Multiple Evanescent White Dot Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Multiple Evanescent White Dot Syndrome
Background
Multiple Evanescent White Dot Syndrome (MEWDS) is one of the diagnoses within the family of White Dot/ White Spot Syndromes, first described by Jampol L. M and colleagues.[1] Within this diagnostic group are MEWDS, Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPEE), Multifocal Choroiditis and Panuveitis (MCP), Punctate Inner Choroiditis (PIC), and Birdshot Chorioretinopathy. The White Dot Syndromes produce yellow-white retinal lesions classically located at the retinal pigment epithelium or outer retina and are found primarily in young adults. Symptoms of MEWDS include unilateral blurred vision, visual field loss, photopsias, and floaters. The various diagnoses are differentiated by history, appearance, laterality, and fluorescein angiogram findings.
Symptoms and Demographics
The typical patient with MEWDS is a healthy middle aged female age 15-50. There is a gender disparity as women are affected with MEWDS four times more often than men. Roughly 30% of patients have experienced an associated viral prodrome. Some cases of MEWDS have been reported following COVID vaccination, although the relationship between the two is unclear. Patients present with acute, painless, unilateral change in vision. They may notice photopsias, dyschromatopsia, or a temporal or paracentral scotoma. Majority of the cases have unilateral involvement, but bilateral MEWDS has been described rarely and is usually asymmetric.
Course
Though the onset is acute, the disease is typically self limiting and recurrences are rare. Visual prognosis is excellent.
Exam Findings
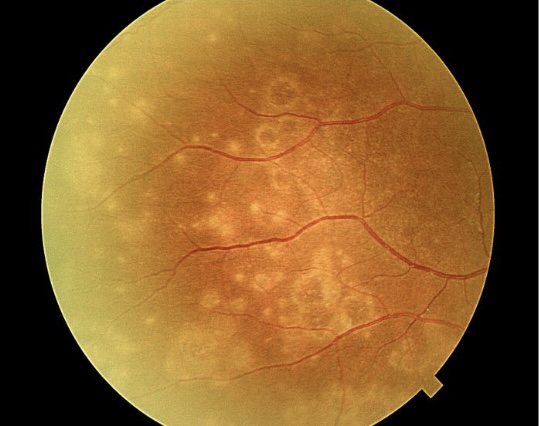
On fundus exam, one sees flat, multifocal, grey-white lesions (100-200 microns), appearing to reach as deep as the RPE. Typically lesions are found outside the fovea in the posterior pole. A characteristic finding in MEWDS is an orange-yellow fovea with granularity. One might also note optic disc edema, mild vitritis (usually posterior vitreous cells), mild anterior chamber flare, a relative afferent pupillary defect and an enlarged blind spot. Sheathing of retinal veins and superficial retinal hemorrhages are rarely seen. Peripapillary serous subretinal fluid has been described in a few young women with MEWDS.
Testing
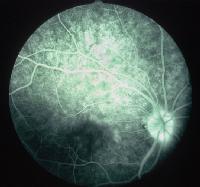
Fluorescein angiography
FA reveals early punctate hyperfluorescence in a wreath-like pattern and late staining, in areas corresponding to the white dots. This hyperfluorescence may be due to dilated retinal microcirculation in middle or deep retinal capillary plexus.[2] Retinal vascular sheathing and optic nerve staining may be seen in some patients with MEWDS. This early hyperfluorescence and late staining is in contrast to acute posterior multifocal placoid pigment epitheliopathy (APMPPE) where early hypofluorescence is seen followed by late hyperfluorescence.
Fundus Autofluorescence
FAF is a quick and non-invasive method of establishing a diagnosis. Hyperautofluorescent dots correlate with the white dots seen on fundoscopy. Even in the absence of white dots on clinical examination, FAF can show characteristic hyperautofluorescent lesions. Recent reports suggest that FAF may be the most sensitive and practical ancillary test to detect MEWDS.
Optical coherence tomography
Discontinuities in inner segment-outer segment junction[3][4] and mild attenuation of external limiting membrane[3] have been reported in acute phase. Recurrent episodes may result in thinning of outer nuclear layer.[4]
Visual field
An enlarged blind spot is typically seen. Other features include a central or paracentral scotoma. Acute Idiopathic Blind Spot Enlargement Syndrome may represent a form of the same disease process.
Indocyanine green angiography (ICGA)
In multiple evanescent white dot syndrome, no defects are usually noted in the early phase but dark hypocyanescent spots, typically outnumbering the clinical lesions are seen at late phase of ICGA.[5]
Electroretinogram
Changes are reversible. A reduced a-wave amplitude may be seen and early receptor potential may be prolonged.
Electroculogram
A reversible decrease in Arden's ratio may be noted.
Visual evoked responses may show a reversible decrease in amplitude and prolongation of latency.
Pathogenesis and Treatment
Frequently, a viral prodrome is elicited from the patient, though an infectious etiology is yet to be elucidated. The exact pathogenesis is unknown. Imaging modalities such as ICGA and SD-OCT suggest the disease is caused by vaso-occlusive problems of choriocapillaris producing transient ischaemia in the outer retina and reversible damage to the outer segments of the photoreceptors. Early and late hyperfluorescent lesions on the FA may represent reactive retinal vasodilatation and exudation caused by hypo or non-perfusion of choriocapillaris.[6]
Since MEWDS is a self-limited disease, with almost all patients regaining good visual acuity within 3-9 weeks, no treatment is recommended. Photopsias and scotomata gradually resolve and the lesions will disappear and may be replaced by mild pigment mottling or chorioretinal scarring. MEWDS typically is a self-limited disease, however, patients with MEWDS may have persistent blind spot enlargement. While it is uncommon, 10% of patients may also experience a recurrence. The prognosis is relatively good for these patients.
Additional Resources
- Basic and Clinical Science Course. United States: American Academy of Ophthalmology, 2010.
- Buggage, R. White Dot Syndrome. Focal Points: Clinical Modules for Ophthalmologists. June 2007. Vol 25(4).
- Emedicine. 13 July 2006. 11 July 2007. www.emedicine.com/oph/topic718.htm
- Friedman, et al. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. Philadelphia: W.B. Saunders Co.; 1998.
- Ho A, Brown G, et al. Color Atlas and Synopsis of Clinical Ophthalmology: Retina. McGraw-Hill publishing. New York. 2003.
- Hy Harvey. White Dot Syndromes. The Ocular Immunology and Uveitis Foundation. http://www.uveitis.org/medical/articles/case/wds.html.
- Jampol LM, Sieving PA, Pugh D, et al: Multiple evanescent white dot syndrome. Clinical findings. Arch Ophthalmol 1984 May; 102(5): 671-4.
- Quillen D, Davis J, et al. Perspective: The White Dot Syndromes. American Journal of Ophthalmology 2004; 137:538-550.
- Quillen D, Blodi B. Clinical Retina. United States: American Medical Association Press, 2002.
- Tewari A, Elliot D. emedicine. 8 June 2005. 11 July 2007. http://www.emedicine.com/OPH/topic749.htm
- Joseph A, Rahimy E, Freund KB, et al. Fundus autofluorescence and photoreceptor bleaching in multiple evanscent white dot syndrome. Ophthalmic Surg Lasers Imaging Retina. 2013 Nov 1;44(6):588-92.
- Images used with permission from emedicine
References
- ↑ Jampol, Lee M. “Multiple Evanescent White Dot Syndrome: I. Clinical Findings.” Archives of Ophthalmology 102, no. 5 (May 1, 1984): 671. doi:10.1001/archopht.1984.01040030527008.
- ↑ Tavallali A, Yannuzzi LA. MEWDS, Common Cold of the Retina. J Ophthalmic Vis Res. 2017 Apr-Jun;12(2):132-134. doi: 10.4103/jovr.jovr_241_16.
- ↑ 3.0 3.1 Lavigne, Luciana Castro, David Leonardo Cruvinel Isaac, José Osório Duarte Júnior, and Marcos Pereira de Avila. “Transient Spectral Domain Optical Coherence Tomography Findings in Classic MEWDS: A Case Report.” Arquivos Brasileiros De Oftalmologia 77, no. 3 (June 2014): 185–87.
- ↑ 4.0 4.1 Nguyen, My Hanh T., Andre J. Witkin, Elias Reichel, Tony H. Ko, James G. Fujimoto, Joel S. Schuman, and Jay S. Duker. “Microstructural Abnormalities in MEWDS Demonstrated by Ultrahigh Resolution Optical Coherence Tomography.” Retina (Philadelphia, Pa.) 27, no. 4 (May 2007): 414–18. doi:10.1097/01.iae.0000246676.88033.25.
- ↑ Yen MT, Rosenfeld PJ. Persistent indocyanine green angiographic findings in multiple evanescent white dot syndrome. Ophthalmic Surg Lasers. 2001 Mar-Apr;32(2):156-8. PMID: 11300640.
- ↑ Papasavvas I, Mantovani A, Tugal-Tutkun I, Herbort CP Jr. Multiple evanescent white dot syndrome (MEWDS): update on practical appraisal, diagnosis and clinicopathology; a review and an alternative comprehensive perspective. J Ophthalmic Inflamm Infect. 2021 Dec 18;11(1):45. doi: 10.1186/s12348-021-00279-7. PMID: 34921620; PMCID: PMC8684571.