Optociliary Shunt Vessels
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Overview
Optociliary shunt vessels, also known as retinochoroidal shunt vessels of the optic disc or retinochoroidal venous collaterals, are collateral vessels on the optic nerve that connect the choroidal and retinal circulations. They are associated with multiple conditions including central retinal vein occlusion, optic nerve sheath meningioma, chronic glaucoma and chronic papilledema[1]and are a nonspecific sign of chronic retinal venous congestion.
Pathophysiology
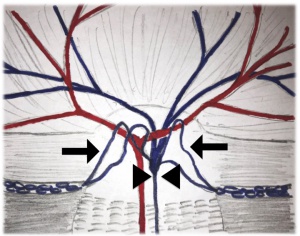
In healthy patients, retinal blood leaves the eye via the central retinal vein, which runs down the center of the optic nerve and finally drains into the superior ophthalmic vein. Optociliary shunt vessels represent collateral venous pathways draining blood from the retinal venous circulation to the peripapillary choroidal veins in the pre-laminar region of the optic nerve[2]. They result from the gradual dilatation and enlargement of pre-existing anastomotic capillary channels, as a compensatory response to the elevated pressure of central retinal venous circulation occurring in multiple conditions (Fig. 1). Studies with Indocyanine Green Angiography (ICG) demonstrated that these dilated vessels allow the retinal venous blood to bypass the obstructed central retinal vein and exit the orbit via the choroidal circulation, vortex veins and ophthalmic veins[3][4][5]. Regression of these shunt vessels have been noted following optic nerve sheath fenestration. [6]
Etiology
Optociliary shunt vessels can be classified as congenital or acquired. Congenital cases are rare. They represent a vascular malformation that connects the retinal and choroidal venous circulations[2].
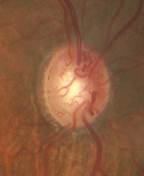
Acquired optociliary shunt vessels usually occur in association with ophthalmic conditions that produce impaired retinal venous outflow[2][7][8] (Table 1). Authors suggest the dilation of retinochoroidal vessels become evident after obstruction of central retinal vein outflow and produces significant impairments in the peripapillary microvascular network.[9] The number of collaterals may be associated with the degree of retinal ischemia.[10] They are seen most commonly with central retinal vein occlusions (CRVO) (Fig. 2). Other frequent causes include optic nerve sheath meningioma (forming a triad of symptoms along with optic atrophy and painless visual loss)[4], and chronic glaucoma[7][11]. Regarding glaucoma patients, some authors postulate that these vessels arise following a nonischemic CRVO that may not have been diagnosed clinically due to preserved central acuity where the patient did not seek medical assistance[12]. Others attribute their pathogenesis to the increased intraocular pressure and glaucomatous enlargement of the optic cup leading to retinal vein distortion[2]. Optociliary shunt vessels are also reported to occur in several other conditions such as optic nerve gliomas, drusen of the optic disc, idiopathic intracranial hypertension and also in cases of chronic papilledema or post-papilledema optic atrophy due to various causes[11][8][13]. Isolated cases have been reported in association with diabetes mellitus, presumably due to venous insufficiency secondary to the process of diabetic microangiopathy and venous stasis[2].
| Table 1- Acquired causes of optociliary shunt vessels |
|---|
| Common |
|
| Less common |
|
Diagnosis
Optociliary shunt vessels are diagnosed on ophthalmic fundus exam, appearing as tortuous vascular loops that start and end on the disc (Fig. 3). Flow within these shunts can be documented in indocyanine green angiograms[1], during the venous phase of fluorescein angiography, or with optical coherence tomography angiography[7][8]. They must be differentiated from neovascularization of the disc because neovascularization requires prompt treatment with laser photocoagulation or anti-VEGF intravitreal injections, while shunt vessels do not and can protect against retinal ischemia[8]. Optociliary shunt vessels are generally loopy and thick in appearance and do not cause leakage on fluorescein angiography[2][14][15].
The clinical approach must include a complete ophthalmic history particularly regarding prior CRVO, since it the most common association. Fundus examination may reveal some obvious etiologies, such as signs of CRVO, optic disc drusen, or a cupped optic nerve suggestive of glaucoma. Otherwise, ophthalmologists must search for causes of chronic compression of the optic nerve, such as optic nerve sheath meningioma or conditions coursing with intracranial hypertension. In cases of papilledema, optociliary vessels may help discern the chronicity of the condition because they emerge only in the setting of chronic papilledema.
Management
Work-up and treatment are directed towards the underlying etiology. Optociliary shunt vessels classically do not disappear. However, various case reports have demonstrated shunt vessels to decrease in caliber or even completely involute after treatments that improve blood flow through the central retinal vein. Another possibility is that the development of optic atrophy results in a thinner nerve with less obstruction, allowing decrease in the central retinal vein pressure and lessening the driving force for blood flow through the optociliary collateral vessels[16]. The regression of optociliary shunt vessels has been documented in cases of pseudotumor cerebri successfully treated with optic nerve sheath fenestration[13][17]. In cases of optic nerve sheath meningiomas, the involution of these vessels has been documented to occur either spontaneously, following surgical removal of the meningioma, or following radiation therapy[18]. Complete regression of the vessels after radiation treatment can be immediate[5] or take years to ensue[18].
The prognostic value of retinochoroidal collateral vessels is an ongoing controversy. Certain proponents postulate that collateral vessels can result in better visual outcomes as they provide an alternate source for drainage and reduce ischemic areas.[10][19][20] Collateral vessels have also been associated with reduced rates of macular edema.[19][21] However, certain studies have shown no difference in visual acuity outcomes between patients with and without shunt vessels.[14][21]
References
- ↑ 1.0 1.1 Fraser CL, Ridha MA, Biousse V, Newman NJ. Vitreous hemorrhage secondary to optociliary shunt vessels from papilledema. J Neuroophthalmol. Dec 2012;32(4):332-4. doi:10.1097/WNO.0b013e31825ba161
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Lee JJ, Yap EY. Optociliary shunt vessels in diabetes mellitus. Singapore Med J. Apr 2004;45(4):166-9.
- ↑ Takahashi K, Muraoka K, Kishi S, Shimizu K. Formation of retinochoroidal collaterals in central retinal vein occlusion. Am J Ophthalmol. Jul 1998;126(1):91-9. doi:10.1016/s0002-9394(98)00069-5.
- ↑ 4.0 4.1 Muci-Mendoza R, Arevalo JF, Ramella M, et al. Optociliary veins in optic nerve sheath meningioma. Indocyanine green videoangiography findings. Ophthalmology. Feb 1999;106(2):311-8. doi:10.1016/s0161-6420(99)90055-6.
- ↑ 5.0 5.1 de Alba Campomanes AG, Larson DA, Horton JC. Immediate shrinkage of optociliary shunt vessels after fractionated external beam radiation for meningioma of the optic nerve sheath. AJNR Am J Neuroradiol. Aug 2008;29(7):1360-2. doi:10.3174/ajnr.A1063.
- ↑ Abbasian J, Lee AG, Longmuir R, Rouleau J. Rapid regression of retinochoroidal venous collaterals following optic nerve sheath fenestration in idiopathic intracranial hypertension. Semin Ophthalmol. 2007 Jan-Mar;22(1):35-7.
- ↑ 7.0 7.1 7.2 Interlandi E, Pellegrini F, Papayannis A, et al. Optical Coherence Tomography Angiography Findings in Optic Nerve Sheath Meningioma. Case Rep Ophthalmol. 2020;11(2):364-369. Published 2020 Jul 14. doi:10.1159/000508411
- ↑ 8.0 8.1 8.2 8.3 Singh A, Agarwal A, Mahajan S, Karkhur S, Singh R, Bansal R, Dogra MR, Gupta V. Morphological differences between optic disc collaterals and neovascularization on optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol. 2017 Apr;255(4):753-759. doi: 10.1007/s00417-016-3565-x. Epub 2016 Dec 9. PMID: 27942950.
- ↑ Cennamo, G., Montorio, D., Solari, D., D’Andrea, L., Morra, V. B., & Tranfa, F. (2019). Optical coherence tomography angiography in optic nerve sheath meningioma. Interdisciplinary Neurosurgery, 17, 131–132. https://doi.org/10.1016/j.inat.2019.04.017
- ↑ 10.0 10.1 Lee HE, Wang Y, Fayed AE, Fawzi AA. Exploring the relationship between collaterals and vessel density in retinal vein occlusions using optical coherence tomography angiography. PLoS One. 2019 Jul 24;14(7):e0215790. doi: 10.1371/journal.pone.0215790. PMID: 31339897; PMCID: PMC6655539.
- ↑ 11.0 11.1 Thapa, B., Singh, S., Basnet, R., & Piya, S. (2019). Optociliary Shunt Vessel: An Ancillary Ophthalmic Sign Harbingering Optic Nerve Sheath Meningioma. Nepal Journal of Neuroscience, 16(3), 62-64. https://doi.org/10.3126/njn.v16i3.27361
- ↑ Konstas AGP, Holló, G.,Ritch, R. The Glaucoma book: a practical, evidence based approach to patient care. vol 6. 2010.
- ↑ 13.0 13.1 Perlmutter JC, Klingele TG, Hart WM, Jr., Burde RM. Disappearing opticociliary shunt vessels and pseudotumor cerebri. Am J Ophthalmol. May 1980;89(5):703-7. doi:10.1016/0002-9394(80)90291-3.
- ↑ 14.0 14.1 Weinberg DV, Wahle AE, Ip MS, et al. Score Study Report 12: Development of venous collaterals in the Score Study. Retina. 2013;33(2):287-295. doi:10.1097/IAE.0b013e318263d106
- ↑ Ataş F, Saatci AO. Optociliary Shunt Vessels or Neovascularisation of the Optic Disc: Fluorescein Angiography Versus Optical Coherence Tomography Angiography. Neuroophthalmology. 2022 Mar 2;46(5):339-342.
- ↑ Ruth A, Newman NJ. Images in clinical medicine. Regression of optociliary shunt vessels. N Engl J Med. Sep 21 2006;355(12):1262. doi:10.1056/NEJMicm050639.
- ↑ Moura FC, Fortini I. Optociliary Shunt Vessels: Role in Diagnosis and Treatment of Atypical Pseudotumor Cerebri. Neuroophthalmology. 2017:224-6. vol. 4.
- ↑ 18.0 18.1 Mashayekhi A, Shields JA, Shields CL. Involution of retinochoroidal shunt vessel after radiotherapy for optic nerve sheath meningioma. Eur J Ophthalmol. Jan-Feb 2004;14(1):61-4. doi:10.1177/112067210401400111
- ↑ 19.0 19.1 An SH, Jeong WJ. Early-scatter laser photocoagulation promotes the formation of collateral vessels in branch retinal vein occlusion. Eur J Ophthalmol. 2020 Mar;30(2):370-375. doi: 10.1177/1120672119827857. Epub 2019 Feb 5. PMID: 30722692.
- ↑ Heiferman MJ, Griebenow EJ, Gill MK, Fawzi AA. Morphological Implications of Vascular Structures Not Visualized on Optical Coherence Tomography Angiography in Retinal Vein Occlusion. Ophthalmic Surg Lasers Imaging Retina. 2018 Jun 1;49(6):392-396. doi: 10.3928/23258160-20180601-02. PMID: 29927465; PMCID: PMC6375291.
- ↑ 21.0 21.1 Suzuki N, Hirano Y, Tomiyasu T, Kurobe R, Yasuda Y, Esaki Y, Yasukawa T, Yoshida M, Ogura Y. Collateral vessels on optical coherence tomography angiography in eyes with branch retinal vein occlusion. Br J Ophthalmol. 2019 Oct;103(10):1373-1379. doi: 10.1136/bjophthalmol-2018-313322. Epub 2018 Nov 22. PMID: 30467130.