Orbital Applications of Microautologous Fat Transplantation
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Original Contributors: Stephanie Trejo Corona, Srijith Kambala, Carla Dias, Jay Jaber, Michael T. Yen, MD
Surgical Therapy
Background
Microautologous fat transplantation (MAFT) is a minimally invasive surgical technique that restores facial and periorbital volume lost in the natural aging process by harvesting and reinjecting fat into targeted areas. Autologous fat transfer was first reported in 1893, in which German surgeon Neuber transplanted adipose tissue from the arm to the orbit.1 Common reasons patients may seek oculoplastic management with MAFT include sunken upper eyelids,2–4 tear trough deformities, protruding orbital fat, and lower eyelid dermatochalasis.5 Achieving a more youthful appearance by restoring the periorbital areas is usually obtained via transcutaneous lower blepharoplasty6 or synthetic fillers.7 Areas typically treated with dermal fillers, such as the periocular area, forehead, brow, cheeks, midface, nasolabial folds, lips, temples, jawline, submental crease, and chin can also be treated with fat grafting.7 MAFT is advantageous as it blends the tear trough (nasojugal groove) and lid-cheek junction (palpebromalar groove) via a more refined and targeted approach that minimizes complications.6 While often used in isolation, MAFT can be combined with other procedures such as blepharoplasties.8 Overall, MAFT is predominantly employed in elective cosmetic procedures but may also be used as therapy for congenital or acquired defects or reconstructive procedures.
Anatomy
With age, a redistribution of body fat occurs, leading to a relative decrease in peripheral subcutaneous fat and an increase in visceral fat. This is a process that involves multiple mechanisms, including age-related insulin resistance, decreased gonadal hormones, and a decrease in adipogenesis.9,10 In the orbit, this redistribution manifests as a reduction of periorbital fat and volume. This reduction of fat alongside an age-related decline in collagen and elastin production in the skin of the orbit can cause eyelid wrinkles, tear trough deformities, and other cosmetic concerns.
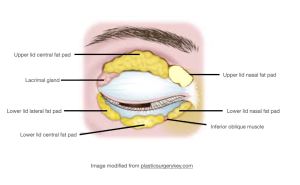
The subcutaneous fat in the orbit is organized into five compartments, two in the upper eyelid orbital fat, and three in the lower eyelid orbital fat.11 The upper eyelid fat compartments are the nasal (medial) fat pad and the central (preaponeurotic) fat pad. The superior fat pads are bordered by the orbicularis retaining ligament as it courses around the superior orbit. The lower lid central and nasal fat pads are also bordered by the orbicularis retaining ligament and the malar septum. The lower lid lateral fat pad has a superior border of the inferior temporal septum, and the inferior border is the superior cheek septum.12
In many older individuals, especially those with previous blepharoplasty, the superior sulcus in the upper eyelid becomes pronounced. This conspicuous superior sulcus along with multiple eyelid folds from thinning skin and preaponeurotic fat atrophy also results in a hollow and sunken-in appearance of the globe. MAFT addresses these contour deformities through fat transplantation from donor sites with abundant and accessible adipose tissue including the abdomen, thighs, and flank.13 These transplanted adipocytes integrate into the recipient site over a few weeks through rapid angiogenesis and revascularization before remodeling with improved collagen production.

Patient Selection
Many patients seek periorbital rejuvenation for sunken upper eyelids,2–4 tear trough deformities, protruding orbital fat, lower eyelid dermatochalasis5 and less commonly for congenital or acquired defects. Primary reconstructive surgery may also be indicated in patients with thyroid-associated orbitopathy and anophthalmic sockets.5 The ages of patients undergoing MAFT can range from 19 to 80 years,5 with studies showing the average age being around 353,4,14 to 50 years.3,6,15 Previous studies report a low male to female ratio, indicating the patient population is dominated mainly by females.5
Indications
Aesthetics
The application of MAFT in restoring volume to the tear trough and lower lids has given it particular importance in aesthetics.5 The procedure offers a range of rejuvenating properties including volume enhancement, improved skin trophicity, and wrinkle minimization.16 Patients commonly seek to alter sunken upper eyelids with multiple folds17 or age-related changes in the periocular region.18 MAFT can be used alone or combined with other techniques to achieve these goals. Optimizing symmetry and fullness can have a notable impact on patient outcomes.
Congenital or Acquired Facial Defects
While MAFT is predominantly employed in elective cosmetic procedures, it can be utilized as a primary or adjunct therapy in acquired and congenital deformities.4,13 MAFT can target a variety of defects as seen in HIV-lipodystrophy, tear trough deformities, and other conditions that affect the periorbital area, with low risk and discomfort for patients.4,21,22 In severe deformities seen in conditions like Parry-Romberg or Treacher Collins syndrome, MAFT is utilized for residual soft tissue deficits after the necessary surgical correction.19
Reconstruction
MAFT provides a minimally invasive approach for augmenting soft tissue volume in surgical treatments.19 Beyond providing volume, fat grafting can promote repair in the tissue in which it is placed.23 While a surgeon might opt for a technique like dermis-fat grafting in more significant reconstructive procedures,24 MAFT has high utility in correcting more subtle deficits, such as thyroid-associated orbitopathy5 or changes in contour from radiotherapy.19
Table 1. Indications for Microautologous Fat Transplantation | |
| Indication | Example Conditions |
| Aesthetics | ● Dermatochalasis
● Facial rejuvenation ● Periorbital hollowing ● Periorbital hyperpigmentation ● Senile sunken eye syndrome ● Sunken upper eyelids ● Tear trough deformity |
| Congenital or Acquired Facial Defects | ● Enophthalmos
● Fat atrophy (e.g. radiotherapy-induced, long-term steroid use) ● Goldehar syndrome ● HIV-lipodystrophy ● Palsy-related asymmetries ● Parry-Romberg Syndrome ● Treacher Collins syndrome |
| Reconstruction | ● Burn or trauma contour deformities
● Local scleroderma ● Post-surgical volume loss (e.g. blepharoplasty) ● Post-traumatic volume loss ● Quiescent thyroid-associated orbitopathy |
Contraindications
Immune System Instability
Although MAFT can be used to treat a variety of disease-induced orbital deformities, it can be unsafe to perform in patients with systemic or site-specific instability. Active infection, organ failure, lipid metabolism disorder, ongoing highly active antiretroviral therapy (HAART), unstable thyroid eye disease, and other chronic disease states like diabetes are common conditions that could affect graft success.22
Bleeding or Clotting Risk
Potential complications of MAFT include vascular occlusion and prolonged bruising.25 This procedure might be contraindicated in certain patients with a higher clotting risk, such as those with a history of DVT or pulmonary embolism,22 or patients at high risk of bleeding, such as those on anticoagulation therapy or a bleeding disorder.25
Orbital Damage
While MAFT can be used in treating mild to moderate deficits, extensive scarring can affect the survival or contour of the fat graft.25 Hypovascular graft sites with extensive scarring or fibrosis may not sufficiently provide nutrients to prevent fat necrosis and resorption.26,27 Contour irregularity from necrosis is also possible in donor sites with prior surgery.25
Inadequate Fat Reserves
MAFT donor sites are predominantly chosen based on fat reserve.28 In very thin patients, favorable donor sites might not provide a sufficient source for harvesting without risking iatrogenic lipoplasty deformity.22
Surgical Technique
Procedures and Surgical Treatment
Photographs of the patient’s face should be obtained at a pre-procedure evaluation and consultation with a physician. The patient’s face is marked while sitting, with careful evaluation of volume asymmetries while referencing the pre-procedure photographs as needed, and the insertion site of the cannula for the MAFT is marked.6 Swiss surgeon Dr. Trepsat8 marks a line in the upper eyelid crease, 1.5 cm above the eyebrow, the transition zone to the malar fat pad in the lower eyelid region, and a line from the tarsus to the lateral canthus. Patients can be placed under general anesthesia or local anesthesia with sedation. If MAFT is to be done in conjunction with blepharoplasty, the blepharoplasty is performed 5-15 minutes after anesthesia to the patient site before MAFT.6

Fat Harvesting
To perform MAFT, fat tissue must be harvested from a donor site, and the site may consist of resected orbital fat pads,29 fat from the abdomen, thigh,6 inner knee, or the flanks.15 Once the donor site is chosen, the site is preinfiltrated with a tumescent solution (500 mL normal saline, 25 mL of 1 to 2% lidocaine, and 0.5 ml epinephrine (1:100,000)) in a 1:1 ratio to the amount of fat that will be harvested. The site is appropriately anesthetized with lidocaine or bupivicaine.4,6 After 15 minutes, an incision is made, and the donor fat is harvested using a blunt tip cannula using a back-and-forth movement.4 It is recommended to harvest more fat than what is intended to be grafted since after centrifugation, approximately half of the harvest is usable.8
Fat Processing
Purification of donor fat is necessary since the solution contains oil, blood, and dead adipocytes. The fat is purified using standard centrifugation according to the internationally accepted Coleman’s technique,30 although other methods have been described in the literature such as the sieve method and multiple-layer gauze filtration.4 Coleman’s technique outlines centrifugation of 3000 rpm (1200 x g) for 3 minutes.4,30 After centrifugation, three layers will appear and consist of oil at the top, graftable fat in the middle, and water, blood, and tumescent solution at the bottom. The top layer of oil can be removed with gauze and the bottom layer can be removed by draining the syringe. Some studies have made modifications to the standardized Coleman technique; for example, in one study 70% fat was diluted with saline and infranatant fluid in order to better match the periocular texture.15
Fat Transfer
The purified fat is then transferred to a 1 mL syringe, and the fat is loaded into a quantified dosing injector called the MAFT-GUN (Dermato Plastica Beauty Co., Ltd., Kaohsiung, Taiwan). The injector is adjusted to the desired volume of fat for injection by rotating the dial on the MAFT-GUN. Each aliquot corresponds to a specific volume, usually 1/240 mL (0.0042 mL).6 The minimization of the injection volume is essential to improve graft survival rate since it decreases the severity of central necrosis of the fat droplet.31 The recipient area is infiltrated with a tumescent solution and anesthetized. An incision is made at the insertion site, the injector is inserted into the incision hole, and the fat is transplanted to the desired areas in multiple passes while withdrawing the MAFT-GUN. The fat is deposited into different tissue planes for a better aesthetic outcome. Some techniques involve tunnelization prior to fat injection, in which the surgeon will insert an empty cannula into the recipient site to create a network of crisscrossing tunnels in the vertical and horizontal planes to facilitate fat distribution.15
For upper eyelids, the fat is transplanted into deep, middle, and superficial layers. In the setting of correction of sunken upper eyelids, the fat is transplanted above the inferior orbital rim, the suborbicularis oculi muscle, and the supraorbicularis oculi muscle just beneath the dermis of the eyelid.4 Similarly, in the setting of correction of sunken upper eyelids with the goal of neoformation of a double eyelid crease, the fat is transplanted above the superior orbital rim, the periorbicularis oculi muscle (inframuscle or supramuscle), and the supraorbicularis oculi muscle just beneath the dermis of the eyelid.14 For lower eyelids, MAFT is done following a transcutaneous lower eyelid blepharoplasty and the fat is transplanted into either two (deep and superficial)29 or three (deep, middle, superficial)6 layers to the tear trough and lid-cheek junction.29 If injected into three layers, the fat is transplanted above the periosteum, between the periosteum and orbicularis oculi muscle, and between the dermis and orbicularis oculi muscle.29
Outcomes
In total, MAFT can take an average of 24.5 minutes to complete depending on the extent of the procedure.14 When paired with transcutaneous lower blepharoplasty, it can take an average of 61 minutes to complete.6 After the procedure, patients receive oral antibiotics and nonsteroidal anti-inflammatory drugs for three to four days. Application of an ice pack for 30 minutes may not be recommended to avoid placing undue pressure.6,15 To relieve swelling, a gentle lymphatic drain massage can be recommended 7 days after the surgery.6
Overall satisfaction with the efficacy of MAFT is high. In a meta-analysis of satisfaction rates, the cosmetic operation satisfaction rate was 91.6% (95% CI, 86.9%–94.8%), while the rate with reconstructive surgeries was 81.9% (95% CI, 73.3%–88.2%).5 Studies have reported varying degrees of volume maintenance after surgery. Another study reported 60 (75.9%) patients photographed maintained orbital volume while 12 patients (15.2%) had some degree of volume depletion between 6 and 12 months.15 Moreover, one study found that 32% of the injected volume was maintained at 16 months based on 3D imaging measurements.32 Given the variability of follow up and fat assessment retention rate, more objective tools to assess fat retention are needed.5 Patients can also request a touch-up after the procedure; one study reported 4.4% patients (9/205) requested a secondary touch-up.6
In terms of patient characteristics affecting surgical outcomes, one study focused on sunken upper eyelids with multiple folds in an Asian population observed that patients in their 20s to early 40s without preseptal or pretarsal fat pads or dermatochalasis had superior results.14. Regarding the technique of the surgeon, when MAFT is performed well, dermal thickness and collagen formation increase, further improving outcomes with regards to fine wrinkles, dark circles, and skin texture when paired with transcutaneous lower blepharoplasty.6 Moreover, a retrospective study of thirty-six patients showed that those undergoing lower eyelid blepharoplasty had better cosmetic improvement with MAFT than without, measured by statistically significant improvements in the global aesthetic improvement scale and the Wrinkle Severity Rating Scale.29
Complications
Microautologous fat grafting is generally a well-tolerated procedure with minor complications. Multiple factors inherent to MAFT help prevent severe complications, including delivery of minimal per-parcel volumes of fat, utilization of autologous cells, and minimal inflammation as compared to large-volume grafting. The most common complications include edema, chemosis, contour irregularity, and volume excess.
Reported complications include the following25:
- Minor
- Edema, ecchymosis
- Volume excess
- Undercorrection
- Fat resorption
- Oil cysts
- Fat necrosis
- Granuloma
- Infection
- Significant (resulting from intravascular injection and subsequent fat embolism)
- Stroke
- Ischemic optic neuropathy or retinal vein occlusion
- Tissue necrosis
A systematic review and meta-analysis of 4046 autologous fat grafting cases revealed a satisfaction rate of 90.9%, with an overall complication rate of 7.9%.5 A subgroup analysis revealed lower complication rates at 5.1% among specially processed fat grafts, including MAFT.5
References
1. Mazzola RF, Mazzola IC. The Fascinating History of Fat Grafting. J Craniofac Surg. 2013;24(4):1069. doi:10.1097/SCS.0b013e318292c447
2. Ramil ME. Fat Grafting in Hollow Upper Eyelids and Volumetric Upper Blepharoplasty. Plast Reconstr Surg. 2017;140(5):889. doi:10.1097/PRS.0000000000003758
3. Lee W, Kwon SB, Oh SK, Yang EJ. Correction of sunken upper eyelid with orbital fat transposition flap and dermofat graft. J Plast Reconstr Aesthet Surg. 2017;70(12):1768-1775. doi:10.1016/j.bjps.2017.05.003
4. Lin TM, Lin TY, Chou CK, Lai CS, Lin SD. Application of microautologous fat transplantation in the correction of sunken upper eyelid. Plast Reconstr Surg Glob Open. 2014;2(11):e259. doi:10.1097/GOX.0000000000000141
5. Yang F, Ji Z, Peng L, et al. Efficacy, safety and complications of autologous fat grafting to the eyelids and periorbital area: A systematic review and meta-analysis. PloS One. 2021;16(4):e0248505. doi:10.1371/journal.pone.0248505
6. Huang SH, Lin YN, Lee SS, et al. Three Simple Steps for Refining Transcutaneous Lower Blepharoplasty for Aging Eyelids: The Indispensability of Micro-Autologous Fat Transplantation. Aesthet Surg J. 2019;39(11):1163-1177. doi:10.1093/asj/sjz005
7. Moak TN, Ebersole TG, Tandon D, Tenenbaum M. Assessing Clinical Outcomes in Autologous Fat Grafting: A Current Literature Review. Aesthet Surg J. 2021;41(Supplement_1):S50-S60. doi:10.1093/asj/sjab148
8. Trepsat F. Periorbital Rejuvenation Combining Fat Grafting and Blepharoplasties. Aesthetic Plast Surg. 2003;27(4):243-253. doi:10.1007/s00266-003-2126-y
9. Hunter GR, Gower BA, Kane BL. Age Related Shift in Visceral Fat. Int J Body Compos Res. 2010;8(3):103-108.
10. Caso G, Mcnurlan MA, Mileva I, Zemlyak A, Mynarcik DC, Gelato MC. Peripheral Fat Loss and Decline in Adipogenesis in Older Humans. Metabolism. 2012;62(3):337. doi:10.1016/j.metabol.2012.08.007
11. Silkiss R, Prakalapakorn SG, Yen MT, Jedrzynski N. Orbital Adipose Tissue. Accessed October 11, 2024. https://eyewiki.org/Orbital_Adipose_Tissue
12. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219-2227. doi:10.1097/01.prs.0000265403.66886.54
13. Kao WP, Lin YN, Lin TY, et al. Microautologous Fat Transplantation for Primary Augmentation Rhinoplasty: Long-Term Monitoring of 198 Asian Patients. Aesthet Surg J. 2016;36(6):648-656. doi:10.1093/asj/sjv253
14. Lin TM, Lin TY, Huang YH, et al. Fat Grafting for Recontouring Sunken Upper Eyelids With Multiple Folds in Asians—Novel Mechanism for Neoformation of Double Eyelid Crease. Ann Plast Surg. 2016;76(4):371. doi:10.1097/SAP.0000000000000668
15. Pelle-Ceravolo M, Angelini M. Properly Diluted Fat (PDF): An Easy and Safe Approach to Periocular Fat Grafting. Aesthet Surg J. 2020;40(1):19-33. doi:10.1093/asj/sjz039
16. Groen JW, Krastev TK, Hommes J, Wilschut JA, Ritt MJPF, Hulst RRJW van der. Autologous Fat Transfer for Facial Rejuvenation: A Systematic Review on Technique, Efficacy, and Satisfaction. Plast Reconstr Surg Glob Open. 2017;5(12):e1606. doi:10.1097/GOX.0000000000001606
17. Lin TM, Lin TY, Chou CK, Lai CS, Lin SD. Application of Microautologous Fat Transplantation in the Correction of Sunken Upper Eyelid. Plast Reconstr Surg Glob Open. 2014;2(11):e259. doi:10.1097/GOX.0000000000000141
18. Tonnard PL, Verpaele AM, Zeltzer AA. Augmentation Blepharoplasty: A Review of 500 Consecutive Patients. Aesthet Surg J. 2013;33(3):341-352. doi:10.1177/1090820X13478966
19. Krastev TK, Beugels J, Hommes J, Piatkowski A, Mathijssen I, Hulst R van der. Efficacy and Safety of Autologous Fat Transfer in Facial Reconstructive Surgery: A Systematic Review and Meta-analysis. JAMA Facial Plast Surg. 2018;20(5):351. doi:10.1001/jamafacial.2018.0102
20. Huang SH, Lin YN, Lee SS, et al. Three Simple Steps for Refining Transcutaneous Lower Blepharoplasty for Aging Eyelids: The Indispensability of Micro-Autologous Fat Transplantation. Aesthet Surg J. 2019;39(11):1163-1177. doi:10.1093/asj/sjz005
21. Simonacci F, Bertozzi N, Grieco MP, Grignaffini E, Raposio E. Procedure, applications, and outcomes of autologous fat grafting. Ann Med Surg. 2017;20:49. doi:10.1016/j.amsu.2017.06.059
22. Donofrio LM. Techniques in Facial Fat Grafting. Aesthet Surg J. 2008;28(6):681-687. doi:10.1016/j.asj.2008.09.003
23. Coleman SR, Katzel EB. Fat Grafting for Facial Filling and Regeneration. Clin Plast Surg. 2015;42(3):289-300, vii. doi:10.1016/j.cps.2015.04.001
24. Alkhairy S, Baig MM, Pasha UA. Unilateral Anophthalmic Socket Reconstruction With Dermis Fat Graft. Cureus. 2021;13(10):e18834. doi:10.7759/cureus.18834
25. Brown K, McCoskey M, Nakra T. Complications of facial autologous fat grafting. Plast Aesthetic Res. 2024;11(0):N/A-N/A. doi:10.20517/2347-9264.2023.94
26. Shih L, Davis MJ, Winocour SJ. The Science of Fat Grafting. Semin Plast Surg. 2020;34(1):5. doi:10.1055/s-0039-3402073
27. Bassetto F, Scarpa C, Vindigni V. Invasive Techniques in Scar Management: Fat Injections. In: Téot L, Mustoe TA, Middelkoop E, Gauglitz GG, eds. Textbook on Scar Management: State of the Art Management and Emerging Technologies. Springer; 2020. Accessed November 16, 2024. http://www.ncbi.nlm.nih.gov/books/NBK586117/
28. Vizcay M, Saha S, Mohammad A, et al. Current Fat Grafting Practices and Preferences: A Survey from Members of ISPRES. Plast Reconstr Surg Glob Open. 2023;11(3):e4849. doi:10.1097/GOX.0000000000004849
29. Cheng CY, Lin TM, Chang SL, Hu S, Huang YL. Transcutaneous lower eyelid blepharoplasty with micro-autologous fat transplantation harvested from orbital fat pads for lower eyelid aging treatment. J Plast Reconstr Aesthetic Surg JPRAS. 2024;93:111-113. doi:10.1016/j.bjps.2024.04.050
30. Coleman SR. The technique of periorbital lipoinfiltration. Oper Tech Plast Reconstr Surg. 1994;1(3):120-126. doi:10.1016/S1071-0949(10)80002-2
31. Carpaneda CA, Ribeiro MT. Study of the histologic alterations and viability of the adipose graft in humans. Aesthetic Plast Surg. 1993;17(1):43-47. doi:10.1007/BF00455048
32. Meier JD, Glasgold RA, Glasgold MJ. Autologous fat grafting: long-term evidence of its efficacy in midfacial rejuvenation. Arch Facial Plast Surg. 2009;11(1):24-28. doi:10.1001/archfacial.2008.518

