Lacrimal Fistula, Congenital
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
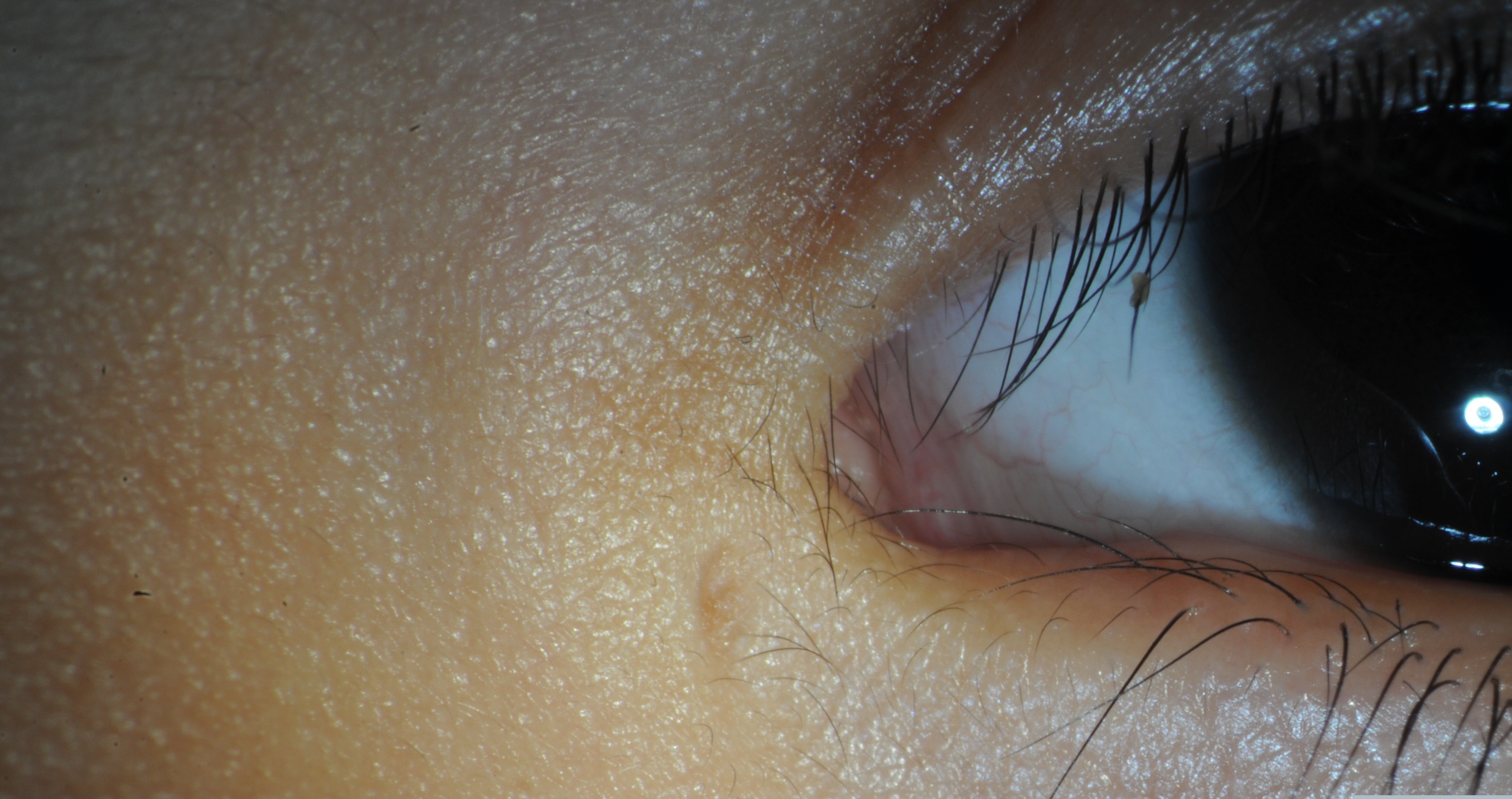
Congenital lacrimal fistulas, also known as lacrimal anlage ducts, are supernumerary lacrimal canaliculi that connect the skin to the common canaliculus or the lacrimal sac (Figure 1).[1][2][3] These rare developmental abnormalities can lead to epiphora[2]
Disease
Lacrimal Fistula (ICD-9 #375.61, ICD-10 #H04.61)
Etiology
This congenital abnormality results from improper formation of the nasolacrimal drainage system, which arises along the line of the ectodermal cleft between the lateral nasal and maxillary processes of the developing embryo.[1] Originally a solid epithelial cord, the canaliculi canalize around day 60 of gestational age and the puncta are patent by the seventh fetal month.[2] It has been postulated that this cord of epithelial cells, also known as the lacrimal anlage, fails to involute in cases of congenital lacrimal fistula. The cord proliferates abnormally and subsequently canalizes, resulting in an aberrant lacrimal drainage system.[4] Competing theories implicate budding from the lacrimal drainage system during embryogenesis[5], amniotic bands, incomplete closure of the embryonic fissure, or inflammatory processes as causative factors.[2][6]
Epidemiology
The prevalence of congenital lacrimal fistulae is around 1 in 2000 live births.
Risk Factors
Congenital lacrimal fistulas are not generally associated with systemic disease; however, they has been reported to be associated with the following conditions: [7]
- Thalassemia
- Preauricular fistula
- Hypospadias
- Balanced 6p and 13 translocation
- CHARGE syndrome
- VACTERL
- Naso-orbital meningocele
- Ectrodactyly-ectodermal dysplasia-clefting syndrome
- Down syndrome
In addition, families with multiple members exhibiting congenital lacrimal fistulas – particularly bilateral fistulas – have been reported.[8][9]
General Pathology
Congenital lacrimal fistulas typically arise from the common canaliculus or the lacrimal sac. The external ostium of the fistula is most often found inferonasal to the medial canthal angle.[2][3] Lacrimal fistulas have a histologic structure very similar to that of typically-developed canaliculi. Those that have been reported usually have a stratified squamous epithelial lining identical to that of a normal canaliculus.[10]
Diagnosis
Diagnosis of congenital lacrimal fistulas can be made on routine examination or directed by patient complaints.
History
Congenital lacrimal fistulas are normally either asymptomatic[11] or revealed after complaints of epiphora[2] or clear mucoid discharge from the fistula’s ostium.[3] Questions regarding redness around the eyelids, tenderness in the periocular structures, purulent discharge, swelling, fevers, chills, and other B symptoms should be asked in order to differentiate congenital lacrimal fistula from an inflammatory process. Information regarding birth history, family history, and other congenital abnormalities should be elicited.
Physical examination
Congenital lacrimal fistulas are often found shortly after birth on routine examination,[11] appearing as a small indentations or holes located inferonasal to the medial canthal angle.[3] They are typically unilateral[10] although numerous bilateral cases have been reported.[8]
Signs
Patients often present with tearing despite a patent nasolacrimal system. An opening inferonasal to the medial canthal angle will be seen either unilaterally or bilaterally. Eyelid dermatitis due to chronic epiphora has also been reported associated with congenital lacrimal fistulas.[12]
Symptoms
A patient will not typically have any systemic symptoms related to a lacrimal fistula. Affected patients are either asymptomatic or complain of either epiphora or mucoid discharge. Mucoid discharge is frequently associated with concurrent nasolacrimal duct obstruction and may resolve with treatment of the distal obstruction.
Clinical diagnosis
The clinical diagnosis is established by both the history and the examination. The history supports the diagnosis when a patient continues to have epiphora despite a nasolacrimal duct that has been proven patent by previous testing. Physical examination, via visualization of the ostium of the lacrimal fistula, is key to its diagnosis.
Diagnostic procedures
Patients are often evaluated by nasolacrimal probing, irrigation, and/or intubation dacryocystography.[2] A dye disappearance test can also be performed to test for normal function of the lacrimal drainage system; this is particularly helpful in young children, who can be uncooperative with examination.[9]
Differential diagnosis
- Atresia of the nasolacrimal duct/congenital nasolacrimal duct occlusion [1]
- Lacrimal sac mucocele[2]
- Acquired lacrimal sac fistula[13][14][15]
- Trauma
- Dacryocystitis
- Malignancy
Management
Management consists of either observation or surgical intervention as determined by the patient’s symptoms.
General treatment
Many patients with congenital lacrimal fistulas are asymptomatic and are observed, with intervention only if developing symptoms of tearing or mucous discharge.
General follow up
After diagnosis, patients are followed up on an as-needed basis if they are asymptomatic.
Surgical treatment
Symptomatic patient require surgical intervention. Simple cautery of the fistula tract has been attempted; however, it is often unsuccessful.[3] Surgical management is somewhat controversial, with some authors advocating excision of the fistula tract with optional stenting of the lacrimal drainage system and others arguing that a dacryocystorhinostomy (DCR) is necessary in addition to fistula excision and nasolacrimal system intubation. The lacrimal drainage system should be confirmed to be patent prior to perform excision to avoid postoperative epiphora and dacryocystitis.
Proponents of fistula ligation and excision with or without nasolacrimal intubation have reported a high success rate with low risk of complications (Figure 2). In the largest series examining this treatment modality, 14 of 14 patients (9 of whom underwent excision alone and 5 of whom had additional nasolacrimal intubation due to concomitant obstruction of the nasolacrimal system) experienced resolution of epiphora after surgical treatment. No complications were reported.[3]
Advocates of DCR in addition to excision of the fistula [2][10]argue that simple cauterization or excision of the fistula could compromise the remainder of the lacrimal drainage system, as many fistulas originate from the common canaliculus, which can be easily damaged if the lacrimal sac is not opened and the base of the fistula is not visualized at the time of its removal. In addition, the increased facility to tear outflow after a DCR causes tears to flow preferentially down the nasolacrimal duct rather than being shunted out of the fistula tract. In the largest surgical series published on congenital lacrimal fistulas, DCR with fistula excision and nasolacrimal intubation resulted in a 95% functional success rate in 21 eyes.[2]
Variations on these surgical techniques, including intraoperative use of a polyvinyl siloxane cast to protect and identify the nasolacrimal sac during DCR, have been reported.[16]
Figure 2: Same lacrimal fistula displayed in Figure 1 after excision of fistula tract
Surgical follow up
Patients are typically seen one to two times in the immediate postoperative period. If a DCR or nasolacrimal intubation is performed, the nasolacrimal stent is removed 3 – 12 months postoperatively, depending on surgeon preference. Patients can typically be transitioned to an as needed follow-up regimen if they remain asymptomatic.
Complications
Complications of surgical management include infection, recurrent or worsening of epiphora, poor cosmetic result, bleeding, damage to lid structures or nose.
Prognosis
The prognosis for patients with congenital lacrimal fistulas is quite good. Many are asymptomatic, and those who have symptomatic epiphora or mucoid discharge can be treated surgically with a high success rate.
References
- ↑ 1.0 1.1 1.2 Older J: Congenital Lacrimal Disorders and Management. In: Lacrimal Surgery. edn. Edited by Linberg J. New York: Churchill Livingstone; 1988: 91-108.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Welham RA, Bergin DJ: Congenital lacrimal fistulas. Arch Ophthalmol 1985, 103(4):545-548.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Birchansky LD, Nerad JA, Kersten RC, Kulwin DR: Management of congenital lacrimal sac fistula. Arch Ophthalmol 1990, 108(3):388-390.
- ↑ Jones T, Wobig J: Surgery of the Eyelids and Lacrimal System. Birmingham, AL: Aesculapius Publishing Co; 1976.
- ↑ Chaung JQ, Sundar G, Ali MJ. Congenital lacrimal fistula: A major review. Orbit. 2016 Aug;35(4):212-20. doi: 10.1080/01676830.2016.1176052. Epub 2016 May 18. PMID: 27191932.
- ↑ Duke-Elder S: System of Ophthalmology, vol. 3. St Louis, MO: CV Mosby Co; 1963.
- ↑ Lee S, Kim N, Khwarg SI, Choung HK, Lee MJ: Congenital lacrimal fistula associated with Down syndrome. Graefes Arch Clin Exp Ophthalmol 2012, 250(10):1515-1519.
- ↑ 8.0 8.1 Zhuang L, Sylvester CL, Simons JP: Bilateral congenital lacrimal fistulae: a case report and review of the literature. Laryngoscope 2010, 120 Suppl 4:S230.
- ↑ 9.0 9.1 Maden A, Yilmaz S, Ture M: Hereditary lacrimal fistula. Orbit 2008, 27(1):69-72.
- ↑ 10.0 10.1 10.2 Masi AV. Congenital fistula of the lacrimal sac. Arch Ophthalmol 1969, 81(5):701-704.
- ↑ 11.0 11.1 Howard RO, Caldwell JB: Congenital fistula of the lacrimal sac. Am J Ophthalmol 1969, 67(6):931-934.
- ↑ Yen MT, Yen KG, Anderson RL. Perivascular dermatitis of the eyelid secondary to chronic epiphora. Can J Ophthalmol. 2004 Dec;39(7):792-4. doi: 10.1016/s0008-4182(04)80078-4. PMID: 15696774.
- ↑ Barrett RV, Meyer DR: Acquired lacrimal sac fistula after incision and drainage for dacryocystitis: a multicenter study. Ophthal Plast Reconstr Surg 2009, 25(6):455-457.
- ↑ Litwin AS, Timlin H, Sagili S, Wright M, Malhotra R: Acquired lacrimal sac fistula mimicking basal cell carcinoma. Br J Dermatol 2013.
- ↑ Shams PN, Selva D: Traumatic sinolacrimocutaneous fistula managed with endonasal dacryocystorhinostomy and anterior ethmoidectomy. Arch Ophthalmol 2012, 130(10):1311-1313.
- ↑ Bhatnagar A, Eckstein LA, Douglas RS, Goldberg RA: Congenital lacrimal sac fistula: intraoperative visualization by polyvinyl siloxane cast. Ophthal Plast Reconstr Surg 2008, 24(2):158-60.
Acknowledgements
The author would like to thank Louise Mawn, MD, of Vanderbilt Eye Institute, for her contributions to this article.