Keratoacanthoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Keratoacanthoma (KA), also known as molluscum sebaceum [1], is a hyperkeratotic dome-shaped nodule that can grow up to one to three centimeters within a few months. It is a low-grade skin tumor found on sun-exposed areas such as the head, hands, arms and trunk.[2][3] It is most important for the ophthalmologists because it can occur on the eyelids. Although KA is characterized by a benign growth, its differentiation from squamous cell carcinoma (SCC) is of upmost importance. For some, KA represents a spontaneous regressive form of SCC ,[4] [5] while other researchers favor a strict differentiation between these two entities based on gene expression [6] and/or expression of cutaneous markers.[7]
Etiology
KA is primarily associated with sun exposure in elderly people. Chemical carcinogens also play a role in its pathogenesis.[8] No genetic basis has been yet identified.
Risk Factors
General Pathology
Gross Pathology [9]
Keratoacantoma appears as a solitary flesh-colored dome shaped lesion with central keratin-filled plug.
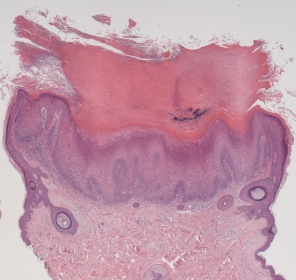
Histology [9]
There is no single histological finding that can characterize keratoacanthoma. Rather, histologic diagnosis requires a constellation of findings:
- Exoendophytic lesion composed of layers of well-differentiated squamous epithelium resulting from acanthosis
- Central keratin-filled crater that may enlarge as the lesion evolves and matures
- Larger mature keratinocytes are found towards the center of tumor cell nests
- Cytoplasm of large keratinocytes give eosinophilic hue on H & E stain.
- Buttressing (lipping) of the lesion edges around the central crater, creating a symmetrical appearance
- Adjacent dermis may contain small micro abscesses composed of mixed inflammatory infiltrate (eosinophils and neutrophils)
Note: Histologic features that favor keratoacanthoma over squamous cell carcinoma include hemispheric flask like shape with overhanging edges and central keratin plug
Variants (from a dermatologic point of view)
- Actinic
- Follicular:[9]
- Giant: [9]
- Multinodular keratoacanthoma) [9]:
- Subungual keratoacanthomas [9]:
- Multiple Keratoacanthoma [9]: These may be seen in Torre’s syndrome (Muir-Torre syndrome) where multiple keratoacanthomas may be associated with underlying primary visceral cancer, most often of the GI tract.
Diagnosis
History
KA commonly presents in old men with fair skin on sun-exposed area. It is a self-limited benign growth characterized by a rapidly enlarging, solitary flesh-colored nodule, followed by a period of stability, which later involutes, leaving behind a scarring lesion. [8] [2]
Physical examination
KA lesions classically present as a quickly growing, firm, flesh-colored papule. The proliferative phase is characterized by a symmetrical, smooth surfaced lesion that progressively ulcerates, forming a hyperkeratotic dome-shaped nodule; often described as a horn like projection. [2]It can also demonstrate a cup-shaped appearance with the central ulceration. [10]Within 1-2 months, it can rapidly grow to 1-2 cm. If on the nose or eyelids, extensive local tissue destruction may occur. Although the duration of the lesion may be variable (few months to a year), it often spontaneously regresses leaving behind a hypopigemented scar.[9]
Clinical diagnosis
Excisional or deep incisional biopsy of the lesion is the preferred tool for establishing the diagnosis of KA. [3]
Diagnostic procedures
The diagnosis can be made by histopathology.
Differential diagnosis [3]
- Actinic Keratosis
- Squamous cell carcinoma
- Cutaneous Horn
- Molluscum contagiosum
Management
General therapy usually consists of cryosurgery, electrodessication and curettage, excision, Mohs micrographic surgery and Radiation treatment (X-ray). Medication therapies such as antineoplastic agents are usually prescribed for patients who have usually more aggressive lesions. Some examples include topical and intralesional 5-fluorouracil, methotrexate and bleomycin.[2][3]
References
- ↑ Georgescu, t., Oproiu, a. m., Rădăşan, m. g., Dumitru, a. v., Costache, d., Pătraşcu, o. m., . . . Costache, m. (n.d.). Keratoacanthoma centrifugum marginatum: an unusual clinical and histopathological diagnostic pitfall. Romanian Journal of Morphology & Embryology, 2017, 58:561-565
- ↑ 2.0 2.1 2.2 2.3 Goldsmith, L. A., Katz, S. I., Gilchrest, B. A., Paller, A. S., Leffell, D. J., & Wolff, K. (2012). Fitzpatrick's Dermatology in General Medicine (8th ed., Vol. 1). The McGraw-Hill Companies, Inc.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Usatine, R. P., Smith, M. A., Chumley, H. S., & Mayeaux Jr., E. J. (2013). The Color Atlas of Family Medicine (2nd ed.). The McGraw-Hill Companies, Inc.
- ↑ Manstein CH, Frauenhoffer CJ, Besden JE. Keratoacanthoma: is it a real entity? Ann Plast Surg, 1998, 40:469–472.
- ↑ Gleich T, Chiticariu E, Huber M, Hohl D. Keratoacanthoma: a distinct entity? Exp Dermatol, 2016, 25:85–91.
- ↑ Ra SH, Su A, Li X, Zhou J, Cochran AJ, Kulkarni RP, Binder SW. Keratoacanthoma and squamous cell carcinoma are distinct from a molecular perspective. Mod Pathol, 2015, 28:799–806.
- ↑ Kanzaki A, Kudo M, Ansai S, Peng WX, Ishino K, Yamamoto T, Wada R, Fujii T, Teduka K, Kawahara K, Kawamoto Y, Kitamura T, Kawana S, Saeki H, Naito Z. Insulin-like growth factor 2 mRNA-binding protein-3 as a marker for distinguishing between cutaneous squamous cell carcinoma and kerato- acanthoma. Int J Oncol, 2016, 48:1007–1015.
- ↑ 8.0 8.1 Ghadially FN, Barton BW, Kerridge DF: The etiology of keratoacanthoma. Cancer 16:603, 1963
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Weedon, D. (2002). Skin Pathology. 2nd ed. London: Churchill Livingstone, pp.778-781.
- ↑ Chiou C, Wolkow N, Freitag SK. Eyelid Keratoacanthoma in an 86-Year-Old Man: Clinical and Histopathologic Features. Ophthalmic Plast Reconstr Surg. 2021 May-Jun 01;37(3S):S166. doi: 10.1097/IOP.0000000000001721. PMID: 32732539.