All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Marginal Keratitis - ICD-10 H16.39 (Other Interstitial and Deep Keratitis)
Other names: Staphylococcal Marginal Keratitis; Catarrhal infiltrates.
Disease
Marginal keratitis is an inflammatory disease of the peripheral cornea, characterized by peripheral stromal infiltrates which are often associated with epithelium break down and ulceration. It is usually associated with the presence of blepharoconjunctivitis and is thought to represent an inflammatory response against S. aureus antigens.[1]
Etiology and pathophisiology
The vast majority of patients with marginal keratitis have symptomatic Staphylococcal blepharitis/conjunctivitis, or asymptomatic Staphylococcal colonization of the eyelid.[1]
Marginal keratitis is thought to be the product of an inflammatory reaction against staphylococcal antigens (rather than a direct staphylococcal infection of the cornea). The presence of bacterial antigens in the peripheral area of the cornea possibly triggers a type III hypersensitivity reaction, in which immunocomplexes are formed and deposited in the peripheral corneal stroma.[2] There are subsequent complement pathway activation and neutrophil attraction, with the formation of a peripheral stromal opacity also called catarrhal infiltrate. This lesion may evolve with epithelial damage, forming a marginal ulcer.
The lesions usually appear in areas of direct contact between the peripheral cornea and the eyelid margin, which substantiates the relationship between the keratitis and S. aureus colonization.[1]
Besides the spatial relationship, it is hypothesized that marginal keratitis is the product of anatomical and chemical variations between the central and peripheral cornea. The distance between the central cornea and limbal blood vessels slows down the diffusion of high molecular weight proteins, like IgM and C1 protein, which occur at higher concentrations in the peripheral cornea. The peripheral cornea also has a higher concentration of Langerhans Cells. Therefore, it has been hypothesized that a circular zone of the cornea that is 1 to 2 mm from the limbus may have an antigen-to-antibody ratio that is conducive to larger, more inflammogenic immune complexes. The distance between the central cornea and limbus also means a reduced contact between central cornea antigens and the afferent arm of the immune system, which may protect the central cornea from immune-mediated injury.[3]
Risk Factors and Primary Prevention
The major risk factor is the presence of longstanding blepharitis, conjunctivitis, or meibomitis. In the vast majority of cases, the presence of catarrhal infiltrates is associated with Staphylococcal blepharoconjunctivitis although other microorganisms have been previously isolated from the eyelid of marginal keratitis patients, such as Haemophilus, Moraxella or Streptococcus.[4]
Management of the underlying cause, i.e. blepharitis, is the main form of prevention of marginal keratitis.
Diagnosis
The diagnosis of marginal keratitis is usually based on patient history and slit-lamp examination findings. Ancillary testing can be useful, especially in atypical cases or in cases with peripheral ulceration, in which other diagnoses need to be ruled out.[1]
Symptoms
Patients with marginal keratitis present with mild, nonspecific symptoms like pain, foreign body sensation, photophobia, and conjunctival injection.
Physical examination
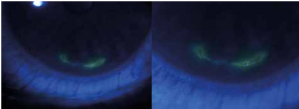
The disease usually begins with the formation of one or more stromal infiltrates in the peripheral cornea, typically in the points of intersection between the eyelid margin and the limbus (i.e. 2, 4, 8, and 10 o’clock positions). These infiltrates are almost always located 1-2mm parallel to the limbus, with a clear margin of healthy cornea between them. The lesions can spread and coalesce circumferentially, with little tendency to grow centrally or peripherally. With prolonged inflammation, there can be an epithelial lesion, leading to the formation of a marginal ulcer.[1][3]
Since the majority of cases are related to symptomatic blepharoconjunctivitis, its distinctive features can also be observed. Erythema and edema of the eyelid margin associated with telangiectasias are common findings in all forms of blepharitis. Eyelash changes like madarosis, poliosis, trichiasis, and the presence of hard scales in the base of eyelashes, are more specific findings of the long-standing S. aureus blepharitis. In more severe cases, the removal of these scales from the eyelid margin can cause ulceration.[5]
Diagnostic procedures
No diagnostic procedures are necessary in typical cases (peripheral stromal infiltrates, with a 1-2mm clear cornea peripheral margin, associated with blepharitis). In cases where an epithelial defect is also present, it is important to distinguish it from other forms of ulceration (mainly infectious ulceration), for which corneal scrape cultures may be useful.[1]
Differential diagnosis
The differential diagnosis of marginal keratitis is broad, encompassing all causes of peripheral stromal keratitis, and peripheral ulcerative keratitis. It is especially important to distinguish this entity from bacterial corneal ulcers which are more central and tend to progress centrally and/or peripherally.
Herpetic stromal keratitis can be indistinguishable from marginal keratitis, but the evolution of both lesions is very different: while herpetic keratitis starts out with an epithelial defect which evolves into a stromal lesion, the opposite happens in marginal keratitis. Herpetic keratitis is also associated with corneal hypoesthesia, contrary to the catarrhal infiltrates.
Peripheral ulcerative keratitis associated with collagen-vascular disorders can mimic marginal keratitis, although it is frequently associated with scleritis and tends to be more severe and less responsive to topical steroids.
Mooren ulcer is a form of idiopathic peripheral ulcerative keratitis, which can be very similar to marginal keratitis. This form of keratitis does not spare the limbal margin and can be more aggressive compared to marginal keratitis.
Management
The primary goal of treatment is to reduce local inflammation and reduce the risk of future flares by reducing staphylococcal antigens at the eyelid margins and corneal surface.
Medical therapy
Topical corticosteroids are the mainstay of treatment directed to the local inflammation, especially in cases of peripheral stromal infiltrates without epithelial defects. In those cases where an epithelial defect is present, steroids should be used judiciously, combined with a broad-spectrum antibiotic, and with close monitoring.
Treatment directed toward blepharitis should also be prescribed: recommendation of adequate eyelid hygiene, topical antibiotic ointments, oral antibiotics if necessary (doxycycline, tetracyclines, or azithromycin) and short courses of topical steroids can be useful to control underlying blepharitis.
Surgery
There is no surgical treatment available targeting the primary disease.
Prognosis
The natural course of the disease is spontaneous resolution in two to three weeks, with few to no long-term sequelae such as anterior stromal scarring. Recurrences are common, especially if the concomitant blepharitis is not treated.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Mannis M., Holland E.: Cornea. Elsevier Health Sciences. 2016; 1079-1081.
- ↑ Smolin G. Hypersensitivity reactions. In: Smolin G, editor. Ocular immunology. 2nd ed. Boston: Little, Brown; 1986
- ↑ 3.0 3.1 Mondino BJ. Inflammatory disease of the peripheral cornea. Ophthalmology 1988;95:463–72.
- ↑ Cohn H, Mondino BJ, Brown SI, et al. Marginal corneal ulcers with acute beta streptococcal conjunctivitis and chronic dacryocystitis. Am J Ophthalmol 1979;87:541–3.
- ↑ McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology 1982;89:1173.