Laser Suture Lysis Post Trabeculectomy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Trabeculectomy has evolved notably since its conception by Cairns in 1968.[1] The long term trabeculectomy survival rate was approximately 60% with no topical medication and approximately 90% with additional topical medication.[2] With the advent of adjuvants, like mitomycin C (MMC), or 5-fluorouracil (5FU), along with the increased surgical success rates, there seemed to be a significant increase in the incidence of postoperative hypotony and its associated complications.[3][4] This led to a conscious effort to ensure a more secure scleral closure in conjunction with the use of either intraoperative releasable sutures or postoperative laser suture lysis (LSL).
LSL, originally described by Lieberman, Hoskins, and Migliazzo, is a procedure that involves the use of compression contact lens in-order to lyse fixed scleral flap sutures, in the postoperative period, pro re nata.[5][6] The titration of postoperative aqueous flow helps in achieving the set target intraocular pressure (IOP).
Principle
The technique involves the use of Laser energy generated by the transconjunctival application of laser, to lyse the suture, thus breaking it. This releases the appositional pressure at the level of scleral flap and helps in a better egress of aqueous into the subconjunctival space.
Indications
This innocuous technique gives the surgeon the liberty to secure the scleral flap with tight sutures intra-operatively, without any onus. LSL should be considered in the following conditions:
- Uncontrolled IOP post-trabeculectomy, despite digital ocular massage
- Low bleb, non-filtering or failing bleb
Contraindications
There are no absolute contraindications for the procedure. However, it would be preferable to avoid the procedure in the following conditions:
- Thick, inflamed tenon’s capsule
- Subconjunctival hemorrhage over the trabeculectomy site
- Fluorescein stained conjunctiva – risk of conjunctival perforation as fluorescein limits argon laser transmission hence concentrating the energy on conjunctiva risking a burn/perforation
Lenses used
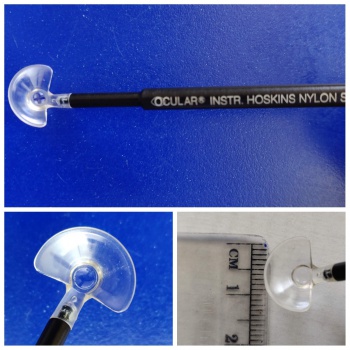
Several different lenses have been used for this procedure, right from four mirror gonioscopy lens as described by Lieberman and the Hoskins suture lysis lens devised by Hoskins and Migliazzo.
Elementally all the lenses serve the same purpose. They not only prevent eye blinking, but also help in applying gentle pressure and blanching the underlying conjunctiva, thus providing good visualization of the small nylon sutures. The lenses used are summarized in Table 1
| Table 1 | Summary of the lenses used for Laser suture lysis (LSL) [7] |
|---|---|
| Hoskins lens – the most commonly used lens(Figure 1) |
|
| Blumenthal lens (Figure 2) |
|
| Ritch lens |
|
| Layden lens |
|
| Mandelkorn lens |
|
| Wells LS |
|
| Edge of Zeiss 4 mirror gonioscopy lens |
Timing
It is preferable to delay suture lysis until 48 hours postoperatively, as an early procedure could risk excessive filtration and ocular hypotony.[8] Hoskins and Migliazzo first described effective LSL when done 1-3 weeks postoperatively. [5] [6] So, prior to the use of adjuvants the acceptable window for LSL in order to achieve a favorable outcome was within the first 2 weeks (day 4 to 3 weeks window period) postoperatively. However, the intraoperative use of MMC was noted to delay wound healing considerably, thus allowing for an extended “window period” to perform LSL. Some studies noted that a delayed LSL could be effective beyond 2 weeks.[9][10]
However, in a recent study by Mano et. al, they have highlighted the efficacy of an earlier LSL from 8th day to 12th-week post trabeculectomy for any IOP reading of >10 mm Hg and observed an effective IOP reduction, more so, following the 1st LSL, without any subsequent increase in the complication rate.[11]
Laser types and settings
Types of Lasers:
Argon laser (514nm) is the most common laser used for laser suture lysis, universally.
However, the other lasers that have been used for this purpose include:
- Nd: YAG (1064 nm or 532 nm frequency-doubled)[12]
- Diode laser (840 nm) originally described by Lieberman
- Krypton (647 nm) and
- Yellow Pascal(577 nm)
Laser parameters for LSL:
Table 2 summarizes the laser parameters for LSL[12][13]
| Table 2 | Laser parameters for laser suture lysis |
|---|---|
| Energy | 250-1000 mW/ 2-2.5mJ/ 300-400mV |
| Spot size | 50-100 microns |
| Duration | 20-100 mSec |
| Applications | 1-3 |
Procedure
- Instill a drop of topical anesthetic (Proparacaine 0.5%), and carefully assess the trabeculectomy site.
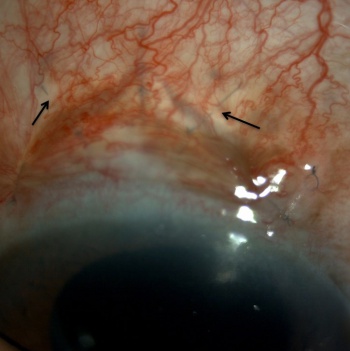
- If the overlying conjunctiva is injected, a drop of 2.5% phenylephrine can be used to cause vasoconstriction, thus allowing an optimum visualization of the underlying scleral sutures.
- Ask the patient to look down and with the help of an assistant gently lift the upper lid for better access and visualization.
- Place the lysis lens directly over the scleral sutures, compressing the conjunctiva onto the scleral surface and deliver the laser energy. The compression causes deturgescence and blanching of the conjunctiva allowing a clear visualization of the suture to be lysed. (Figure 2 & 3)
- Care must be taken to cut one suture at a time.
- The suture closest to the limbus should be lysed first, followed lastly by the distal sutures, as cutting these could lead to larger blebs and hypotony.
- Once lysed (Figure 4), the site should be reassessed to look for spontaneous bleb formation.
- If the outcome is inadequate, ocular massage can be done with the same lens.
In circumstances where the patient is relatively uncooperative, or in case of an inadequate surgical skill, Kratz et al, described a novel technique of using a multi-spot laser system. This involves the creation of a “laser line” of 250 microns length, composed of 5 conjoined laser spots, each of 50-micrometer diameter, 400 mW power, 10 mSec in duration, using a green laser (532 nm).[14]
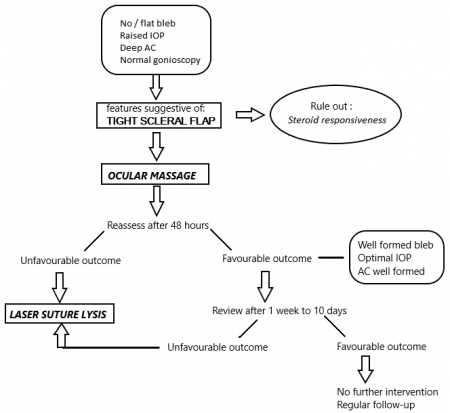
Figure 5 describes the algorithm suggested by authors for early postoperative management with LSL.
Complications
The incidence of complications post LSL is observed to be around 30%.[13] Based on the time of occurrence of these complications, they are classified into immediate, early and late as summarized in the tables below. [13][15]
Immediate complications:
| Table 3 | Immediate post LSL complications |
|---|---|
| Wound dehiscence |
|
| Conjunctival perforation |
|
Early complications:
| Table 4 | Early post LSL complications |
|---|---|
| Hypotony |
|
| Shallow or flat AC |
|
| External aqueous leaks |
|
| Iris incarceration |
|
| Hyphema |
|
| Malignant glaucoma |
|
Late complications:
| Table 5 | Late post LSL complications |
|---|---|
| Progressive lenticular opacity |
|
| Large filtering blebs |
|
Summary
Laser suture lysis constitutes an integral part of early postoperative management of ineffective aqueous drainage due to tight scleral closure. The fundamental procedure has remained simple despite some minor variations in laser systems and techniques. LSL gives the surgeon the liberty to tip his scale towards securing the scleral flap more tightly, thus avoiding the risk of hypotony and its associated complications. In addition to this, the adequacy of an office setting adds to its advantage. LSL can be done anytime between 4th day to 3 weeks postoperatively, with a liberty of delayed-release in trabeculectomy surgeries enhanced with antimetabolites. Though a simple procedure, the presence of hemorrhage or chemosis or fibrosed tenon’s capsule could make it difficult. Furthermore, it should be kept in mind that it is preferable to do sequential lysis, in-order to lower IOP gradually to the desired range. In conclusion, LSL is a simple office procedure to manage early postoperative increase in IOP risking bleb failure and should be considered a fairly good option not requiring any additional surgical skill.
References:
- ↑ Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66(4):673–679.
- ↑ Landers J, Martin K, Sarkies N, Bourne R, Watson P. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology. 2012;119(4):694–702. doi:10.1016/j.ophtha.2011.09.043
- ↑ Costa VP, Wilson RP, Moster MR, Schmidt CM, Gandham S. Hypotony maculopathy following the use of topical mitomycin C in glaucoma filtration surgery. Ophthalmic Surg. 1993;24(6):389–394.
- ↑ Stamper RL, McMenemy MG, Lieberman MF. Hypotonous maculopathy after trabeculectomy with subconjunctival 5-fluorouracil. Am J Ophthalmol. 1992;114(5):544–553. doi:10.1016/s0002-9394(14)74481-2
- ↑ 5.0 5.1 Lieberman MF. Suture lysis by laser and goniolens. Am Y Ophthalmol 1983; 95: 257-8.
- ↑ 6.0 6.1 Hoskins HD, Migliazzo C. Management of failing filtering blebs with the argon laser. Ophthalmic Surg 1984; 15: 731-3.
- ↑ Aditi Singh, Meena Menon. Lenses in Glaucoma. Delhi journal of ophthalmology 2018; 28:55-57
- ↑ Melamed S, AshkenaziI, Glovinski J, Blumenthal M. Tight scleral flap trabeculectomy with postoperative laser suture lysis. Am J Ophthalmol. 1990;109(3):303–309. doi:10.1016/s0002-9394(14)74555-6
- ↑ Pappa KS, Derick RJ, Weber PA, Kapetansky FM, Baker ND, Lehmann DM. Late argon laser suture lysis after mitomycin C trabeculectomy. Ophthalmology. 1993;100(8):1268–1271. doi:10.1016/s0161-6420(93)31494-6
- ↑ Ramakrishna S, Nelivigi S, Sadananda AM, Ganesh S. Study of efficacy and timing of laser suture lysis in reducing intraocular pressure after trabeculectomy with mitomycin-C. Oman J Ophthalmol. 2016;9(3):144–149. doi:10.4103/0974-620X.192264
- ↑ Mano SS, Esteves RM, Ferreira NP, Abegão Pinto L. A standardized protocol of laser suture lysis in postoperative management in trabeculectomy with mitomycin C: One-year study [published online ahead of print, 2020 Jan 27]. Eur J Ophthalmol. 2020;1120672120901699. doi:10.1177/1120672120901699
- ↑ 12.0 12.1 Shah, Syed Shah, Shujaat Rai, Partab Siddiqui, Shahid Abbasi, Safdar Shaikh, Dure. Role of Laser suture lysis in Immediate Trabeculectomy Failure. Pakistan Journal of Ophthalmology. Pak J Ophthalmol 2015
- ↑ 13.0 13.1 13.2 Macken P, Buys Y, Trope GE. Glaucoma laser suture lysis. Br J Ophthalmol. 1996;80(5):398–401. doi:10.1136/bjo.80.5.398
- ↑ Kratz A, Goldberg I, Levy J, Knyazer B, Lifshitz T. A Novel Method for Laser Suture Lysis Using Multispot Laser System. J Glaucoma. 2017;26(4):e163–e164. doi:10.1097/IJG.0000000000000570
- ↑ 15.0 15.1 15.2 15.3 Savage JA, Condon GP, Lytle RA, Simmons RJ. Laser suture lysis after trabeculectomy. Ophthalmology. 1988;95(12):1631–1638. doi:10.1016/s0161-6420(88)32964-7
- ↑ Bardak Y, Cuypers MH, Tilanus MA, Eggink CA. Ocular hypotony after laser suture lysis following trabeculectomy with mitomycin C. Int Ophthalmol. 1997;21(6):325–330. doi:10.1023/a:1006024522541
- ↑ Geijssen HC, Greve EL. Mitomycine, suture lysis and hypotony. Int Ophthalmol 1992; 16: 371–4
- ↑ Zacharia PT, Deppermann SR, Schuman JS. Ocular hypotony after trabeculectomy with mitomycin C. Am J Ophthalmol 1993; 116: 314–26
- ↑ Morinelli EN, Sidoti PA, Heuer DK, et al. Laser suture lysis after mitomycin C trabeculectomy. Ophthalmology. 1996;103(2):306–314. doi:10.1016/s0161-6420(96)30699-4