Inverted Flap Technique
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical Therapy
Inverted flap technique (or inverted internal limiting membrane flap technique) for macular hole closure.
Background
Macular holes are one of the main vitreoretinal interface disorders and their prevalence varies from 0.2 to 0.7% in the general population [1]. They are due to an anatomical defect in the fovea which causes the poor central vision reported in this entity (see detailed information on "Macular Hole" here ).
In 1991, Kelly and Wendel [2] described the first surgical approach to this condition which, until then, was considerable untreatable. The rational of the surgery was the identification and treatment of vitreoretinal traction forces, either tangential, anteroposterior or both. Ever since, the treatment strategy has been improving and currently most of macular holes (around 85-90%[1]) can be successfully closed using a procedure involving pars plana vitrectomy, dye-assisted internal limiting membrane peeling, and gas tamponade. However, for some macular holes such as those which are large, chronic, or associated with myopia, surgical failure is more commonly seen. In fact, the rate of persistent macular hole varies between 8-44%[1] in literature. In 2010, Michalewska et al[3] introduced the inverted flap technique, thus providing a new surgical approach to overcome these challenging scenarios. On their original description of the inverted flap technique, Michalewska et al reported a 98% closure rate of large macular holes (defined as > 400 µm, according to the classification in the International Vitreomacular Traction Study[4]). As the success of the procedure was broadly demonstrated since the beginning, the indications and applications of the technique have grown, surpassing the previous standard procedures in selected situations.
Patient Selection
The inverted internal limiting membrane flap technique was originally described to address challenging cases of large macular holes[3] and myopic macular holes[5], where it achieved higher anatomic success rate than the standard technique.
This procedure is not indicated in eyes with previous internal limiting membrane removal around the macular hole[6].
Common Indications
Idiopathic Full-Thickness Large Macular Hole
The anatomical success of the surgical treatment of large macular holes (usually defined as having a diameter >400 µm, based on the horizontally measured linear width at the narrowest point of the hole) using vitrectomy and internal limiting membrane peeling is reportedly low. In fact, large macular holes have been recorded to remain open after primary repair in up to 44% of cases[1]. Consequently, the inverted flap technique was developed to resolve these challenging situations[3]. The success that it demonstrated when compared to standard treatment resulted in its dissemination as a primary choice.
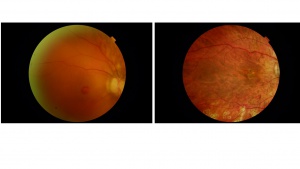
Myopic Macular Holes
In patients with macular hole and myopia, the incidence of retinal detachment increases as myopia worsens (97.6% retinal detachment in myopia over −8.25 D, 67.7% retinal detachment in myopia between −8.0 and −3.25 D and 1.1% retinal detachment in myopia under −3.0 D)[7][8]. High myopia is often associated with posterior staphyloma with increasing the tangential macular traction at the vitreoretinal interface, likely increasing the odds of developing a macular hole and possibly a retinal detachment. Myopic macular holes, associated or not with retinal detachment, are a challenging to repair and the functional and anatomical recovery is seldom achieved with standard vitrectomy and internal limiting membrane peeling. Michalewska et al [5] first demonstrated the efficacy of the inverted flap technique by successfully repairing 100% of the myopic macular holes in their study and improving visual acuity.
Macular Hole associated with Retinal Detachment
Macular holes associated with retinal detachment, especially in high myopia, present a demanding situation with frequent low closure rates. An open macular hole in these cases not only impairs central vision but also increase the risk of recurrent retinal detachment. Inverted flap technique has also demonstrated increased success rate when compared to the standard procedure in these patients [8][9][10][11].
Other Possible Indications
Given the success of the technique, its use has been expanded to other scenarios, such as traumatic macular holes [12][13], where the standard approach demonstrates a low success rate. Nevertheless, more sustained evidence is required to prove the superiority of the above-mentioned method in such scenarios.
Surgical Technique
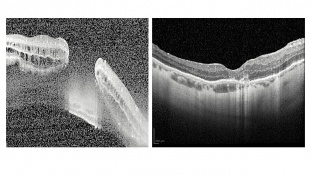
According to the original description[3], the surgery steps are :
- Core vitrectomy and optional staining of the ILM with Brilliant Blue G, trypan blue, ICG green, or triamcinolone acetonide are performed.
- The internal limiting membrane is grasped with an internal limiting membrane forceps and peeled off in a circular fashion for approximately 2-disc diameters around the macular hole.
- During the circumferential peeling, the internal limiting membrane is not removed completely from the retina. Instead, it is left attached to the edges of the macular hole. In the modified technique described by Michalewska and colleagues, only the temporal ILM is peeled and left hinged at the temporal edge of the macular hole.
- A peripheral piece of the internal limiting membrane is trimmed with a vitreous cutter or scissors and the central part of the internal limiting membrane is left in place. Small remnants of the internal limiting membrane remain surrounding the macular hole.
- The internal limiting membrane is gently massaged over the macular hole from all sides until the internal limiting membrane become inverted (upside down such that the surface normally facing the vitreous body now faces the retinal pigmented epithelium).
- At the final of the procedure, the macular hole is covered with the inverted internal limiting membrane flap.
- At the end of surgery, fluid-air exchange is performed, and patients are asked to maintain a facedown position for 3 days to 4 days postoperatively.
The technique is demonstrated in the video below (the video demonstrates the procedure performed by our group, courtesy of Dr. Antonio Rocha):
Mechanism of Inverted Flap Technique
The procedure aims to eliminate the anteroposterior and tangential traction exerted on the retinal surface by removing all cortical vitreous and surface components of the retina, namely epiretinal membranes, and internal limiting membrane, while stimulating cell proliferation and migration of glial cells into the macular hole. Therefore, it enhances the chances of closure and potentially improves the postoperative visual acuity.
Histopathological Mechanism
The histopathological mechanism of macular hole closure using the inverted flap technique is thought to be multifactorial.
The internal limiting membrane, that contain Muller cells, may help inducing gliosis and provide a scaffold for glial cell proliferation thereby facilitating the closure of the hole. An experimental study in macular hole models corroborated this theory, and found that activated Muller cells present on the surface of the internal limiting membrane produce neurotrophic factors that may contribute to macular hole closure [14].
Outcomes
Several studies have reported the success of the inverted flap technique in both anatomical closure of the macular hole and functional recovery under different circumstances.
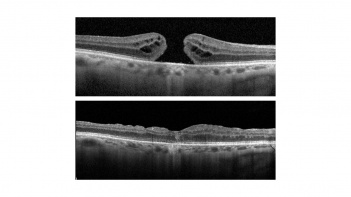
Idiopathic Full-Thickness Large Macular Hole
A randomized trial [15]compared conventional internal limiting membrane peeling versus inverted flap technique in idiopathic large macular hole (diameter >600 μm) and found anatomical success rates of 70 and 90% and functional recovery of 1.4 versus 2.1 lines, respectively. Another trial [16]compared three techniques (conventional internal limiting membrane peeling, inverted flap and free-flap technique) and concluded that the inverted flap induces a faster and more significant recovery. Moreover, other non-controlled studies have demonstrated similar results[17][18][19].
Myopic Macular Hole (associated or not with Retinal Detachment)
A metanalysis [8] compared vitrectomy with inverted internal limiting membrane flap versus internal limiting membrane peeling for macular hole retinal detachment in high myopia, and concluded that the inverted internal limiting membrane flap contributed to a higher macular hole closure rate than internal limiting membrane peeling. Nonetheless, no differences were found regarding visual improvement. A previous metanalysis had also been performed achieving similar results[20].
Complications
Most of the complications are similar to the standard vitrectomy and internal limiting membrane peeling.
It is worth noting that the inverted internal limiting membrane flap may detach spontaneously during the fluid-air exchange. Thus, this step must be carefully performed to achieve a successful result.
As the internal limiting membrane is the basement membrane of the retinal glia, thereby playing an important role in buffering the intraretinal potassium concentration, it has been argued that the flap technique may disturb this process thus inducing retinal damage. However, when this was accessed using multifocal electroretinograms and microperimetry, no deficits were found[21].
Special Considerations and Variations of the Technique
Several variations of the technique have been adopted:
- The temporal internal limiting membrane flap [22]a modification in which the internal limiting membrane is peeled only from the temporal side of the fovea. A 2-disc-diameter area of internal limiting membrane is removed from the temporal side of the fovea and inverted to cover the macular hole. No significant difference in initial and final visual acuity between conventionally inverted internal limiting membrane flap and temporal internal limiting membrane flap technique was evident, although less dissociated optic nerve fiber layer appearance was observed with the temporal ILM technique.
- In the cabbage leaf inverted internal limiting membrane flap technique[23], multiple internal limiting membrane flaps are inverted over each other covering the hole. The technique has been proposed for cases of chronic, large, full-thickness macular hole.
- The inverted internal limiting membrane flap without extra manipulation[24] has also been described. In this technique the flap is not tucked into the macular hole, as originally described. This technique may reduce the risk of iatrogenic damage to the retinal pigmented epithelium, yet extreme care must be taken during fluid-air exchange to keep the macular hole covered.
Conclusion
Vitrectomy associated with the inverted internal limiting membrane flap technique seems to be an effective approach to repairing macular holes that are predisposed to a lower probability of closure, such as refractory, large, or chronic holes.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 Tam ALC, Yan P, Gan NY, Lam WC. The current surgical management of large, chronic, recurrent, or persistent macular holes. Retina. 2018;38(7):1263-1275.
- ↑ Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol (Chicago, Ill 1960). 1991;109(5):654-659.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117(10):2018-2025.
- ↑ Duker JS, Kaiser PK, Binder S, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611-2619.
- ↑ Jump up to: 5.0 5.1 Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina. 2014;34(4):664-669.
- ↑ Park JH, Lee SM, Park SW, Lee JE, Byon IS. Comparative analysis of large macular hole surgery using an internal limiting membrane insertion versus inverted flap technique. Br J Ophthalmol. 2019;103(2):245-250.
- ↑ Ishida S, Yamazaki K, Shinoda K, Kawashima S, Oguchi Y. Macular Hole Retinal Detachment in Highly Myopic Eyes: ultrastructure of surgically removed epiretinal membrane and clinicopathologic correlation. Retina. 2000;20(2):176-183
- ↑ Jump up to: 8.0 8.1 8.2 Xu Q, Luan J. Vitrectomy with inverted internal limiting membrane flap versus internal limiting membrane peeling for macular hole retinal detachment in high myopia: a systematic review of literature and meta-analysis. Eye. 2019.
- ↑ Sasaki H, Shiono A, Kogo J, et al. Inverted internal limiting membrane flap technique as a useful procedure for macular hole-associated retinal detachment in highly myopic eyes. Eye. 2017;31(4):545-550.
- ↑ Matsumura T, Takamura Y, Tomomatsu T, et al. Comparison of the Inverted Internal Limiting Membrane Flap Technique and the Internal Limiting Membrane Peeling for Macular Hole with Retinal Detachment. Hartnett ME, ed. PLoS One. 2016;11(10):e0165068.
- ↑ Kinoshita T, Onoda Y, Maeno T. Long-term surgical outcomes of the inverted internal limiting membrane flap technique in highly myopic macular hole retinal detachment. Graefe’s Arch Clin Exp Ophthalmol. 2017;255(6):1101-1106.
- ↑ Browne AW, Conti FF, Kaiser PK, Singh RP. Surgical Repair of Traumatic Macular Holes With Extreme Macular Pathology Using an Internal Limiting Membrane Flap Technique. Ophthalmic Surgery, Lasers Imaging Retin. 2018;49(10):e143-e146. doi:10.3928/23258160-20181002-17
- ↑ Astir S, Shroff D, Gupta C, Shroff C. Inverted flap technique for a large traumatic macular hole with choroidal rupture and subretinal hemorrhage. Oman J Ophthalmol. 11(1):68-70. doi:10.4103/0974-620X.226348
- ↑ Shiode Y, Morizane Y, Matoba R, et al. The role of inverted internal limiting membrane flap in macular hole closure. Investig Ophthalmol Vis Sci. 2017;58(11):4847-4855.
- ↑ Kannan NB, Kohli P, Parida H, Adenuga OO, Ramasamy K. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC Ophthalmol. 2018;18(1):177.
- ↑ Velez-Montoya R, Ramirez-Estudillo JA, Sjoholm-Gomez de Liano C, et al. Inverted ILM flap, free ILM flap and conventional ILM peeling for large macular holes. Int J Retina Vitreous. 2018;4:8. Published 2018 Feb 19.
- ↑ Narayanan R, Singh SR, Taylor S, et al. Surgical outcomes after inverted internal limiting membrane flap versus conventonal peeling for very large macular holes. Retina.April 2018:1.
- ↑ Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F. Internal Limiting Membrane Peeling Versus Inverted Flap Technique for Treatment of Full-Thickness Macular Holes. Retina. 2018;38(Ilm):S73-S78.
- ↑ Yamashita T, Sakamoto T, Terasaki H, et al. Best surgical technique and outcomes for large macular holes: retrospective multicentre study in Japan. Acta Ophthalmol. 2018;96(8):e904-e910.
- ↑ Yuan J, Zhang L-L, Lu Y-J, Han M-Y, Yu A-H, Cai X-J. Vitrectomy with internal limiting membrane peeling versus inverted internal limiting membrane flap technique for macular hole-induced retinal detachment: a systematic review of literature and meta-analysis. BMC Ophthalmol. 2017;17(1):219.
- ↑ Horiguchi M, Tanikawa A, Mizuguchi T, Tanaka H, Sugimoto M, Shimada Y. The Effect of an Inverted Internal Limiting Membrane Flap on Retinal Function after Macular Hole Surgery. Ophthalmol Retin. 2017;1(5):421-427.
- ↑ Michalewska Z, Michalewski J, Dulczewska-Cichecka K, et al. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina. 2015;35(9):1844–1850.
- ↑ Aurora A, Seth A, Sanduja N. Cabbage leaf inverted flap ILM peeling for macular hole: a novel technique. Ophthalmic Surg Lasers Imaging Retina. 2017;48(10):830–832.
- ↑ Chung CY, Wong DS, Li KK. Is it necessary to cover the macular hole with the inverted internal limiting membrane flap in macular hole surgery? A case report. BMC Ophthalmol. 2015;15:115.