Ocular Prostheses, Scleral Shells, and Conformers
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Patients facing the loss or disfigurement of an eye often seek solutions to address aesthetic appearance. Ocular prostheses, scleral shells, and conformers are three options available, each with unique purposes (Table 1). It is important to remember to care for the remaining eye by wearing protective glasses (i.e. polycarbonate lenses) and getting regular ophthalmic exams. If blunt trauma was received, even if the remaining eye has not been directly affected by trauma, there is an increased risk of recessed angles, so all remaining eyes should also get a gonioscopy, along with full ophthalmic examination.[1]
| Ocular Prosthesis | Scleral Shell | Conformer |
|---|---|---|
| Permanent | Permanent | Temporary |
| No residual globe | Residual disfigured globe | No residual globe |
| Primarily cosmetic | Primarily cosmetic | Primarily protects sutured wounds |
| Used with orbital implant | Not used with orbital implant | Used with orbital implant |
| Used post-enucleation/evisceration | Used for congenital/traumatic globe disfigurement | Used post-enucleation/evisceration and for socket construction |
| Usually individually customized to match remaining eye | Can be individually customized or ordered from standard sizes/colors | Usually transparent but can sometimes be ordered with pupil, iris, and scleral coloring |
Ocular Prostheses
An ocular prosthesis is an artificial substitute for an absent eyeball following enucleation or evisceration. It is designed to fit over an orbital implant and under the eyelids.[2] Custom fit prosthesis are meticulously crafted to replicate the appearance of a natural eye. They are individually tailored to match the size, shape, color, and movement of the remaining natural eye. Stock ocular prosthetics are also available in countries without access to custom-fit prosthetics. Ocular prosthetics are usually made from rigid acrylic or soft silicone, making them durable and lifelike.[3]
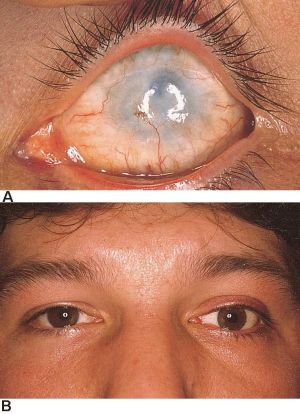
Scleral Shells
A scleral shell (Figure 1) is a prosthetic device fitted over a residual disfigured globe, like in cases of phthisis bulbi, atrophic bulbi, or microphthalmos. This is in contrast to an ocular prosthesis, which is fitted in an orbit with no residual globe.[4] Scleral shell prostheses are indicated when the palpebral aperture needs to be enlarged, the cornea is misshapen, or the disfigured eye has strabismus. Although stock scleral shells can be obtained from contact lens manufacturers that use set design parameters, better results are achieved by making fully customized scleral shells for the individual patient.[3]
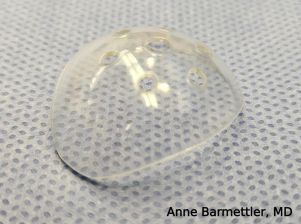
Conformers
Conformers (Figure 2) are temporary devices most commonly used in the early stages of eye socket rehabilitation after enucleation/evisceration. The conformers are meant to temporarily maintain deep conjunctival fornices to avoid scar contracture until the patient has healed enough to be fitted for a prosthesis (usually after 6 weeks). Fenestrations in the conformer prevent buildup of discharge and wound maceration.[5] They are available in stock sizes and are usually made from silicone or acrylic.[3]
Ocular conformers also have utility in the treatment of congenital anophthalmia/microphthalmia. The growing socket requires stimulation to grow, so children with congenital anophthalmia/microphthalmia will have facial asymmetry due to a smaller eye socket without intervention. In some cases, physicians can stimulate growth of eye sockets in patients with these conditions by using static acrylic conformers, which also slowly expand the lid fissure and conjunctival fornices. At regular intervals, the conformer is replaced with progressively larger versions until the socket has been serially enlarged to the appropriate size. This allows for suitable prosthesis with the best possible cosmetic appearance.[6]
Conclusions
Ocular prostheses, scleral shells, and conformers represent distinct options for patients requiring eye restoration or rehabilitation. Since the loss of an eye and/or its function can cause severe psychological trauma, an ocular prosthesis or scleral shell helps to improve quality of life by improving confidence and restoring ocular symmetry.[2] While ocular prostheses and scleral shells offer a customized and lifelike solution for patients post-enucleation or disfigured eyes, conformers serve as temporary protection in the post-operative healing process. Collaborative efforts between patients and ophthalmologists are essential in selecting the most suitable device based on individual needs and circumstances.
References
- ↑ Iannucci, Valeria, et al. “Bilateral Angle Recession and Chronic Post-Traumatic Glaucoma: A Review of the Literature and a Case Report.” Life. 2023;13(9):1814.
- ↑ 2.0 2.1 Sah, RK and Titiyal, JS. "Ocular Prosthesis: A Next Generation Cosmetic Management by an Eye for an Eye." J Ophthalmol & Vis Sci. 2023;8(2):1077.
- ↑ 3.0 3.1 3.2 Pine, Keith, et al. Clinical Ocular Prosthetics. Switzerland: Springer; 2015.
- ↑ Raizada, Kuldeep, and Rani, Deepa. "Ocular Prosthesis." Cont Lens Anterior Eye. 2007;30(3):152-62.
- ↑ Vincent, Andrea L, et al. “Prosthetic conformers: A step towards improved rehabilitation of enucleated children.” Clin Exp Ophthalmol. 2002;30(1):58–9.
- ↑ Watanabe, Akihide, et al. “Socket expansion with conformers in congenital anophthalmia and microphthalmia.” J Pediatr Ophthalmol Strabismus. 2022;26(6):318.e1-318.e6.