cells, thickened vessel walls, interstitial fibrosis, hemosiderin pigment (indicating chronic hemorrhage), infiltration of chronic inflammatory cells, and phleboliths[3].
Differential diagnosis
Differential of non-thrombosed varices includes:
- Cavernous hemangioma. The most common benign primary orbital tumor in adults. It is usually diagnosed in the third to fifth decade of life and is characterized by slowly progressive unilateral globe proptosis. Imaging will likely show a well circumscribed, homogenous mass, as opposed to typical irregular shape of an orbital varix.
- Lymphatic malformation. Previously called lymphangioma. Formed due to a disruption in the initially pluripotent rudimentary vasculature, leading to aberrant development and congenital vascular dysgenesis [1]. In the orbit, they usually become apparent in early childhood. They often contain both venous and lymphatic components, and some believe them to be a variant of orbital varices[2]. However, in studies with arteriography or venography, lymphangiomas showed no demonstrable connections to the venous system[3]. Bleeding into the lumen can occur, with formation of blood-filled ‘chocolate cysts’ which often regress with time[2]. Anterior lesions can present as multiple soft blue masses in the upper nasal quadrant, while posterior lesions can present as slowly progressive proptosis, or sudden severe painful proptosis due to spontaneous intralesional hemorrhage[2]. Some lymphatic malformations may transiently get larger with upper respiratory tract infections, likely due to a reaction of the lymphoid tissue in the lesion. MRI showing multiple grape-like cystic lesions with layering of serum and red blood cells is pathognomonic [1].
- Arteriovenous malformation. Like venous malformations, arteriovenous malformations form from vascular dysgenesis. They are composed of high-flow anastomosing veins and arteries without an intermediate capillary bed. On physical exam, dilated corkscrew episcleral vessels may be seen.
- Hemangiopericytoma. Rare, slow-growing, unilateral tumors originating from pericytes with a tendency to occur in the superior orbit. The majority occur in adulthood but they can be seen at any age[3]. Imaging will likely show a well circumscribed mass, as opposed to typical irregular shape of an orbital varix.
- Infantile hemangioma. Benign vascular tumor that usually appears during the first few months of life. They usually enlarge during the first 2 years of life and then undergo spontaneous involution by age 7. It occurs most frequently in the superior nasal quadrant in healthy children[3].
- Fast draining carotid cavernous fistula. Direct communication between the internal carotid artery and the cavernous sinus resulting in dilation of the superior ophthalmic vein. The patient typically has a history of head trauma, and findings include pulsating exophthalmos, bruit over the eye, and tortuous episcleral vessels [3].
The differential for thrombosed varices encompasses that of an orbital mass:
- Mucocele. Cystic growth involving mucoid secretions and debris that arises from the paranasal sinuses. Mucoceles from frontal or ethmoidal sinuses can present with orbital symptoms such as proptosis, ptosis, or diplopia[3].
- Idiopathic orbital inflammation (pseudotumor). The patient can present with a sudden onset of unilateral eye pain, chemosis, redness, diplopia, and proptosis[3].
- Meningioma. Slow growing, benign neoplasms arising from arachnoid cap cells in the meninges. They can present in the orbit as primary orbital meningiomas, arising from the optic nerve sheath, or as secondary orbital meningiomas, extending into the orbit from other intracranial structures[10].
- Schwannoma. Benign peripheral nerve tumor due to proliferation of Schwann cells. Generally presents in young to middle-aged adults with painless progressive proptosis and downward displacement of the globe (Schwannomas tend to arise from the supraorbital and supratrochlear nerves)[3].
- Orbital neurofibroma. Benign peripheral nerve sheath tumor derived from Schwann cells, perineural cells and fibroblasts[10].
- Lacrimal gland tumors. Can be classified into epithelial and non-epithelial, with non- epithelial being the most common. Presentation generally involves upper eyelid swelling with a mass, and later symptoms can include globe displacement, ptosis, diplopia, and limited extraocular movements[10].
- Orbital lymphoma. Malignant lymphomas and reactive lymphoid lesions can present with mild unilateral proptosis, ptosis, chemosis/edema, and limitation in extraocular movements [10].
- Orbital rhabdomyosarcoma. The most common primary malignant orbital tumor in children, arising from undifferentiated mesenchymal cells. Patients present with rapid, progressive proptosis[10].
- Metastatic tumors. The orbit lacks lymphatic channels and is therefore reached by metastatic tumors by the hematogenous route. The most common primary tumors to metastasize to the orbit from most to least likely are breast, lung, prostate, skin melanoma, and gastrointestinal tract. In children, the most common source is neuroblastoma. The metastases present with a sudden onset of proptosis with lid ecchymosis, and can be bilateral[3].
Management:
To date there has been no definite standardization of treatment for orbital varices. Small lesions do not usually require treatment. Recurrent thrombosis, severe proptosis, pain, or optic nerve compression can be indications for intervention.
Surgical Excision
Deep distensible venous malformations have been traditionally treated with surgery. Surgical excision can be challenging due to the friable nature of the lesions with a tendency to bleed, which can lead to severe hemorrhage and optic nerve compromise from vascular insufficiency[2]. Often, the varix is in a collapsed state when the patient is supine during the surgery, contributing to the difficulty in finding and dissecting the varix. Placing the patient in Trendelenburg position, jugular compression, or requesting the anesthesiologist to increase the intrathoracic pressure can help[3]. Surgical excision has been reported to be facilitated by the use of clips, endovascular embolization, and percutaneous injection of N-butyl cyanoacrylate NBCA glue[11].
Endovascular embolization
Embolization been used as an alternative to surgical excision, as well as prior to surgical excision to decrease the risk of bleeding. The first description of embolization for the treatment of an orbital varix was in 1994 by Takechi et al. using transvenous microcoil embolization with 204 platinum microcoils via Guglielmi detachable coil (GDC)[12]. Endovascular embolization of the varix can be performed via the jugular vein and cavernous sinus, or after surgical exposure of the varix. Compressive optic neuropathy and severe vision loss have been reported following endovascular coiling, due to formation of intralesional thrombosis and subsequent enlargement of the lesion[13].
Percutaneous N-butyl cyanoacrylate (NBCA) glue embolization
Percutaneous injection of NBCA glue into the varix has been used to embolize orbital varices prior to orbitotomy surgery. Percutaneously injected NBCA was found to be useful in visualizing the varix during the excision, and provided good hemostasis in a retrospective case series of 4 patients [14]. A case series reported a giant cell foreign body response to the glue cast, after glue embolization for a varix in the lower eyelid[11].
Percutaneous alcohol sclerotherapy
This technique has been shown to be effective in treating superficial facial venous malformations, however it has not been recommended for use in deep orbital varices. If alcohol leaks from the injection site, it can produce local tissue injury, therefore increasing risk of optic nerve injury (11, 15).
Carbon dioxide laser surgery
CO2 laser ablation has been used as an adjunct to surgical excision. Success has also been reported with use transcutaneously and after surgical exposure without subsequent surgical excision for both superficial and deep venous malformations[11][15].
Prognosis:
Most cases of primary orbital varices have a good prognosis. Recurrence after surgical intervention can occur, but most patients remain stable.
References
- ↑ Jump up to: 1.0 1.1 1.2 Foster, Jill A. Orbit, Eyelids, and Lacrimal System. American Academy of Ophthalmology, 2018.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Bowling, B. (2016). Kanski's clinical ophthalmology: A systematic approach. Elsevier.
- ↑ Jump up to: 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 Karcioglu, Z. A. (Ed.). (2014). Orbital tumors: diagnosis and treatment. Springer.
- ↑ Rubin, P. A., & Remulla, H. D. (1997). Orbital venous anomalies demonstrated by spiral computed tomography. Ophthalmology, 104(9), 1463-1470.
- ↑ Smoker, W. R., Gentry, L. R., Yee, N. K., Reede, D. L., & Nerad, J. A. (2008). Vascular lesions of the orbit: more than meets the eye. Radiographics, 28(1), 185-204.
- ↑ Aggarwal, E., Madge, S., Crompton, J., & Selva, D. (2009). Dynamic pupillary abnormalities associated with orbital varices. Clinical & experimental ophthalmology, 37(8), 825-826.
- ↑ Yoshimoto, M., & Matsumoto, S. (2004). Orbital varix rupture during cataract surgery. Journal of Cataract & Refractive Surgery, 30(3), 722-725.
- ↑ Jump up to: 8.0 8.1 Islam, N., Mireskandari, K., & Rose, G. E. (2004). Orbital varices and orbital wall defects. British journal of ophthalmology, 88(8), 1092-1093.
- ↑ Hmida, B., Mnari, W., Maatouk, M., Zrig, A., & Golli, M. (2019). Orbital varix: rare cause of blepharospasm. The Pan African Medical Journal, 32, 147.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 10.4 Shields, J. A., & Shields, C. L. (2008). Eyelid, conjunctival, and orbital tumors: An atlas and textbook. Lippincott Williams & Wilkins.
- ↑ Jump up to: 11.0 11.1 11.2 Lacey, B., Rootman, J., & Marotta, T. R. (1999). Distensible venous malformations of the orbit: clinical and hemodynamic features and a new technique of management. Ophthalmology, 106(6), 1197-1209.
- ↑ Takechi, A., Uozumi, T., Kiya, K., Yano, T., Sumida, M., Yoshikawa, S., & Pant, B. (1994). Embolisation of orbital varix. Neuroradiology, 36(6), 487-48
- ↑ Hwang, C. S., Lee, S., & Yen, M. T. (2012). Optic neuropathy following endovascular coiling of an orbital varix. Orbit, 31(6), 418-419.
- ↑ Couch, S. M., Garrity, J. A., Cameron, J. D., & Cloft, H. J. (2009). Embolization of orbital varices with N-butyl cyanoacrylate as an aid in surgical excision: results of 4 cases with histopathologic examination. American journal of ophthalmology, 148(4), 614-618.
- ↑ Arat, Y. O., Mawad, M. E., & Boniuk, M. (2004). Orbital venous malformations: current multidisciplinary treatment approach. Archives of Ophthalmology, 122(8), 1151-1158.
- Dutton, JJ. Radiology of the Orbit and Visual Pathways. 2010. Elsevier, Inc. Ch 6:121-385.