Ocular Manifestations of Hemophagocytic Lymphohistiocytosis Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease entity
Hemophagocytic lymphohistiocytosis (HLH) or hemophagocytic syndrome (HS) is a rare, life-threatening multi-system disorder of immune regulation that can result in end-organ damage most commonly involving the liver, central nervous system, and bone marrow and eventually death. The diagnosis of HLH is often challenging due to the diverse clinical manifestations and the presence of several diagnostic mimics. [1] Several ocular manifestations have been reported in association with HLH.
Types
HLH is classified as familial which is caused by inherited genetic mutations and acquired that arises because of external triggers like viral infection (most common trigger), malignancy, rheumatologic disease, stem cell transplantation, drug hypersensitivity, or other causes. [1] [2]
Epidemiology of Hemophagocytic lymphohistiocytosis disease
- The mean age at the time of HLH diagnosis is 1.8 years for familial HLH, while in acquired cases it is 50 years. [1] [3]
- The incidence of HLH ranges from 1 to 225 per 300,000 live births.
- Regarding adult population, there are fewer studies documenting the incidence and sex distribution. [1] [4]
Epidemiology of Hemophagocytic lymphohistiocytosis cases associated with ophthalmic manifestations
- The mean age at time of presentation was 30.21 (14.42) years.
- 94 patients (62%) were males and 58 patients (38 %) were females.
Pathophysiology
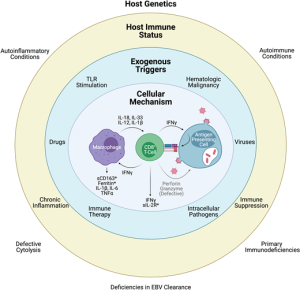
HLH is caused by Th1 proinflammatory cytokine dysfunction. There is hyperproduction of the cytokines that make up the Th1 profile including Interferon-γ, tumor necrosis factor-α, Interleukin (IL)-6, IL-10, IL-12, sIL-2 R (CD25), which results in T-lymphocyte and macrophage activation (Figure 1). [5] [6]
Criteria for diagnosis
The international major criteria for diagnosis include the following: [1] [2] [7]
- Fever.
- Splenomegaly.
- Cytopenia involving at least 2 cell types.
- Hypertriglyceridemia or hypofibrinogenemia.
- Hemophagocytosis demonstrated in the bone marrow, liver, or lymph node.
Risk factors for ophthalmic involvement:
A recent retrospective analysis conducted by Wang et al. screened HLH cases in a single center in China from 2013 to 2021. Out of 1525 HLH patients, 341 had ocular examinations, and 133 (133/341, 39.00%) had ocular abnormalities. The following risk factors were found to be significant to predict ocular affection: [8]
- Old age.
- Autoimmune disorders.
- Decreasing red blood cell count.
- Decreasing platelet count.
- Increasing fibrinogen level.
Ophthalmic manifestations of Hemophagocytic lymphohistiocytosis
- After reviewing the literature from 1968 till May 2023, a total of 152 patients of HLH were reported to have ophthalmic involvement .
- 14 patients were familial and 138 were acquired. Eptein-Barr Virus (EBV) Infection was the most common underlying cause.
- In the largest study by Wang et al. 2023 [8], posterior segment involvement was reported in 50 % (retinal hemorrhage was the most common sign), ocular surface infection in 38 %, uveitis in 8 %, adnexal abnormalities and strabismus in 6 %, and anterior segment complications in 4.5 %.
External examination:
- Lid edema: in 2 patients. [9][10]
- Strabismus and ocular motility limitation: in 3 patients. [8][11]
- Dacryoadenitis: in 2 patients.[8]
- Dacryocystitis: in one patient.[8]
- Orbital cellulitis: in 2 patients.[8]
- Orbital pseudotumor: in 2 patients.[8]
Ocular surface:
- Conjunctival chemosis: in 5 patients.[8]
- Conjunctivitis: in 34 patients.[8]
- Subconjunctival hemorrhage: in 11 patients. [8]
- Keratitis: in 16 patients.[8]
Anterior segment:
- Steroid-induced glaucoma: in 5 patients. [8]
- Radiation cataract: in one patient. [8]
Uveitis:
Posterior segment:
- Retinal hemorrhages: it is the most common ocular finding.
- Purtscher-like retinopathy: inner retinal whitening associated with cotton-wool spots were noticed in 1 patient. Optical coherence tomography (OCT) findings in the same patient were consistent with paracentral acute middle maculopathy (PAMM) lesion. [8]
- Retinal white lesions: 4 patients were reported to have white flat or sometimes fluffy lesions not associated with vitritis at the posterior pole around 2 disc diameter in size. [7][10][14][17]
- Serous retinal detachment: 10 patients had serous retinal detachment whether reported clinically or after OCT.[8][5][15][18] [19]
- Acute macular neuroretinopathy (AMN): outer plexiform layer hyperreflecitivity consistent with AMN was reported in 2 patients. [8]
- Cytomegalovirus retinitis: one patient was diagnosed with cytomegalovirus (CMV) retinitis. [8]
- Choroidal hypoperfusion: was found in one patient after OCT angiography, and in another patienton Indocyanine Green Angiography (ICGA). [14][17]
- Macular edema: OCT macula was done and revealed macular edema in 2 patients and ellipsoid zone disruption in one patient. [12][15][19]
Tissue pathology:
Histopathological assessment and immunohistochemistry were done in 4 patients after autopsy showing histocytic infiltration of mainly trabecular meshwork and choroid and to a lesser extent infiltration of retina, optic nerve, ciliary body and iris.[16][21]
Table illustrating the reported ophthalmic manifestations associated with HLH (Total 152 patients):
| Location | Opthalmic findings | Number of patients (%) |
|---|---|---|
| External examination | Lid edema | 2 (1 %) |
| Strabismus and ocular motility limitation | 3 (2 %) | |
| Dacryoadenitis | 2 (1 %) | |
| Dacryocystitis | 1 (0.6 %) | |
| Orbital cellulitis | 2 (1 %) | |
| Orbital pseudotumor | 2 (1 %) | |
| Ocular surface | Conjunctival chemosis | 5 (3%) |
| Subconjunctival hemorrhage | 11 (7%) | |
| Conjuctivitis | 34 (22%) | |
| Keratitis | 16 (10%) | |
| Anterior segment | Steroid-induced glaucoma | 5 (3%) |
| Radiation cataract | 1 (0.6 %) | |
| Uveitis | Anterior uveitis | 11 (7%) |
| Panuveitis | 2 (1 %) | |
| Posterior segment | Retinal hemorrhages | 55 (36 %) |
| Retinal white lesions | 4 (3%) | |
| Serous retinal detachment | 10 (7%) | |
| Purtscher-like retinopathy | 1 (0.6 %) | |
| Perivenous exudation and infiltrates | 3 (2 %) | |
| Acute macular neuroretinopathy | 2 (1 %) | |
| Cytomegalovirus retinitis | 1 (0.6 %) | |
| Choroidal hypoperfusion | 2 (1 %) | |
| Macular edema | 2 (1 %) | |
| Optic disc swelling | 15 (10%) | |
| Afferent pupillary defect | 2 (1 %) |
Prognosis of Hemophagocytic lymphohistiocytosis disease
- Familial HLH has a poor prognosis without treatment and has a median survival of 1 to 2 months. In adults the outcome is variable with the worst prognosis for malignancy-associated HLH. [1]
- Prognosis in patients associated with ophthalmic manifestations, 12 patients (6 in each category ) died within a few months shortly after presentation. Resolution of the condition followed by discharge was reported in only 3 acquired and 1 familial patients. However, there are no sufficient data in literature regarding the prognosis of the remaining patients.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Ponnatt TS, Lilley CM, Mirza KM. Hemophagocytic Lymphohistiocytosis. Arch Pathol Lab Med. 2022;146(4):507-519. doi:10.5858/arpa.2020-0802-RA
- ↑ Jump up to: 2.0 2.1 Al-Samkari H, Berliner N. Hemophagocytic Lymphohistiocytosis. Annu Rev Pathol Mech Dis. 2018;13:27-49.
- ↑ Niece JA, Rogers ZR, Ahmad N, Langevin AM, McClain KL. Hemophagocytic lymphohistiocytosis in Texas: Observations on ethnicity and race. Pediatr Blood Cancer. 2010;54(3):424-428.
- ↑ Hayden A, Park S, Giustini D, Lee AYY, Chen LYC. Hemophagocytic syndromes (HPSs) including hemophagocytic lymphohistiocytosis (HLH) in adults: A systematic scoping review. Blood Rev. 2016;30(6):411-420.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 Listernick R. A 6-year-old girl with “pink eye” for several months. Pediatr Ann. 2010;39(5):267-270.
- ↑ Janka GE, Lehmberg K. Hemophagocytic lymphohistiocytosis: pathogenesis and treatment. Hematology Am Soc Hematol Educ Program. 2013;2013(1):605-611.
- ↑ Jump up to: 7.0 7.1 Suhr KS, Chiang MF, Flynn JT, Engelbert M. Ocular involvement in hemophagocytic syndrome: A novel funduscopic manifestation and review of the literature. Retin Cases Br Reports. 2016;10(4):345-348.
- ↑ Jump up to: 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 8.13 8.14 8.15 8.16 8.17 8.18 8.19 Wang L, Suo L, Kou F, et al. Ocular Phenotypes in Patients with Hemophagocytic Lymphohistiocytosis: A Retrospective Analysis in a Single Center over 7 Years. Am J Ophthalmol.
- ↑ Jump up to: 9.0 9.1 Petersen RA, Kuwabara T. Ocular Manifestations of Familial Lymphohistiocytosis. Arch Ophthalmol. 1968;79(4):413-416.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 Kawamura H, Hatsukawa Y, Furukawa A, Inoue M, Kawa K. Ophthalmic findings in a case of hemophagocytic syndrome. Am J Ophthalmol. 1997;124(2):261-263.
- ↑ Jump up to: 11.0 11.1 Abu-Yaghi N, Obiedat A, Abdaljaleel M, Ar’ar T, Al-Abbadi M. Diplopia and Vision Loss Associated With Presumed Systemic Lymphohistiocytic Disease: A Case Report. Clin Med Insights Case Reports. 2022;15:11795476221137262.
- ↑ Jump up to: 12.0 12.1 Li X, Ma Y, Tang J, Chen T, Ma X. A Hemophagocytic Lymphohistiocytosis Patient that Presented with Unilateral Panuveitis. Ocul Immunol Inflamm. 2017;25(2):275-277.
- ↑ Liao PM, Thompson JT. Ophthalmic Manifestations of Virus-Associated Hemophagocytic Syndrome. Arch Ophthalmol. 1991;109(6):777.
- ↑ Jump up to: 14.0 14.1 14.2 14.3 Suzuki S, Mizota A, Adachi-Usami E. A case of hemophagocytic syndrome with retinal changes resembling acute posterior multifocal placoid pigment epitheliopathy. Retina. 2002;22(2):219-222.
- ↑ Jump up to: 15.0 15.1 15.2 Yao H, Liu Y, Ding W, Xu Y, Cheng Y. Ocular findings in a patient with virus-associated hemophagocytic syndrome. Ocul Immunol Inflamm. 2012;20(3):233-234.
- ↑ Jump up to: 16.0 16.1 Vizcaino MA, Eberhart CG, Rodriguez FJ. Hemophagocytic Lymphohistiocytosis in Adults with Intraocular Involvement: Clinicopathologic Features of 3 Cases. Ocul Oncol Pathol. 2017;4(1):1-11.
- ↑ Jump up to: 17.0 17.1 Lin BR, Pluym ID, Tsui I. Characterization of retinal lesions secondary to hemophagocytic lymphohistiocytosis with OCTA. Ophthalmic Surg Lasers Imaging Retin. 2019;50(10):653-655.
- ↑ Jump up to: 18.0 18.1 Lubin JR, Walton DS, Albert DM. Two cases of suspected familial erythrophagocytic lymphohistiocytosis. Am J Ophthalmol. 1981;91(6):743-749.
- ↑ Jump up to: 19.0 19.1 Lee EW, Mieler WF. Ocular findings in a patient with hemophagocytic syndrome. Arch Ophthalmol. 2006;124(11):1656-1658.
- ↑ Jump up to: 20.0 20.1 Appen RE, Weber SW, De Venecia G, Zu Rhein GM. Ocular and cerebral involvement in familial lymphohistiocytosis. Am J Ophthalmol. 1976;82(5):758-766.
- ↑ Jump up to: 21.0 21.1 21.2 Park JK. Ocular involvement in familial erythrophagocytic lymphohistiocytosis. Graefe’s Arch Clin Exp Ophthalmol. 1997;235(10):647-652.

