Occipital Epilepsy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
G40.109 Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures, not intractable, without status epilepticus.
Disease
Occipital epilepsy is characterized by occipital seizures originating from an epileptic focus within the occipital lobes.
Epidemiology
Occipital epilepsy comprises approximately 5 - 10% of all epilepsies. In reported demographic studies, the prevalence is 6%, comparable to the 5% seen among neurosurgical series[1]. In a population study of newly diagnosed epilepsy, occipital seizures were diagnosed in 1.2 - 1.6% of cases but this study noted the potential for under-diagnosis due to how occipital epilepsies can mimic other epilepsy syndromes and be misidentified[2].
Pathophysiology
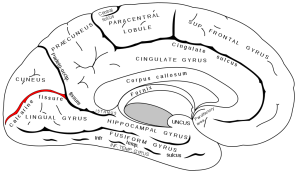
Seizures commonly spread from the occipital region to more anterior regions of the brain. Infracalcarine occipital foci spread to the ipsilateral medial temporal lobe in 50% of neurosurgical series. Supracalcarine foci tend to disseminate to the parietal and frontal regions in 12-38% of recorded neurosurgical series. Sensory and motor symptoms come from the lateral supracalcarine area. Complex posturing is secondary to medial supracalcarine spread.[1]
Etiology
The pathogenesis of occipital seizures is dependent on the underlying etiology. Etiologies can include:
Idiopathic occipital epilepsies:
- Idiopathic childhood occipital epilepsy of Gastaut:
- Idiopathic occipital epilepsy accounts for approximately 0.3% of newly diagnosed nonfebrile seizures and 2 - 7% of benign childhood focal seizures[3]. It is age-related with typical onset between 3-15 years and a mean age of 8. By the age of 16, two-thirds of the patient population has attained remission, with 50-60% having full resolution within 2-4 years after initial onset.[2]
- It is characterized by visual phenomena that consist of brief elementary visual hallucinations, ictal blindness, and deviation of the eyes. EEG shows occipital spikes and occipital paroxysms (when eyes are closed) due to fixation-off sensitivity. Most children require prophylactic antiseizure medications.[2][3]
- Idiopathic photosensitive occipital lobe epilepsy:
- Idiopathic photosensitive occipital lobe epilepsy is age-related with typical onset between 3-15 years old, mean age of 8. Reflex seizures are induced by video games, television, or other stimuli. By definition, all patients are photosensitive where photosensitivity refers to an abnormal clinical and/or electroencephalographic response to visual stimuli[4].[1]
- The current hypothesis on pathophysiology is that the excitatory response may be secondary to impaired visual cortical mechanisms of contrast gain control for specific patterns. However, there are theories that there may be a genetic influence, more likely polygenic, with the gene GRIN2A being increasingly recognized. Photosensitive family members are more likely to have photosensitive relatives, and there have been several family members within one family that demonstrate idiopathic photosensitive occipital lobe epilepsy or a related epileptic disorder[4]
- EEG patterns show either generalized or posterior occipital lobe epileptiform discharges with generalized bursts at rest and paroxysmal activity, or both secondary to photic stimuli.[4] A more recent study found that some patients were found to have seizures without photic stimuli.[4]
- Patients, especially those who experience spontaneous seizures, may require medical therapy in addition to stimuli avoidance. The prognosis depends on the severity of photosensitivity and seizures.[4]
Genetic diseases often associated with occipital lobe seizures:
- Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS)
- MELAS typically presents in childhood or adulthood with myopathy, deafness, lipomas, and short stature. It is characterized by episodic vomiting, migraines, seizures, and stroke-like episodes. It may lead to hemiparesis (reversible or permanent), hemianopia, or cortical blindness with focal particularly occipital seizures. Brain imaging may show lesions in the parieto-occipital region. Clinical diagnosis is supported by ragged red fibers on muscle biopsy. Other laboratory findings include lactic acidosis, elevated cerebrospinal fluid or proton MRS lactate, and myopathic changes on electromyography.
- Myoclonus epilepsy with ragged-red fibers (MERFF)
- MERFF is also associated with occipital epilepsy. The features of myopathy, deafness, optic atrophy, and lipomas may differentiate the two; however, DNA analysis may also be used to identify the mutation.
- Mitochondrial disease due to mutations in the POLG1 gene
- POLG1-related epilepsy has a preference for the occipital region on EEG and neuroimaging; however, there is no clear explanation as to why. On EEG, epileptiform and slow abnormalities were most frequently seen over occipital regions.[5] Valproate is contraindicated in this disorder due to potential liver failure.
- Lafora disease
- Lafora disease is an autosomal recessive, progressive myoclonus epilepsy caused by mutations in EPM2A or NHLRC1 that typically presents at ages 11-18 years old. Several types of seizures are associated - myoclonic, occipital, generalized tonic-clonic, absence, and atonic seizures - and gradually increase in frequency over time. With time, seizures become increasingly intractable, behavior and cognition deteriorate, and eventually the patient enters a vegetative state and potentially dies. Death results from status epilepticus, aspiration pneumonia, or other complications of chronic neurodegeneration[6].
- Panayiotopoulos syndrome:
- Panayiotopoulos syndrome (PS) describes a “multifocal childhood-related susceptibility to autonomic seizures and autonomic status epilepticus” and accounts for 6% of children with nonfebrile seizures. The age of onset is between 1 to 14 years, with 76% of cases starting between 3 and 6. PS is believed to be polygenic and has been associated with SCN1A mutations.[7]
- It is characterized by seizures that are often prolonged with half of seizures lasting greater than 30 minutes. Most patients have 1-5 seizures, therefore continuous prophylactic antiepileptics may not be needed. Instead, patients rely on abortive therapy with benzodiazepines (midazolam) to terminate autonomic status epilepticus. In more than half of patients, seizures resolve in 4 years.
Symptomatic occipital epilepsies secondary to structural or other identifiable lesions:
- Congenital:
- Sturge-Weber disease (rare)
- Structural lesions:
- Focal cortical dysplasia:
- Cortical dysplasia is characterized by poor delineation of the gray-white matter interface, focal cortical thickening, and subcortical white matter T2 prolongation secondary to glial proliferation. Clinical onset usually occurs within the first two decades of life.[2] Typically, this disorder is refractory to anti-seizure medications and does better with surgical resection which can relieve frequency but complete seizure relief is rare[8].
- Heterotopia
- The occipital region is a common region for focal periventricular heterotopia (PVH), typically seen bilaterally rather than unilaterally. When unilateral, there appears to be a predilection for the right side. Occipital seizures typically develop in the second decade with onset ranging from early childhood to the fourth decade. Most patients have medically refractory epilepsy, and surgery has also had disappointing results. Theoretically, the epileptogenic zone may be larger than the nodules that appear on imaging.[2]
- Polymicrogyria
- Polymicrogyria is characterized by multiple small gyri, either focal or diffuse, with abnormal cortical lamination. It is thought to occur due to developmental disorder or injury that occurs during neuronal migration or in early cortical organization. However, it has also been linked to the gene GPR56[9]. Chronic occipital epilepsy can be associated with unilateral or bilateral focal polymicrogyria and typically manifests as complex partial seizures with automatisms in the first or second decade of life. Typically, patients do not have major visual field deficits.[2]
- Tuberous sclerosis
- Vascular malformations
- Ding et al. conducted a retrospective study involving 1000 patients with arteriovenous malformations (AVM) who were screened for epilepsy. They reported that 229 of the patients were found to have epilepsy, of those with occipital AVMs however had the lowest rate of seizure (21.5%). The pathophysiology of epilepsy secondary to AVMs is still limited but there are several hypotheses including neuronal degeneration and aberrant signaling, generation of reactive oxygen species, alterations in glial structure, and an imbalance of excitatory and inhibitory activity[12]. Cerebral cavernous malformations (CCMs) are another vascular malformation that may cause occipital epilepsy. Diagnosis is primarily diagnosed by imaging (47% of the time) and other manifestations less often: convulsions (25%), intracerebral hemorrhage (12%), and focal neurological deficits (15%)[13]. CCMs may either be sporadic or familial and are associated with malformations in the genes encoding CCM1, CCM2, and CCM3 which are proteins in the vascular endothelial cells that regulate signal transduction. Mutations result in hemangioma formation and abnormal intercellular junctions.
- Intraoccipital or extraoccipital lobe tumors
- One case report discussed an intracerebral schwannoma in the parieto-occipital lobe which manifested as an epileptic episode; however, intracerebral schwannomas are rare.[14] The majority of intracerebral schwannomas are located in the temporal and frontal regions.[12] There is also a retrospective study that reported the prevalence of seizures in patients with brain tumors was higher when the lesions were in the frontal lobe compared to the occipital lobe[15].
- Reversible posterior leukoencephalopathy syndrome
- Focal cortical dysplasia:
Metabolic Disorders:
- Celiac disease (CD):
- Celiac disease has been linked to epilepsy. Studies have shown that epilepsy is 1.8 times more prevalent in patients with CD compared to the general population[16]. Among patients with occipital lobe epilepsy, the prevalence of CD is two to three times higher than in the normal population. The prevalence is reported to be 2-3% however different studies report different frequencies. Gluten-free diets (GFD) have been shown to manage epilepsy by either reducing seizure frequency and/or reducing the need for antiepileptic drugs; however, it is unclear whether GFD directly resolved the seizures or improved the absorption of medical therapy. As opposed to other forms, epilepsy associated with CD appears to be more resistant to monotherapy, therefore screening for CD is recommended in children with resistant epilepsy[17].
- CEC Syndrome refers to the triad of CD, Epilepsy, and Calcification in the occipital lobe. According to a systematic review, the majority of cases (82%, n = 131) demonstrated posterior calcifications with the remainder located in the frontal, temporal, or in the subcortical areas. The incomplete form is cerebral calcifications and CD without epilepsy. CEC is associated with HLA-DQ2 and HLA-DQ8, however, the pathophysiology and whether CEC is a genetic condition is unknown[18].
Situation-related occipital seizures or conditions with occipital epileptic seizures that are traditionally not diagnosed as a form of epilepsy:
- Occipital seizures secondary to an acute metabolic or toxic event (i.e. eclampsia, nonketotic hyperglycemia, alcohol, drugs)[19][1]
- Isolated provoked occipital seizures during prolonged exposure to video games without evidence of photo or pattern sensitivity.[1]
- Incidental occipital seizures induced by vigorous photic stimulation in EEG departments in otherwise normal subjects.[1]
Diagnosis
Diagnosis relies on a detailed history and EEG findings. Neuroimaging studies may be done to rule out other etiology but are not necessary for diagnosis.
History
A history of visual hallucinations, and external manifestations (listed under symptoms) should be investigated. In children, additional critical signs include vomiting, pallor, and eye deviation.[1]
Symptoms & Signs
Symptoms are typically visual and oculomotor and may be classified as subjective, objective, or both.
Subjective:
Visual subjective symptoms are characterized by transient visual symptoms that may be positive (flashes, phosphenes) or negative (amaurosis, hemianopia, scotoma).
- Positive visual hallucinations typically present unilaterally in the temporal visual field contralateral to the epileptogenic focus. Approximately 10-30% of the time, they appear centrally or in an undefined location. After their initial presentation, they may multiply, increase in size, or change positions and luminance depending on the progression.
- Flickering or flashing is common, translation in a two-dimensional plane is less common, and rotation or moving towards or away is rare. In terms of appearance, they are usually multicolored and circular. Other shapes are rare but become more complex if the occipito-temporal cortex is involved. In rare instances, the patient may see their own image (heautoscopy).[19]
- Elementary visual hallucinations often progress to other manifestations after spreading to various regions.
- Perceptive illusions where an object appears to be distorted may also occur. Simple perceptive illusions refer to distortion in size (macropsia, micropsia), shape (metamorphopsia), illumination, color, or clarity.
- Complex illusions refer to objects that appear disoriented in the distance (macroproxiopia, microtelepsia), or appear to be distant and minute (teleopsia).
- Alternatively, the patient may have decreased or enhanced stereoscopic vision or have persistent or recurrent palinopsia. Additionally, patients may also experience palinopsia, sensory hallucinations of ocular movements, or blindness. Ictal blindness may present secondary to visual hallucinations or as an initial manifestation. Occasionally, it may be the only manifestation. Ictal blindness and ictal hemianopia (occurs less frequently) occur in 33% of patients with symptomatic and 67% of patients with idiopathic occipital epilepsy.[1]
- Postictally, headaches that feel similar to migraines occur in >50% of cases. After severe seizures or status epilepticus, the patient may experience blindness.[2]
Objective:
- Objective oculomotor symptoms include oculoclonic movements, nystagmus, palpebral jerks, or repetitive eyelid closure or fluttering which usually occur after visual hallucinations conclude and consciousness is impaired.
- Pursuit-like tonic deviation occurs in 40-50% of cases which is often followed by an ipsilateral turning of the head.
- Other objective symptoms include autonomic features, emesis, ictal headache, ocular pain, tinnitus, vertigo, rapid-onset seizures lasting a few seconds to 3 minutes, and status epilepticus. Autonomic features are classically associated with benign childhood seizure susceptibility syndrome. The tinnitus and vertigo are hypothetically related to epileptic spread to the posterior temporoparietal region.
- Additionally, other manifestations of epilepsy representative of foci or spread to alternate areas of the brain may appear.[1]
Diagnostic procedures
Interictal scalp EEG frequently demonstrates abnormal findings with characteristic findings specific to underlying etiologies. The most common finding overall is posterior temporal activity. Other findings include bilateral frontally predominant paroxysms and wide distribution diffuse posterior sharp or spike activity.[1] EEGs may record bilateral epileptiform discharges from each occipital lobe. The lower voltage discharges indicate secondary spread. It is important to note that EEG findings may not show an occipital origin of the seizure, but may instead catch the spread to the posterior temporal, parietal, and frontal regions. Dissemination of the seizure to the opposite occipital lobe may be rapid in children but a late finding in adults.[2]
In idiopathic occipital lobe epilepsy, the most common EEG abnormalities are occipital spikes and/or occipital paroxysms (90% prevalence).[1] The classic pattern consists of nearly continuous high amplitude, rhythmic 2-3 Hz, unilateral or bilateral posterior sharp and slow wave complexes with “fixation-off” sensitivity (the phenomenon of activating epileptiform activity when fixation is lost).[2] However, the majority of children with idiopathic epilepsy appear to show occipital spikes facilitated by sleep, without any relation to “fixation-off” sensitivity.[1]
In Panayiotopoulos syndrome, occipital paroxysms and spikes may occur concurrently with extraoccipital spikes and/or brief generalized discharges.[1]
In idiopathic photosensitive occipital epilepsy, EEG demonstrates occipital paroxysms at a wide range of flash frequencies.
Neuroimaging (MRI, CT) may be used to identify structural abnormalities.
If suspected, celiac disease may be screened for.[2] Lafora disease and MELAS have additional diagnostic biopsies that may be collected.[2]
Differential diagnosis
Migraines should be ruled out due to the similar presentation to occipital epilepsy. The visual symptoms of migraines typically last for several minutes (average 15-20 minutes) and can present as flickering, scintillating, zigzag, fortification scotomas within the central field with march and build-up, compared to the more transient, colorful, geometric visual symptoms associated with occipital epilepsy.[2]
Other causes of visual hallucinations may include but are not limited to the following: ocular pathology, Charles Bonnet Syndrome, peduncular hallucinosis, narcolepsy, delirium, psychosis, drug-induced, or secondary to alcohol withdrawal.
Management
General treatment
Medical or surgical treatment may be used depending on the etiology and severity of occipital epilepsy.
Medical therapy
Antiseizure medications are recommended including carbamazepine, lamotrigine, levetiracetam, oxcarbazepine, and topiramate.[1] Carbamazepine is the most commonly used in children with idiopathic occipital epilepsies with 90% clinical response.[7] Sodium valproate may be useful in children with idiopathic photosensitive occipital epilepsy.[1]
Surgery
For those with medically refractory occipital epilepsy, surgery is increasingly being considered with overall long-term seizure resolution in 46-65% of cases.[20] Depending on the underlying etiology, the outcomes range from 45% (developmental abnormalities) to 85% (tumors).[10] Resection of tumors has nearly uniform seizure control as opposed to resection of developmental abnormalities, which is less uniform which may account for the difference in efficacy.[6] Additionally, within the developmental causes of occipital epilepsy, low-grade focal cortical dysplasias had better outcomes than heterotopia and hamartoma regardless of surgical procedure.[10]
Total excision of a lesion compared to partial excision has better outcomes, although total lesionectomy versus occipital lobectomy does not predict outcome.[2]
Low-grade focal cortical dysplasias have better surgical outcomes than heterotopia and hamartoma regardless of type of surgery performed.[10]
EEG findings may help predict surgical outcomes - localized discharges are typically associated with better outcomes.[2] Inactive postoperative scalp EEG and electrocorticography also predict better outcomes.[2]
Complications
The most common complication is a visual field defect.[1][2] Post-surgical visual field defects have been reported in 20-76% of patients, which is lower than predicted, therefore there are theories that cortical reorganization occurs in some patients.[2] Neuroimaging including ictal SPECT and ictal PET scans may confirm the area of resection prior to surgery.[2] Intraoperative mapping through electrocortical stimulation under awake conditions has been used to preserve visual integrity, however it is still not widely used[20].
Prognosis
The prognosis varies depending on the underlying etiology.
Additional Resources
https://www.aao.org/bcscsnippetdetail.aspx?id=756ae97b-827c-4865-8733-1a5cc969b36d
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Adcock, Jane E.; Panayiotopoulos, Chrysostomos P.. Occipital Lobe Seizures and Epilepsies. Journal of Clinical Neurophysiology: October 2012 - Volume 29 - Issue 5 - p 397-407 doi: 10.1097/WNP.0b013e31826c98fe
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 Isabella Taylor, Ingrid E. Scheffer, Samuel F. Berkovic, Occipital epilepsies: identification of specific and newly recognized syndromes, Brain, Volume 126, Issue 4, April 2003, Pages 753–769, https://doi.org/10.1093/brain/awg080
- ↑ 3.0 3.1 Caraballo R, Koutroumanidis M, Panayiotopoulos CP, Fejerman N. Idiopathic childhood occipital epilepsy of Gastaut: a review and differentiation from migraine and other epilepsies. J Child Neurol. 2009;24(12):1536-1542. doi:10.1177/0883073809332395
- ↑ 4.0 4.1 4.2 4.3 4.4 Politi-Elishkevich K, Kivity S, Shuper A, Levine H, Goldberg-Stern H. Idiopathic photosensitive occipital epilepsy: clinical and electroencephalographic (EEG) features. J Child Neurol. 2014;29(3):307-311. doi:10.1177/0883073812473366
- ↑ Specchio N, Pietrafusa N, Calabrese C, et al. POLG1-Related Epilepsy: Review of Diagnostic and Therapeutic Findings. Brain Sci. 2020;10(11):768. Published 2020 Oct 23. doi:10.3390/brainsci10110768
- ↑ 6.0 6.1 Nitschke F, Ahonen SJ, Nitschke S, Mitra S, Minassian BA. Lafora disease - from pathogenesis to treatment strategies. Nat Rev Neurol. 2018;14(10):606-617. doi:10.1038/s41582-018-0057-0
- ↑ 7.0 7.1 Emmady PD, M Das J. Benign Occipital Seizure. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 8, 2022.
- ↑ Spreafico R, Blümcke I. Focal Cortical Dysplasias: clinical implication of neuropathological classification systems. Acta Neuropathol. 2010;120(3):359-367. doi:10.1007/s00401-010-0714-x
- ↑ Jansen A, Andermann E. Genetics of the polymicrogyria syndromesJournal of Medical Genetics 2005;42:369-378.
- ↑ 10.0 10.1 10.2 10.3 Aykut-Bingol C, Bronen RA, Kim JH, Spencer DD, Spencer SS. Surgical outcome in occipital lobe epilepsy: implications for pathophysiology. Ann Neurol. 1998;44(1):60-69. doi:10.1002/ana.410440112
- ↑ Guerreiro MM, Andermann F, Andermann E, et al. Surgical treatment of epilepsy in tuberous sclerosis: strategies and results in 18 patients. Neurology. 1998;51(5):1263-1269. doi:10.1212/wnl.51.5.1263
- ↑ 12.0 12.1 Ding D, Starke RM, Quigg M, et al. Cerebral Arteriovenous Malformations and Epilepsy, Part 1: Predictors of Seizure Presentation. World Neurosurg. 2015;84(3):645-652. doi:10.1016/j.wneu.2015.02.039
- ↑ Ishii K, Tozaka N, Tsutsumi S, Muroi A, Tamaoka A. Familial cerebral cavernous malformation presenting with epilepsy caused by mutation in the CCM2 gene: A case report. Medicine (Baltimore). 2020;99(29):e19800. doi:10.1097/MD.0000000000019800
- ↑ Haga Y, Shoji H, Oguro K, et al. Intracerebral Schwannoma--case report. Neurol Med Chir (Tokyo). 1997;37(7):551-555. doi:10.2176/nmc.37.551
- ↑ Hamasaki T, Yamada K, Kuratsu J. Seizures as a presenting symptom in neurosurgical patients: a retrospective single-institution analysis. Clin Neurol Neurosurg. 2013;115(11):2336-2340. doi:10.1016/j.clineuro.2013.08.016
- ↑ Julian T, Hadjivassiliou M, Zis P. Gluten sensitivity and epilepsy: a systematic review. J Neurol. 2019;266(7):1557-1565. doi:10.1007/s00415-018-9025-2
- ↑ Dai AI, Akcali A, Varan C, Demiryürek AT. Prevalence of resistant occipital lobe epilepsy associated with celiac disease in children. Childs Nerv Syst. 2014;30(6):1091-1098. doi:10.1007/s00381-014-2387-6
- ↑ Gobbi G. Coeliac disease, epilepsy and cerebral calcifications. Brain Dev. 2005;27(3):189-200. doi:10.1016/j.braindev.2004.05.003
- ↑ 19.0 19.1 Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989;30(4):389-399. doi:10.1111/j.1528-1157.1989.tb05316.x
- ↑ 20.0 20.1 Joswig H, Girvin JP, Blume WT, Burneo JG, Steven DA. Awake perimetry testing for occipital epilepsy surgery. J Neurosurg. 2018;129(5):1195-1199. doi:10.3171/2017.6.JNS17846