Laser Resurfacing of the Eyelids and Face
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Overview
Laser resurfacing is a facial rejuvenation procedure available to cosmetic surgeons that uses a laser to improve the tone, texture, and pigmentation of the skin. There are a variety of different dermatologic lasers that are currently in use and these lasers can be broadly categorized into two types: ablative and non-ablative lasers. These lasers are used to remove damaged skin layers and allow the growth of new, smoother, evenly toned, and tighter skin. Though it can be used to treat minor facial flaws such as lentigines, rhytides, and a wide variety of scars, it is not a substitute for a facelift or blepharoplasty. The indications, contraindications, mechanism of action, efficacy, adverse effects, and management of these laser treatments will be discussed.
History
Laser resurfacing has evolved tremendously since its first application in the 1980s with advancements in laser technology. This procedure was first performed using continuous wave carbon dioxide (CO2) laser. While effective, use of this ablative laser was associated with adverse effects including erythema, dyspigmentation, infections, and scarring due to significant thermal damage. To reduce such adverse events, subsequent development of pulse CO2 lasers allowed for limited skin heating, which improved the safety of this treatment.[1] In the 1990s, erbium:yttrium-alumninum-garnet (Er:YAG) lasers were developed for skin resurfacing. These lasers had more control over the depth of cutaneous ablation than CO2 lasers due to their shorter wavelength.[2] Though these new developments in laser technology led to improved safety of skin resurfacing treatments, the process of ablating the epidermis still had long recovery times and a small, but significant, risk of adverse events, including erythema, dyspigmentation, infections, and scarring.[1] [3]
Non-ablative laser skin resurfacing technology arose in the 1990s as an alternative to these ablative laser treatments to improve the skin cosmetically with faster recovery times and lower risk of adverse effects. This was attempted via remodeling of the dermis while leaving the epidermis intact. However, these non-ablative laser treatments were quickly shown to be less effective.[4]
In the 2000s, the development of fractional lasers transformed skin resurfacing by drastically improving recovery times for ablative procedures. By emitting numerous narrow, microscopic columns of laser, fractional lasers created microscopic thermal zones interspersed with zones of normal tissue allowing for faster recovery. Both ablative and non-ablative skin resurfacing treatments have now adopted this new technology, but recovery time is unexpectedly not faster for non-ablative fractional lasers. This is because “non-ablative fractional lasers” actually use ablative technology for better outcomes, but are still considered “non-ablative” as they attempt to preserve the epidermis with cooling techniques.[5]
Ablative Laser Skin Resurfacing
Indications
Indications for ablative laser resurfacing include the following:[6] [7]
- Photoaging
- Facial wrinkles
- Acne scars
- Surgical or traumatic scars
- Actinic keratoses
- Seborrheic keratoses
- Warts
- Moles and other nevi
- Xanthelasma
- Skin tags
- Rhinophyma
- Sebaceous hyperplasia
- Pyogenic granuloma
- Neurofibroma
- Angiofibroma
- Actinic cheilitis
- Keloids
Contraindications
Possible contraindications for ablative laser resurfacing include the following:[6][7]
- Fitzpatrick skin types IV-VI
- History of keloidal scarring
- Recent oral isotretinoin therapy
- Ectropion
- Morphea
- Scleroderma
- Prior radiation therapy
- Cutaneous disorders
- Active herpes outbreaks or other ongoing infections in the targeted area
- Ongoing ultraviolet exposure
- Recent chemical peel
- Pregnancy
Types
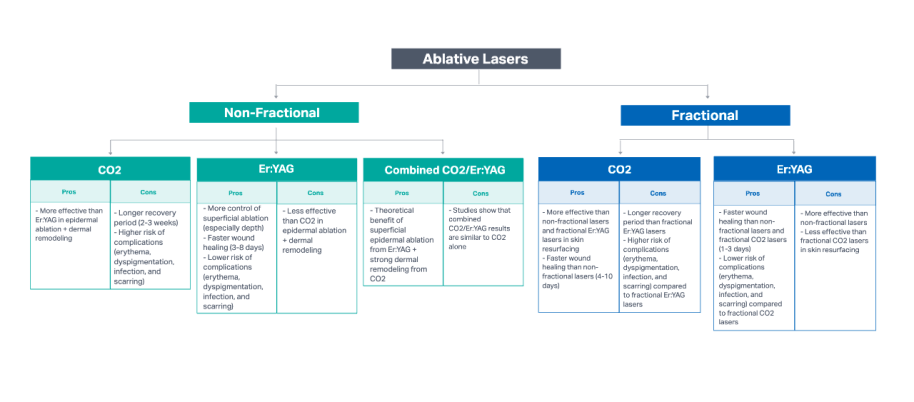
Ablative laser skin resurfacing can be further divided by the type of laser used: non-fractional or fractional lasers (See Figure 1).
Non-Fractional Ablative Lasers
Mechanism of Action
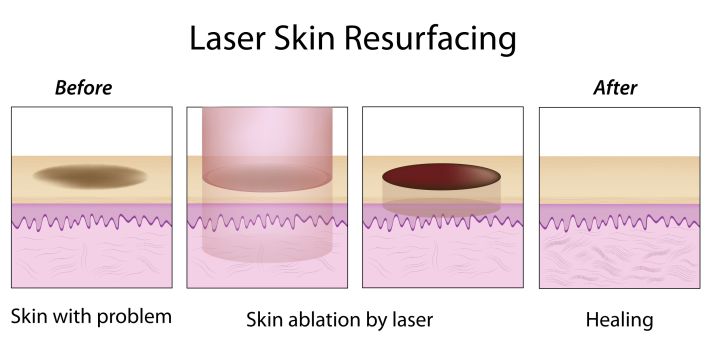
In ablative skin resurfacing using non-fractional lasers, the epidermal layer is removed by projecting a laser on the entire surface of the treated skin. The light emitted by the non-fractional laser is absorbed by the water in the epidermis. When these water molecules superheat and turn into gas, the epidermal layer is subsequently vaporized.[8][9] This thermal damage extends beyond depth at which the light penetrates. The heat transferred to the underlying dermal layer promotes collagen formation and remodeling, leading to retraction of the dermis and epidermis and observed skin tightening.[8][10][11][12]
Types
Non-fractional ablative lasers can be further distinguished by the type of laser used: CO2, Er:YAG, or combined CO2/Er:YAG lasers.
CO2 Lasers
CO2 lasers were the first lasers developed for skin resurfacing. Today, there are two main types of CO2 lasers used for non-fractional ablative skin resurfacing: high-power pulsed CO2 laser and scanning of continuous wave CO2 laser. Studies have shown that pulsed CO2 lasers and scanning CO2 lasers produce equivalent resurfacing results with similar side effects and histology.[13]
Examples of commercially available CO2 lasers include Matrix LS-40 (Sandstone Medical Technologies, Birmingham AL) and UltraPulse (Lumenis, Israel).
Er:YAG Lasers
Er:YAG lasers were the next lasers developed for skin resurfacing. Er:YAG lasers provide more depth control of cutaneous ablation due to shorter wavelength, which allows water molecules to absorb light emitted from Er:YAG lasers at 10 to 16 times greater than the light emitted from CO2 lasers.[14] This greater affinity for light by water in the epidermis decreases the penetration depth of Er:YAG lasers, thereby leading to more precise ablation of the epidermal layer with less damage to surrounding tissues.8 9 Studies show that CO2 lasers may be slightly superior to Er:YAG lasers due to better collagen remodeling associated with CO2 lasers.[15] However, Er:YAG lasers are associated with less severe side effects due to more depth control and less heat injury.[16]
Examples of commercially available Er:YAG lasers include Focus Medical NaturaLase ER (Focus Medical, Bethel CT), Quantel Derma GmbH BURAINE (Quantel, France) and SmoothPeel (Candela, Wayland MA).
Combined CO2/Er:YAG
Doctors have attempted to synergize the effects of both CO2 and Er:YAG lasers by combining the increased depth of CO2 lasers with the theoretically improved control of Er:YAG lasers to preserve the epithelium.[17] However, studies show that combined CO2/Er:YAG laser treatment show similar efficacy to CO2 laser treatment alone.[18]
Examples of a commercially available combined CO2/Er:YAG laser include the Cortex Resurfacing Work Station (Sandstone Medical Technologies, Birmingham AL).
Fractional Ablative Laser
Mechanism of Action
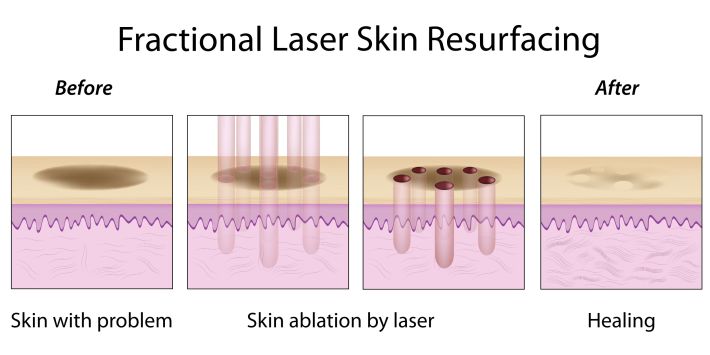
The mechanism of action of ablating the epidermal layer is similar in both fractional and non-fractional ablative laser skin resurfacing. Water molecules absorb light emitted by the laser and superheat. As water molecules transform into gas, the epidermal layer is subsequently vaporized.[8][9] Thermal damage from vaporization promotes collagen formation and remodeling within the dermal layer, leading to retraction of the dermis and epidermis and observed skin tightening. Fractional ablative lasers differ from non-fractional ablative lasers in how the laser is emitted onto the skin (See Figure 2 and 3).[8][10][11][12] In fractional ablative laser skin resurfacing, numerous narrow, microscopic columns of lasers are emitted thereby creating many microscopic thermal zones interspersed with zones of normal tissue. The undamaged surrounding skin adjacent to these microscopic thermal zones function as a reservoir of viable tissue, allowing for rapid re-epithelization during the healing process and quicker recovery period. In non-fractional ablative lasers, healing is dependent on migration of epithelial cells from nearby untreated skin.[5][19]
Efficacy
Similar to non-fractional ablative lasers, fractional ablative lasers can be emitted as both CO2 lasers and Er:YAG lasers. Fractional technology was first developed for CO2 lasers and subsequently developed for Er:YAG lasers.[8] The advantages and disadvantages of fractional CO2 lasers compared to fractional Er:YAG lasers are similar to those of non-fractional ablative lasers. Fractional Er:YAG lasers are associated with less post-operative complications due to its shorter wavelength and consequent less residual thermal damage.[20] Moreover, fractional ablative lasers have been shown to be as effective or more effective than non-fractional ablative laser resurfacing treatments with lower risk of adverse effects.[19][21] As a result, fractional ablative lasers have now become the preferred method of laser resurfacing treatment.
Examples of commercially available CO2 fractional, ablative lasers include the Harmony Platform Pixel CO2 (Alma, Israel), Slim Evolution II MiXto Pro (Lasering USA, San Ramon CA), and eCO2 (Lutronic, South Korea)
Examples of commercially available Er:YAG fractional, ablative lasers include the 2940 DualMode (Industra Technologies, Brazil) and ProFractional XC (Sciton, Palo Alto CA).
Complications of Ablative Lasers
Complications of ablative laser skin resurfacing, whether non-fractional or fractional, include persistent erythema, dyspigmentation, infections, and scarring. However, the complications for fractionated are much rarer and shorter in duration when they do occur.[22]
Erythema due to non-fractional ablative laser skin resurfacing normally lasts about one month after Er:YAG laser treatment and about two months after CO2 laser treatment. However, this erythema may persist for up to one year with non-fractional CO2 laser treatment.[2][23]
Dyspigmentation, both hyperpigmentation and hypopigmentation, is possible with ablative laser skin resurfacing. Studies have shown that patients may experience transient hyperpigmentation that can last up to three months and transient hypopigmentation that can last up to one year. In some cases, patients may have permanent dyspigmentation. Of note, patients with darker skin tone are at higher risk of dyspigmentation. Therefore, it is important to be more cautious when utilizing ablative lasers on darker skin.[1][8][24][25] CO2 laser treatment has been associated with more discoloration.[3]
Viral, bacterial, and candida infection may occur after ablative laser skin resurfacing. Clinical signs of infection include pain with deterioration in skin appearance with or without exudates. Of note, ablative skin resurfacing may reactivate herpes simplex virus (HSV) and precautions should be taken.[26] Moreover, the skin barrier may be compromised after non-fractional ablative laser skin resurfacing in the treated area and increase susceptibility to contact dermatitis.[27]
Scarring is a feared cosmetic complication of non-fractional ablative laser skin resurfacing. The risk of scarring is greater when performing laser resurfacing treatments outside the face.28 Though both CO2 and Er:YAG lasers can cause scarring, the risk for scarring is greatest with CO2 lasers because of its greater residual thermal damage.[13][15][16] In fact, due to its high risk for scarring, use of non-fractionated CO2 lasers is discouraged in laser resurfacing treatments outside the face.[28]
Management
Pre-Operative
Prior to initiating non-fractional or fractional ablative laser resurfacing treatment, patients must be properly informed of the risks and expectations of the procedure. Also, it is important to assess the patient for any contraindications to this therapy [See Section 2.2, Contraindications]. Patients should also be aware of the risks of hypopigmentation and hyperpigmentation.
As ablative laser resurfacing treatment may reactivate HSV, in patients with a prior positive history, oral antiviral prophylaxis is recommended to prevent reactivation of HSV. Typically, acyclovir 200mg BID, valacyclovir 500mg BID, or famciclovir 500mg BID is given one day before treatment and continued until re-epithelization is complete.[26]
Prophylactic antibiotic use for bacterial infections is still debated with some studies recommending its use and others demonstrating no real indication for its use.[29][30] As of now, prophylactic antibiotic use is limited to patients who are perceived to be at high risk for infection, such as immunocompromised patients.
Pretreatment with topical tretinoin is commonly recommended by cosmetic surgeons to improve healing time. However, there is currently insufficient data and further studies are needed to establish its role.[31][32]
Intra-Operative
Ablative laser resurfacing treatment is painful. The patient will feel more pain the deeper the laser resurfacing procedure goes. For superficial resurfacing procedures, topical anesthesia usually suffices. However, local anesthesia and/or nerve blocks, as well as sedation, may be used as needed.[33] For full face treatments, patients normally require light sedation.[34]
In non-fractional ablative laser resurfacing treatments, more than one laser pass is often performed during a single session to achieve cosmetic satisfaction. The effacement of the skin deformity (rhytides, lentigines, etc.) indicates treatment endpoint. However, treatment should be stopped immediately when brown or yellow color is noted on wiping away vaporized tissue as this may indicate tissue necrosis.[35] Moreover, since treatment causes significant color contrast between treated and untreated skin, it is recommended that a treatment incorporate an entire cosmetic unit and to consider lower power settings near the edges to taper the color contrast if the full face is not treated.
In fractional ablative laser resurfacing treatments, the density of microscopic thermal zones may increase the depth of ablation and may lead to increased risk of adverse effects.[36] Therefore, it is recommended to reduce the density of microscopic thermal zones when using fractional ablative lasers in areas associated with greater risk for complications such as the neck and periocular skin.[19] Moreover, like non-fractional ablative laser treatments, since treatment causes significant color contrast between treated and untreated skin, it is recommended that fractional ablative laser resurfacing treatment incorporate an entire cosmetic unit and to consider lower power settings near the edges to taper the color contrast if the full face is not treated.
Given the possible damage that ablative lasers can cause, metal shields are used to protect the eyes when ablative therapy is used around the periocular area.
Post-Operative
Post-operative management is vital after non-fractional and fractional ablative laser resurfacing to promote wound healing and reduce erythema, dyspigmentation, infection, and scarring. Management after the procedure includes the use of cool compresses to reduce swelling and saline/water soaks to keep the skin moist. Studies have demonstrated that moisture promotes wound healing, so some providers recommend frequent application of topical ointments, such as petroleum jelly (Aquaphor (Beiersdorf AG, Hamburg Germany) or Vaseline (Unilever, London UK)). However, both open and closed (that is, covered) wound care techniques have shown similar outcomes.[3][35][37] Once the skin is smooth without crusting and oozing, petroleum jelly is discontinued and hypoallergenic moisturizers are used to keep the skin moist for continued wound healing. Edema is expected after treatment and typically subsides after the first few days.[3]
Other complications include erythema and dyspigmentation, which may persist for months. However, it is usually transient and should subside with time. To prevent possible permanent dyspigmentation, patients should engage in proper sun protective practices when going outside in the sunlight. Ideally, patients should avoid sun exposure two weeks prior to and after treatment.[22][38] Moreover, if dyspigmentation occurs, the use of topical hydroquinone cream or retinoids has been shown to accelerate resolution of dyspigmentation.[3][24]
Scarring is another complication for which topical or injectable steroids or non-ablative laser skin resurfacing may be used.[39]
Use of CO2 lasers generally requires a longer recovery period than that of Er:YAG lasers due to the greater residual thermal damage. With non-fractional CO2 lasers, most patients can return to work two to three weeks after full face treatment. With non-fractional Er:YAG lasers, most patients can return to work three to eight days after full face treatment.[6] With fractional CO2 lasers, most patients can return to work four to ten days after treatment. With fractional Er:YAG lasers, most patients can return to work within one to three days after treatment.[6]
Non-Ablative Laser Skin Resurfacing
Indications
Indications for non-ablative laser resurfacing include the following:[40]
- Photoaging
- Dyschromia
- Acne scars
- Surgical and traumatic scars
- Erythema
- Telangiectasias
- Melasma
- Striae distensae
- Mild to moderate rhytides
- Mild to moderate laxity
Contraindications
Possible contraindications for non-ablative laser resurfacing include the following:[40][41]
- Fitzpatrick skin types IV-VI
- History of keloidal scarring
- Recent oral isotretinoin therapy
- Pregnancy
Types
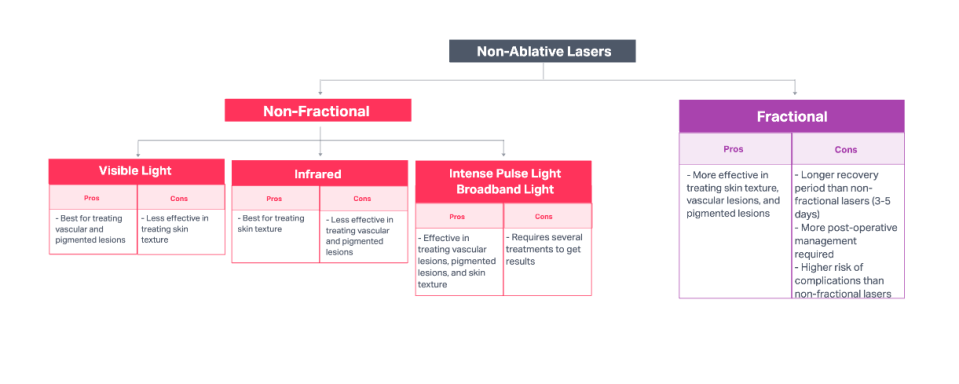
Non-ablative laser skin resurfacing can be further divided by the type of laser used: non-fractional or fractional lasers (Figure 4).
Non-Fractional Non-Ablative Lasers
Mechanism of Action
In non-ablative skin resurfacing using non-fractional lasers, light emitted by the non-fractional laser is absorbed by various molecules or chromophores in the dermal layer, causing selective thermal injury and subsequent new collagen formation and remodeling in the dermis while leaving the epidermis intact.[4] This skin resurfacing treatment is known as “non-ablative,” because the epidermis does not vaporize like in ablative laser resurfacing treatments. The epidermis is protected from most damage through a variety of means, including the use of specific wavelengths that selectively target the dermis or use of cooling techniques to decrease damage to the epidermis.[42] Since non-fractional, non-ablative lasers do not induce significant damage to the epidermis, these skin resurfacing treatments not only have a shorter recovery time, but also have a significantly lower risk of adverse effects compared to ablative lasers. However, these lasers are less efficacious than ablative lasers in treating skin tone, texture, and pigmentation and show only modest improvements.[8][9][35][42]
Types
Non-fractional non-ablative laser skin resurfacing can be performed using a variety of different devices that use lasers at different wavelengths. The types of lasers used in non-fractional non-ablative laser skin resurfacing will be discussed here.
Visible Light Lasers
Using visible light lasers for non-fractional non-ablative laser skin resurfacing is ideal for treating vascular and pigmented lesions, since these lasers emit light at wavelengths that hemoglobin and melanin absorb well. Though improvement in skin texture is often seen with visible light lasers because of residual thermal injury and subsequent fibroblast activity and collagen formation and remodeling, the skin texture improvement is smaller than that seen for vascularity and pigmentation.[4][42][43][44][45][46]
Examples of commercially available visible light lasers include the Harmony XL Pro (Alma, Israel), VBeam (Candela, Wayland MA), and Accolade (Cynosure, Westford MA).
Infrared Lasers
Using infrared lasers (1320-nm Nd:YAG, 1450-nm diode, and 1540-nm erbium-glass) for non-fractional, non-ablative laser skin resurfacing is ideal for treating skin texture, since these lasers emit light at wavelengths that water molecules absorb well thereby heating the dermis. The resulting thermal damage in the dermis promotes new collagen formation and remodeling resulting in improved skin texture. The process of activating fibroblasts and promoting new collagen in non-fractional, non-ablative infrared lasers is similar to that of ablative lasers. Unlike ablative lasers, however, use of infrared lasers in non- fractional non-ablative skin resurfacing utilizes a variety of cooling techniques to protect the epidermis. These include cryogen cooling sprays and contact cooling systems.[4][42][47][48][49][50]
Examples of commercially available infrared lasers include the QYAG5 (Palomar, Carlsbad CA), CT3 Plus (Cooltouch, Roseville CA) and Aramis (Quantel, France).
Intense Pulse Light/Broadband Light
Intense pulse light (IPL) devices for non-fractional, non-ablative laser skin resurfacing use a broad spectrum of light emissions with varying wavelengths to heat up the skin and cause damage to tissue that the body naturally removes and rejuvenates afterwards. Unlike visible light and infrared lasers, IPL can be used to treat skin texture, vascular lesions, and pigmented lesions.[42][51][52]
Examples of commercially available IPL devices include the Icon (Cynosure, Westford MA) and Apex (CPMT, Canada).
Broadband light (BBL) devices for non-fractional, non-ablative laser skin resurfacing work in much the same way as IPL. However, BBL uses higher intensity lights than IPL. IPL is better suited for treating a targeted area whereas BBL is better for treating a broader skin range.
Examples of commercially available BBL devices include the BBL Hero (Sciton, Palo Alto CA)
Fractional, Non-Ablative Lasers
Mechanism of Action
In fractional, non-ablative laser skin resurfacing, infrared lasers emit wavelengths that are absorbed well by water molecules, resulting in thermal damage in the dermis that promotes new collagen formation and remodeling. These lasers are emitted onto the skin in numerous narrow, microscopic columns, creating microscopic thermal zones interspersed with zones of normal tissue. The undamaged skin adjacent to these microscopic thermal zones allow for rapid re-epithelization during the healing process and for a shorter recovery period.[4][8][9] Unlike infrared lasers used in non-fractional, non-ablative skin resurfacing treatments, where a variety of cooling techniques protect the epidermis from damage, these fractional infrared lasers can damage the epidermis leading to possible ablation of the epidermal layer. However, the epidermis can be preserved by utilizing low energy settings. As a result, some fractional laser treatments can be considered non-ablative – hence the name, “fractional, non-ablative.” [8][35][53]
Fractional, non-ablative lasers can be used to improve skin texture and dyspigmentation, including mild to moderate wrinkles, acne scarring, and hyperpigmentation.[4][8][9][53] Unlike other forms of laser skin resurfacing treatment, fractional, non-ablative lasers can also be used to effectively treat regions outside the face, including the neck, chest, and extremities.[54]
Examples of commercially available fractional, non-ablative lasers include Starlux (Palomar, Carlsbad CA), Affirm (Cynosure, Westford MA), and ResurFx (Lumenis, Yokneam Israel).
Complications
Complications after non-ablative laser skin resurfacing therapy are very rare and very self-limiting, but can include erythema, pinpoint hemorrhages, dyspigmentation, blistering, ulcerations, and scarring. Most complications are a result of improper technique or excessive treatment. Regardless, most complications that do occur are transient and subside with time without any permanent damage. Areas of thinner skin and minimal fat such as the periorbital area are more likely to experience complications of pinpoint hemorrhages.[8][40]
Management
Pre-Operative
Prior to initiating non-ablative laser skin resurfacing therapy, patients must be properly informed of the risks and expectations of the procedure. Though complications due to non-ablative laser resurfacing are significantly more rare than ablative laser resurfacing, it is important to warn patients of such possible complications. Moreover, since non-ablative laser resurfacing therapy has modest improvements in skin tone, texture, and pigmentation, it is important to only recommend this therapy to patients, who would see a benefit from the treatment. It is most appropriate for patients with features of photoaging, who want rapid recovery and a low-risk procedure. Of note, it is important to assess the patient for any contraindications to this therapy [See 3.2 Contraindications].[4][40] Though non-ablative resurfacing therapy has been approved for all skin tones, patients with darker skin tone have a higher risk of dyspigmentation and are often recommended to pretreat with 4% hydroquinone daily for 3 to 4 weeks before treatment to minimize dyspigmentation.
Prophylactic antibiotics and antivirals are not routinely indicated for non-ablative laser skin resurfacing, since the epidermis remains intact. However, for fractional, non-ablative skin resurfacing treatments, HSV prophylaxis is recommended to avoid reactivation of HSV.[4][40] A typical dose includes the following: acyclovir 200mg BID, valacyclovir 500mg BID, or famciclovir 500mg BID is given one day before treatment and continued until re-epithelization is complete.[26]
Intra-Operative
Pain associated with non-ablative laser skin resurfacing therapies varies depending on the device used. For most non-fractional, non-ablative therapies using visible light lasers or IPL, anesthesia is not required as there is only mild discomfort for the patient. However, non-ablative therapies using infrared lasers (non-fractional and fractional) are associated with some pain, so topical or local anesthesia is routinely used.[4][33] Moreover, metal shields are used to protect the eyes when fractional, non-ablative therapy is used around the periocular area.
Post-Operative
Unlike ablative laser skin resurfacing therapies, non-ablative therapies do not require specific post-operative measures to promote healing as there are usually no serious complications and the complications that do occur are very self-limiting. For most non-ablative laser therapies, patients can resume normal activity immediately after the treatment. Post-operative erythema, edema, and pain is usually very minimal and resolve within hours; however, this may vary between patients. Cold compresses can be used post-operatively to minimize possible swelling and improve patient comfort.[3][35]
Due to the nature of fractional technology, fractional, non-ablative laser skin resurfacing therapies have slightly longer recovery periods than other non-ablative laser therapies and may require some post-operative measures. Post-operative erythema and edema can last up to three days in these patients. Moreover, patients may also apply non-irritating emollients that maintain skin moisture and promote healing.[4][35][40][54]
Moreover, since sun exposure increases the risk for post-inflammatory hyperpigmentation, patients should engage in proper sun protective practices to prevent complications of dyspigmentation.[3][4][24]
References
- ↑ Jump up to: 1.0 1.1 1.2 Ross EV, Grossman MC, Duke D, Grevelink JM. Long-term results after CO2 laser skin resurfacing: a comparison of scanned and pulsed systems. J Am Acad Dermatol. 1997;37(5 Pt 1):709-718. doi:10.1016/s0190-9622(97)70106-3
- ↑ Jump up to: 2.0 2.1 Perez MI, Bank DE, Silvers D. Skin resurfacing of the face with the Erbium:YAG laser. Dermatol Surg. 1998;24(6):653-659. doi:10.1111/j.1524-4725.1998.tb04223.x
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Alster TS, Lupton JR. Erbium:YAG cutaneous laser resurfacing. Dermatol Clin. 2001;19(3):453-466. doi:10.1016/s0733-8635(05)70286-2
- ↑ Jump up to: 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Khattar, Maria. (2016). Nonablative Lasers for Photorejuvenation. 10.1007/978-3-319-20251-8_5-1.
- ↑ Jump up to: 5.0 5.1 Hantash BM, Bedi VP, Chan KF, Zachary CB. Ex vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39(2):87-95. doi:10.1002/lsm.20405
- ↑ Jump up to: 6.0 6.1 6.2 6.3 Verma N, Yumeen S, Raggio BS. Ablative Laser Resurfacing. In: StatPearls. Treasure Island (FL): StatPearls Publishing; November 18, 2021.
- ↑ Jump up to: 7.0 7.1 Krupa Shankar D, Chakravarthi M, Shilpakar R. Carbon dioxide laser guidelines. J Cutan Aesthet Surg. 2009;2(2):72-80. doi:10.4103/0974-2077.58519
- ↑ Jump up to: 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Preissig J, Hamilton K, Markus R. Current Laser Resurfacing Technologies: A Review that Delves Beneath the Surface. Semin Plast Surg. 2012;26(3):109-116. doi:10.1055/s-0032-1329413
- ↑ Jump up to: 9.0 9.1 9.2 9.3 9.4 Brightman LA, Brauer JA, Anolik R, et al. Ablative and fractional ablative lasers. Dermatol Clin. 2009;27(4):479-vii. doi:10.1016/j.det.2009.08.009
- ↑ Jump up to: 10.0 10.1 Ross EV, McKinlay JR, Anderson RR. Why does carbon dioxide resurfacing work? A review. Arch Dermatol. 1999;135(4):444-454. doi:10.1001/archderm.135.4.444
- ↑ Jump up to: 11.0 11.1 Fulton JE Jr, Barnes T. Collagen shrinkage (selective dermaplasty) with the high-energy pulsed carbon dioxide laser. Dermatol Surg. 1998;24(1):37-41. doi:10.1111/j.1524-4725.1998.tb04049.x
- ↑ Jump up to: 12.0 12.1 Walia S, Alster TS. Prolonged clinical and histologic effects from CO2 laser resurfacing of atrophic acne scars. Dermatol Surg. 1999;25(12):926-930. doi:10.1046/j.1524-4725.1999.99115.x
- ↑ Jump up to: 13.0 13.1 Alster TS, Nanni CA, Williams CM. Comparison of four carbon dioxide resurfacing lasers. A clinical and histopathologic evaluation. Dermatol Surg. 1999;25(3):153-159. doi:10.1046/j.1524-4725.1999.08126.x
- ↑ Kaufmann R, Hartmann A, Hibst R. Cutting and skin-ablative properties of pulsed mid-infrared laser surgery. J Dermatol Surg Oncol. 1994;20(2):112-118. doi:10.1111/j.1524-4725.1994.tb00123.x
- ↑ Jump up to: 15.0 15.1 Ross EV, Miller C, Meehan K, et al. One-pass CO2 versus multiple-pass Er:YAG laser resurfacing in the treatment of rhytides: a comparison side-by-side study of pulsed CO2 and Er:YAG lasers. Dermatol Surg. 2001;27(8):709-715. doi:10.1046/j.1524-4725.2001.01015.x
- ↑ Jump up to: 16.0 16.1 Newman JB, Lord JL, Ash K, McDaniel DH. Variable pulse erbium:YAG laser skin resurfacing of perioral rhytides and side-by-side comparison with carbon dioxide laser. Lasers Surg Med. 2000;26(2):208-214. doi:10.1002/(sici)1096-9101(2000)26:2<208::aid-lsm12>3.0.co;2-r
- ↑ Janik JP, Markus JL, Al-Dujaili Z, Markus RF. Laser resurfacing. Semin Plast Surg. 2007;21(3):139-146. doi:10.1055/s-2007-991182 (Save for MOA)
- ↑ Goldman MP, Marchell N, Fitzpatrick RE. Laser skin resurfacing of the face with a combined CO2/Er:YAG laser. Dermatol Surg. 2000;26(2):102-104. doi:10.1046/j.1524-4725.2000.98208.x
- ↑ Jump up to: 19.0 19.1 19.2 Tierney EP, Eisen RF, Hanke CW. Fractionated CO2 laser skin rejuvenation. Dermatol Ther. 2011;24(1):41-53. doi:10.1111/j.1529-8019.2010.01377.x
- ↑ Kyung Eun Jung, Kum Hee Jung, Young Min Park, Jun Young Lee, Tae Yoon Kim, Hyung Ok Kim & Hei Sung Kim (2013) A Split-face comparison of ablative fractional lasers (CO2 and Er:YAG) in Asian patients; postprocedure erythema, pain and patient's satisfaction, Journal of Cosmetic and Laser Therapy, 15:2, 70-73, DOI: 10.3109/14764172.2012.759053
- ↑ Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg. 2009;35(10):1445-1461. doi:10.1111/j.1524-4725.2009.01258.x
- ↑ Jump up to: 22.0 22.1 Metelitsa AI, Alster TS. Fractionated laser skin resurfacing treatment complications: a review. Dermatol Surg. 2010;36(3):299-306. doi:10.1111/j.1524-4725.2009.01434.x
- ↑ Waldorf HA, Kauvar AN, Geronemus RG. Skin resurfacing of fine to deep rhytides using a char-free carbon dioxide laser in 47 patients. Dermatol Surg. 1995;21(11):940-946. doi:10.1111/j.1524-4725.1995.tb00530.x
- ↑ Jump up to: 24.0 24.1 24.2 Alster TS, Garg S. Treatment of facial rhytides with a high-energy pulsed carbon dioxide laser. Plast Reconstr Surg. 1996;98(5):791-794. doi:10.1097/00006534-199610000-00005
- ↑ Kim YJ, Lee HS, Son SW, Kim SN, Kye YC. Analysis of hyperpigmentation and hypopigmentation after Er:YAG laser skin resurfacing. Lasers Surg Med. 2005;36(1):47-51. doi:10.1002/lsm.20120
- ↑ Jump up to: 26.0 26.1 26.2 Nestor MS. Prophylaxis for and treatment of uncomplicated skin and skin structure infections in laser and cosmetic surgery. J Drugs Dermatol. 2005;4(6 Suppl):s20-s25.
- ↑ Lowe NJ, Lask G, Griffin ME. Laser skin resurfacing. Pre- and posttreatment guidelines. Dermatol Surg. 1995;21(12):1017-1019.
- ↑ Avram MM, Tope WD, Yu T, Szachowicz E, Nelson JS. Hypertrophic scarring of the neck following ablative fractional carbon dioxide laser resurfacing [published correction appears in Lasers Surg Med. 2009 Jul;41(5):398]. Lasers Surg Med. 2009;41(3):185-188. doi:10.1002/lsm.20755
- ↑ Ross EV, Amesbury EC, Barile A, Proctor-Shipman L, Feldman BD. Incidence of postoperative infection or positive culture after facial laser resurfacing: a pilot study, a case report, and a proposal for a rational approach to antibiotic prophylaxis. J Am Acad Dermatol. 1998;39(6):975-981. doi:10.1016/s0190-9622(98)70273-7
- ↑ Walia S, Alster TS. Cutaneous CO2 laser resurfacing infection rate with and without prophylactic antibiotics. Dermatol Surg. 1999;25(11):857-861. doi:10.1046/j.1524-4725.1999.99114.x
- ↑ Orringer JS, Kang S, Johnson TM, et al. Tretinoin treatment before carbon-dioxide laser resurfacing: a clinical and biochemical analysis. J Am Acad Dermatol. 2004;51(6):940-946. doi:10.1016/j.jaad.2004.04.040
- ↑ Mandy SH. Tretinoin in the preoperative and postoperative management of dermabrasion. J Am Acad Dermatol. 1986;15(4 Pt 2):878-889. doi:10.1016/s0190-9622(86)70245-4
- ↑ Jump up to: 33.0 33.1 Gaitan S, Markus R. Anesthesia methods in laser resurfacing. Semin Plast Surg. 2012;26(3):117-124. doi:10.1055/s-0032-1329416
- ↑ Brightman LA, Brauer JA, Anolik R, et al. Ablative and fractional ablative lasers. Dermatol Clin. 2009;27(4):479-vii. doi:10.1016/j.det.2009.08.009
- ↑ Jump up to: 35.0 35.1 35.2 35.3 35.4 35.5 Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008;58(5):719-740. doi:10.1016/j.jaad.2008.01.003
- ↑ Tierney EP, Hanke CW, Petersen J. Ablative fractionated CO2 laser treatment of photoaging: a clinical and histologic study. Dermatol Surg. 2012;38(11):1777-1789. doi:10.1111/j.1524-4725.2012.02572.x
- ↑ Batra RS, Ort RJ, Jacob C, Hobbs L, Arndt KA, Dover JS. Evaluation of a silicone occlusive dressing after laser skin resurfacing. Arch Dermatol. 2001;137(10):1317-1321. doi:10.1001/archderm.137.10.1317
- ↑ Chan HH, Manstein D, Yu CS, Shek S, Kono T, Wei WI. The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2007;39(5):381-385. doi:10.1002/lsm.20512
- ↑ Khatri KA, Mahoney DL, McCartney MJ. Laser scar revision: A review. J Cosmet Laser Ther. 2011;13(2):54-62. doi:10.3109/14764172.2011.564625
- ↑ Jump up to: 40.0 40.1 40.2 40.3 40.4 40.5 Narurkar VA. Nonablative fractional laser resurfacing. Dermatol Clin. 2009;27(4):473-vi. doi:10.1016/j.det.2009.08.012
- ↑ Rubenstein R, Roenigk HH Jr, Stegman SJ, Hanke CW. Atypical keloids after dermabrasion of patients taking isotretinoin. J Am Acad Dermatol. 1986;15(2 Pt 1):280-285. doi:10.1016/s0190-9622(86)70167-9
- ↑ Jump up to: 42.0 42.1 42.2 42.3 42.4 DeHoratius DM, Dover JS. Nonablative tissue remodeling an
- ↑ Adrian RM, Tanghetti EA. Long pulse 532-nm laser treatment of facial telangiectasia. Dermatol Surg. 1998;24(1):71-74. doi:10.1111/j.1524-4725.1998.tb04055.x
- ↑ Lee MW. Combination 532-nm and 1064-nm lasers for noninvasive skin rejuvenation and toning [published correction appears in Arch Dermatol. 2004 May;140(5):625]. Arch Dermatol. 2003;139(10):1265-1276. doi:10.1001/archderm.139.10.1265
- ↑ Goldberg D, Tan M, Dale Sarradet M, Gordon M. Nonablative dermal remodeling with a 585-nm, 350-microsec, flashlamp pulsed dye laser: clinical and ultrastructural analysis. Dermatol Surg. 2003;29(2):161-164. doi:10.1046/j.1524-4725.2003.29040.x
- ↑ Rostan E, Bowes LE, Iyer S, Fitzpatrick RE. A double-blind, side-by-side comparison study of low fluence long pulse dye laser to coolant treatment for wrinkling of the cheeks. J Cosmet Laser Ther. 2001;3(3):129-136. doi:10.1080/147641701753414933
- ↑ Goldberg DJ. Full-face nonablative dermal remodeling with a 1320 nm Nd:YAG laser. Dermatol Surg. 2000;26(10):915-918. doi:10.1046/j.1524-4725.2000.026010915.x
- ↑ Lask, G. P., Lee, P. K., Seyfzadeh, M., Nelson, J. S., Milner, T. E., Anvari, B., ... & Berry, M. J. (1997, May). Nonablative laser treatment of facial rhytides. In Lasers in surgery: advanced characterization, therapeutics, and systems VII (Vol. 2970, pp. 338-349). International Society for Optics and Photonics.
- ↑ Kelly KM, Nelson JS, Lask GP, Geronemus RG, Bernstein LJ. Cryogen spray cooling in combination with nonablative laser treatment of facial rhytides. Arch Dermatol. 1999;135(6):691-694. doi:10.1001/archderm.135.6.691
- ↑ Friedman PM, Jih MH, Kimyai-Asadi A, Goldberg LH. Treatment of inflammatory facial acne vulgaris with the 1450-nm diode laser: a pilot study. Dermatol Surg. 2004;30(2 Pt 1):147-151. doi:10.1111/j.1524-4725.2004.30062.x
- ↑ Sadick NS, Weiss R. Intense pulsed-light photorejuvenation. Semin Cutan Med Surg. 2002;21(4):280-287. doi:10.1053/sder.2002.36902
- ↑ Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol Surg. 2000;26(9):835-843. doi:10.1046/j.1524-4725.2000.00085.x
- ↑ Jump up to: 53.0 53.1 Wanner M, Tanzi EL, Alster TS. Fractional photothermolysis: treatment of facial and nonfacial cutaneous photodamage with a 1,550-nm erbium-doped fiber laser. Dermatol Surg. 2007;33(1):23-28. doi:10.1111/j.1524-4725.2007.33003.x
- ↑ Jump up to: 54.0 54.1 Yaghmai D, Garden JM, Bakus AD, Massa MC. Comparison of a 1,064 nm laser and a 1,320 nm laser for the nonablative treatment of acne scars. Dermatol Surg. 2005;31(8 Pt 1):903-909. doi:10.1097/00042728-200508000-00003