Monocular Occipital Temporal Crescent Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Retro-chiasmal lesions typically present with contralateral homonymous visual field defects. Temporal crescent syndrome, which occurs from a lesion in the anterior occipital cortex, however, is an exception to this rule. Temporal crescent syndrome presents as a monocular loss of a crescent shape visual field in the temporal and peripheral vision contralateral to the lesion.[1]
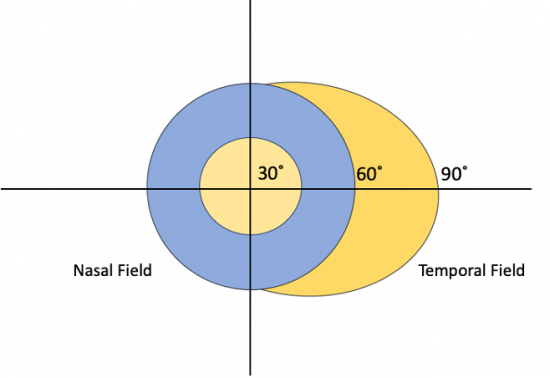
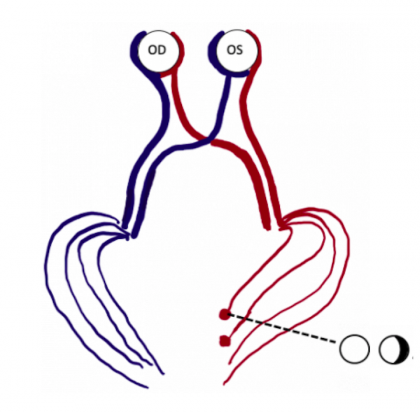
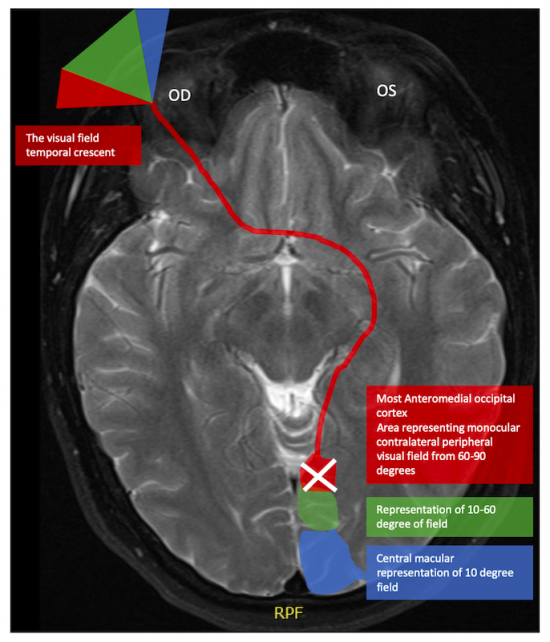
The etiology for this special monocular visual field defect is due to the distribution and overlap of the nasal and temporal visual fields. The normal visual field in degrees from the central point is 60 degrees nasal, 50 degrees superiorly, and 90-100 degrees temporally (Figure 1). The nasal and temporal hemifields in each eye overlap but the monocular temporal crescent has no perimetric correlate in the fellow eye because the temporal visual field is larger than the nasal visual field, hence there are more crossing nasal fibers than there are ipsilateral temporal fibers with a 53:47 ratio. [2] The extra nasal fibers that cross accounts for the non-overlapping contralateral temporal crescent. These fibers end up in the most anterior medial striate cortex and compromise 8-10% of the striate cortex. [3] This monocular representation in a retrochiasmal pathology is attributed to the monocular innervation in that area.[4] Thus, 30-40 degrees of the peripheral temporal visual field is unpaired and has unilateral representation in the contralateral visual cortex. Damage to this area of the visual cortex leads to the contralateral temporal crescent (Figure 2.)[5][6]
Etiology
The monocular temporal crescent syndrome can be congenital or acquired. In cases of congenital lesions, a complete homonymous hemianopsia may spare or involve the temporal crescent. Patients with congenital occipital lobe lesions may be asymptomatic. In acute acquired occipital lesions (e.g., occipital hemorrhage or stroke) the defect may be noticed acutely. However, slowly progressive lesions (e.g., occipital tumor, neurodegenerative disease or arteriovenous malformations) may produce symptoms over months to years,[7] [8] Other symptoms and signs (e.g., headache) may also be present in occipital lesions. [8]
Yamaguchi et al. first described the absence of the temporal crescent in a lateral ventricular glioependymal cyst [5] but the most common cause in adults is a vascular event. [9] Other cases reported to cause temporal crescent syndrome include vascular lesions [7], moderate peripartum hypertension, [7] Creutzfeldt-Jakob disease (CJD), [9] hemorrhagic infarction of the anterior aspect of the parieto-occipital sulcus in a patient with seizure,[6] and arteriovenous malformation with compression on the medial anterior visual cortex. [7]
Diagnosis
History
Patients may present with an isolated monocular crescent or other symptoms depending on localization. A history of stroke, birth injury, trauma, aneurysm, seizure, or migraine may be helpful. Severe headache accompanied by nausea, photophobia, along with the visual loss may occur, also patients with a missing temporal crescent may showcase other neurological deficits.[1][5][6][7][8][9][10]
Exam
Any patient presenting with a monocular temporal crescentic visual field defect should have a full neuro-ophthalmic and ocular exam to exclude intraocular causes of the visual field loss (e.g., retinal detachment). A relative afferent pupillary defect (RAPD) is generally present in such cases ipsilateral to the retinal or optic nerve lesion, whereas in a unilateral missing temporal crescent there is no RAPD. It has been shown that a quick test can be used by the examiner by moving their hand slowly behind the patient's head, anteriorly, showcasing that the temporal visual field border extends beyond 90 degrees. Confrontation visual field testing may be helpful in documenting the peripheral crescentic field loss. The test can be used to detect constriction of the temporal aspect of the visual field but may not include all of the temporal peripheral field because the examiner’s hand is not long enough to enter the temporal crescent out of the blind area.[7]
Investigations
Visual field
Although Goldmann Kinetic Perimetry can detect the temporal crescentic peripheral field defect it is not universally available. The largest stimulus should be presented at the edge of the cupola, to include the temporal crescent for best results. [7] It is important to understand that since lesions that cause a missing temporal crescent begin approximately 60 degrees from fixation, the central field is normal, and the nasal retinal periphery should be carefully examined ophthalmoscopically. [1] Unfortunately, current central (30-2 or 24-2) automated perimetry (e.g., Humphrey Visual Field Analyzer) cannot detect a temporal crescent (which is beyond the central 30 degrees). [8] Some automated perimetry can test the peripheral visual field but the normative database is not as robust for such larger visual field tests.
Radiographic imaging
Patients with an acute onset of the temporal crescent syndrome should undergo neuroimaging. Typically, computed tomography (CT) scan is the initial imaging to determine the underlying etiology in the acute setting (e.g., hemorrhage). If the CT scan is non-diagnostic or if further delineation of a CT lesion is necessary, then magnetic resonance imaging (MRI) may be helpful in the absence of pathology on CT scan. Gradient echo sequences and T2 weighted spin-echo sequences can be used to detect subtle lesions (e.g., hemorrhage) in the monocular temporal crescent syndrome. [1][5][6][7][9][10]
Treatment
Management, treatment, and prognosis depend on the underlying etiology of the syndrome.[5]
The Preserved Temporal Crescent
Banton et al, described homonymous hemianopia visual field defects in 4 of their patients with preservation of the temporal crescent ,[11] one of the theories of this preservation is that the striate cortex is supplied by 4 different vessels with variable dominance which accounts for the different types of field defects manifesting in an occipital injury; the calcarine, posterior temporal and parieto- occipital branches of the posterior cerebral artery and occipital branches of the anterior cerebral artery.[12] This finding usually implies contralateral occipital lobe ischemia sparing less than 10% of striate cortex (or geniculocalcarine connections).[10] However, in the case series by Lepore , 19% of patients with preserved temporal crescent had lesions confined to the optic radiations rather than striate cortex. [10]
Summary
Clinicians should be aware that a monocular temporal crescent visual field defect (temporal crescent syndrome) can occur from a contralateral, anterior occipital cortex lesion. The etiology for the temporal crescent syndrome is typically ischemic infarction or hemorrhage in the acute setting but neoplastic, infectious, infiltrative, and vascular malformation etiologies may also occur. An RAPD should not be present in occipital lesions and careful examination of the retina and optic nerve should be performed to exclude non-occipital causes for the visual field loss. CT or MR scan of the brain may be necessary to confirm the diagnosis and etiology. Treatment should be directed at the underlying cause.
References
- ↑ 1.0 1.1 1.2 1.3 Chavis PS, Al-Hazmi A, Clunie D, Hoyt WF. Temporal crescent syndrome with magnetic resonance correlation. Journal of neuro-ophthalmology. 1997 Sep 1;17(3):151-5.
- ↑ Kupfer C, Chumbley L, De J, Downer C. Quantitative histology of optic nerve, optic tract and lateral geniculate nucleus of man*. Vol. 101, J. Anat. 1967.
- ↑ Horton JC, Dagi LR, McCrane EP, de Monasterio FM. Arrangement of ocular dominance columns in human visual cortex. Arch Ophthalmol. 1990 Jul;108(7):1025-31. doi: 10.1001/archopht.1990.01070090127054. PMID: 2164380.
- ↑ Miki A, Liu GT, Raz J, van Erp TG, Liu CJ, Leuthardt EC, et al. Contralateral Monocular Dominance in Anterior Visual Cortex Confirmed by Functional Magnetic Resonance Imaging. 2000.
- ↑ 5.0 5.1 5.2 5.3 5.4 Yamaguchi I, Pooh KH, Azumi M, Takagi Y. Temporal crescent syndrome caused by a lateral ventricular glioependymal cyst: case report. Journal of Neurosurgery: Pediatrics. 2020 May 15;1(aop):1-5.
- ↑ 6.0 6.1 6.2 6.3 Ali K. The temporal crescent syndrome. Practical Neurology. 2015 Feb 1;15(1):53-5.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Landau K, Wichmann W, Valavanis A. The missing temporal crescent. American journal of ophthalmology. 1995 Mar 1;119(3):345
- ↑ 8.0 8.1 8.2 8.3 Camacho-Velasquez JL, Rivero-Sanz E, Pérez-Lázaro C, Tejero-Juste C. Temporal crescent syndrome secondary to transient ischaemic attack. Neurologia (Barcelona, Spain). 2019 May;34(4):275-6.
- ↑ 9.0 9.1 9.2 9.3 Pellegrini F, Stafa A, Bonsanto D, Fraser CL. The dark side of the (half) moon. Survey of Ophthalmology. 2020 May 1;65(3):381-5.
- ↑ 10.0 10.1 10.2 10.3 Lepore FE. The preserved temporal crescent: the clinical implications of an “endangered” finding. Neurology. 2001 Nov 27;57(10):1918-21.
- ↑ Benton S, Levy I, Swash M. VISION IN THE TEMPORAL CRESCENT IN OCCIPITAL INFARCTION [Internet]. Vol. 103, Brain. 1980. Available from: https://academic.oup.com/brain/article/103/1/83/271262
- ↑ SmithCG, RichardsonWFG.The course and distribution of the arteries supplying the visual (striate) cortex. Am J Ophthalmol. 1966;61:1391\x=req-\ 1396.