Lipid Keratopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Corneal degenerations typically feature the deposition of material, thinning of tissue, and neovascularization.
Primary lipid keratopathy (LK) is infrequent and occurs spontaneously as stromal deposits of cholesterol and phospholipids. Primary LK is not associated with elevated serum lipids levels.
The secondary form is associated with previous ocular injury or pathology.
Unlike the primary form, secondary LK is far more common and is characteristically associated with corneal neovascularization. This article focus mainly on the primary form of this entity.
Disease Entity
ICD-10: H18.49 - Other corneal degeneration.
Disease
LK is a term applied to conditions where lipid degeneration of the cornea occurs. There are only a few cases of primary LK published to date.
Etiology
LK is supposedly a degenerative disorder with a non-hereditary pattern of occurrence. The accumulation of lipids may result from excessive production, impaired lipid metabolization or both mechanisms.
Risk Factors
Corneal lipid deposition may occur secondary to systemic disorders of lipid metabolism (Fish-eye disease, Tangier disease or familial lipoprotein deficiencies). The secondary form is also associated with previous ocular diseases or injury. Herpetic corneal infections are the most frequent pathologies underlying secondary LK. Although rare, it has been reported following corneal edema, as in hydrops or surgical trauma, such as Intacs implantation.
General Pathology
Histological evaluation shows that the keratopathy material consists of intra- and extracellular lipids. Histochemical staining (Oil red 0 and Sudan black B) indicate deposits of neutral fats and phospholipids.
Diagnosis
Diagnosis of primary lipid degeneration is based on the presence of lipid deposits in the cornea with no prior vascularization, traumatic or inflammatory change.
Physical examination
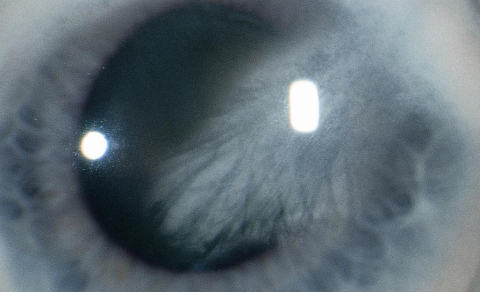
Primary LK may be peripheral, central, or diffuse. The disease is usually bilateral, and the central lipid, often with cholesterol crystals, may severely decrease visual acuity. Secondary LK features are dependent on the underlying cause but frequently one can find a characteristic dense yellow-white infiltrate associated with the presence of an adjacent corneal blood vessel.
Symptoms
Patients complaint of progressive reduction of visual acuity due to opacification of the cornea.
Differential diagnosis
The differential diagnosis should include corneal arcus. LK is frequently denser than arcus and may appear as a circular deposit adjacent to blood vessels. Schnyder corneal dystrophy and other corneal diseases with deposits such as cystinosis, tyrosinemia, hyperuricemia, multiple myeloma, monoclonal gammopathy and infectious crystalline keratopathy should also be considered. Depositions from drugs such as gold, chlorpromazine, chloroquine, and clofazimine might also result in corneal deposition.
Management
In secondary LK treatment, should focus on the underlying disease. Abnormal vascularization may be eliminated by argon laser photocoagulation or needle point cautery to induce the absorption of the lipids through the destruction of the feeder vessels. Intrastromal anti-VEGF agents may be an effective therapeutic option for the management of corneal neovascularization.
Surgery
Although primary LK is extremely rare, penetrating keratoplasty is the preferred approach. Graft outcomes appear to be favorable, possibly because of lack of neovascularization. In secondary LK, corneal grafting remains an option, but it needs a relative quiescence, and the clinical outcome is rather poor because of the corneal thinning, hypoesthesia, and sustained vascularization.
References
- ↑ American Academy of Ophthalmology. Lipid keratopathy. https://www.aao.org/image/lipid-keratopathy-2 Accessed June 28, 2019.
- Araújo AS, Borges JS: Primary lipid keratopathy: a morphological and biochemical assessment. British Journal of Ophthalmology 1993; 77: 248-250
- Babizhayev, M. A., et al. (2014). Studies on the Cornea and Lens, Springer New York.
- Cogan DG, and Kuwabara T: Lipid keratopathy and atheromas. Circulation 1958; 18: pp. 519-525
- Croxatto JO, Dodds CM, and Dodds R: Bilateral and massive lipoidal infiltrates of the cornea (secondary lipoidal degeneration). Ophthalmology 1985; 92: pp. 1686-1690
- Duran JA, and Rodriguez-Ares MT: Idiopathic lipid corneal degeneration. Cornea 1991; 10: pp. 166-169
- Mannis, M. J. and E. J. Holland (2016). Cornea E-Book, Elsevier Health Sciences.
- Shapiro LA, and Farkas TG: Lipid keratopathy following corneal hydrops. Arch Ophthalmol 1977; 95: pp. 456-458