Intracameral Medications Following Cataract Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Postoperative endophthalmitis is a rare but vision threatening complication of cataract surgery that is reported to occur at a highly variable rate.[1] It is associated with risk factors such as age, [2][3] male gender, [3][4][5] intraoperative posterior capsule rupture[3][4], and other ocular comorbidities. Various preventative measures are used by surgeons, most common being preoperative 5% povidone-iodine as it is supported by level 1 evidence to reduce the incidence of endophthalmitis.[6][7] In addition to topical application, different routes of antibiotic injection are also utilized, including subconjunctival, intracameral, and intravitreal. Intracameral (IC) injection, in particular, has gained its popularity as prophylaxis following an ESCRS study in 2007 that demonstrated a five-fold decrease in postoperative endophthalmitis rates with IC cefuroxime use.[8]
Survey of Current Prophylaxis Practice
Although there is increasing evidence that intracameral antibiotics are effective, considerable variation remains in antimicrobial prophylaxis without worldwide consensus. [9][10][11][12][13] While topical antibiotics use is a common practice, intracameral prophylaxis has not been universally adopted, partially due to the universal availability of a commercial formulation. [1][6][12][14][15]
Causative Microorganisms
While precise bacterial isolates may vary depending on risk factors such as age and vitreous communication,[16] the majority of endophthalmitis causing microorganisms in acute post-cataract surgery are gram-positive, with coagulase-negative staphylococci being most common. [17][18][19][20][21][22]
Other bacterial isolates from studies include Staphylococcus aureus, Streptococci, Enterococci, and Propionibacterium acnes. A study in China also found Pseudomonas species as a notable causative gram-negative organism. [18]
Routes of Medication Administration
Intracameral as adjuvant
Benefits and risks of different prophylactic antibiotic routes have been compared in multiple studies. Some studies suggest that intracameral antibiotics alone are as effective as a combined intracameral and topical approach, reducing frequency and duration of eye drops and improving compliance. [23][24] Based on a 2017 Cochrane review, high-certainty evidence supports the efficacy of intracameral cefuroxime alone with or without topical levofloxacin while moderate-certainty evidence supports a combination of topical eye drops and intracameral injection compared to either approach alone. [25]
Topical application limitations
Whether the use of long-term or short-term topical antibiotics adds any clinical benefit is questionable. [1][26][27] A 2013 Cochrane review and subsequent studies demonstrated that topical application may be less effective than intracameral injection when compared individually. [17][28] Systematic review and meta-analysis revealed no difference between topical and intracameral route on preventing endophthalmitis. [1][23]
From an economic standpoint, frequently used topical fluoroquinolone is significantly less cost-effective than using intracameral cefuroxime alone. [29]
Subconjuctival injection
The efficacy of subconjunctival injection is generally inferior to that of intracameral use according to a systematic review.[26]
A retrospective single center study in Iran showed intracameral injection has statistically lowest POE rate compared to topical or subconjunctival injection. [2]
Intravitreal injection
Intravitreal injection of combined steroid and antibiotics was first introduced by James Gills, MD and Paul Koch, MD in 2005. An advantage of intravitreal injection is that while anterior chamber has a turn-over rate of two to four hours, the vitreous cavity functions more as a deposit, releasing content over a prolonged time period.
Tri-Moxi (Triamcinolone acetonide and moxifloxacin HCl)
Tri-Moxi (Triamcinolone acetonide and moxifloxacin HCl, Imprimis Pharmaceuticals, San Diego, USA) is available in a commercially compounded form. When comparing anterior chamber cell reaction severity to standard eyedrops in a single-center retrospective longitudinal comparative study (n=1195), pars plana intravitreal injection of Tri-Moxi (containing 1mg/mL of moxifloxacine) effectively controlled intraocular inflammation and infection following cataract surgery.[30] Although the difference was not statistically significant (p=0.84), the endophthalmitis rate was reduced in the study group (0.14%) compared to the control group (0.19%). The same surgical center also reported an endophthalmitis event that resulted in severe vision loss from fluoroquinolone-resistant staphylococcus epidermidis using the same method.[31]
Tri-Moxi-Vanc (Triamocinolone acetonide, Moxifloxacin, Vancomycin)
Previously, Tri-Moxi-Vanc (Triamcinolone acetonide, Moxifloxacin, Vancomycin) intraocular solution (Imprimis Pharmaceuticals, San Diego, CA) has also been studied. A single-site prospective randomized study (n=25) by Fisher et al. showed statistically similar outcomes in post-operative IOP, central corneal thickness, and BCVA when compared transzonular vitreous Tri-Moxi-Vac injection to topical Pred-Moxi-Ketor regimen.[32]
A restrospective review (n=1429) of single-specialty ambulatory center in New Jersey by Tyson et al. evaluated its use of transzonular intravitreal Tri-Moxi-Vanc injection. Although no postoperative endophthalmitis cases were found, a topical equivalent rate of breakthrough inflammation and CME occurred.[33] However, due to reports of hemorrhagic occlusive retinal vasculitis with vancomycin use, intraocular vancomycin should be used judiciously.
Other compounded intraocular formulations
Other compounded forms that include Dexamethasone include Dex-Moxi (Dexamethasone Sodium Phosphate Moxifloxacin HCl, Imprimis Pharmaceuticals) and Dex-Moxi-Ketor (Dexamethasone Sodium Phosphate Moxifloxacin HCl Ketorolac, Imprimis Pharmaceuticals). No study has been published on their effectiveness to date.
Table 1. Intraocular Compounded Formulations
| Name | Formulations |
|---|---|
| Tri-Moxi (Imprimis Rx) | Triamcinolone acetonide 15mg and Moxifloxacin hydrochloride 1mg/mL |
| Dex-Moxi (Imprimis Rx) | Dexamethasone 1mg and Moxifloxacin 5mg/mL |
| Dex-Moxi-Ketor (Imprimis Rx) | Dexamethasone 1mg, Moxifloxcain 0.5mg, and Ketorolac 0.4mg/mL |
Complications
Toxic anterior segment syndrome and corneal endothelial toxicity are major concerns following ocular injection procedure. Any injection has potential to cause inflammation from drugs, preservatives, or other solution ingredients in addition to changes in the pH and osmolality of the anterior chamber. It is important for the antibiotic of choice to remain above MIC of causative pathogens for an appropriate duration without causing toxicity.
Intracameral Antibiotics
1. Intracameral Cefuroxime
Pharmacology
Time-dependent bactericidal effect via inhibition of cell wall synthesis. It is a broad-spectrum antibiotic that covers both gram-positive and gram-negative organisms with notable exceptions of methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant Enterococci.
Current usage
Available in a single-use commercial product called Aprokam. (Thea Pharmaceuticals, Clermont-Ferrand, France) Aprokam is a powdered solution used by dissolving in 0.9% sterile sodium chloride and is widely available in European countries but not in the US. It is a cost-saving option for hospitals with a lower risk of dilution error.[34]
Recommended dose for intracameral cefuroxime in an otherwise healthy adult is 1.0mg/0.1mL.
Efficacy
ESCRS is currently the only randomized trial studied on IC cefuroxime which demonstrated a five-fold reduction in postoperative endophthalmitis rate (n=16,603).[8]
This study, however, also recognized other important factors that concomitantly increased the infection rate including use of silicone as IOL optic material, clear corneal incision, and posterior capture rupture.
Multiple surgical centers in various countries that compared periods before and after the introduction of the 2007 ESCRS endophthalmitis study and subsequent adoption of IC cefuroxime have agreed on its efficacy through retrospective observational studies, concluding its efficacy in 2015 systematic review and meta-analysis.[1][23]
Limitations: Resistance
Continued use of IC Cefuroxime, however, may increase prevalence of resistant strains, especially Enterococci spp.[35]
Safety
Anterior chamber
IC cefuroxime has reported cases of TASS development that improved upon switching to IC moxifloxacin.[36]
A randomized controlled trial (n=129) by Lam et al. found no statically significant difference in central endothelial cell density for standard dose (1mg/ 0.1mL) compared to controls.[37]
Several other studies have also found no statistically significant endothelial cell loss or corneal damage.[38][39]
Other risks and limitations
Cakir et al. reported a case series of Fusarium endophthalmitis in 8 patients in whom compounded intracameral cefuroxime was used.[36]
Reported side effects with administration of high-dose cefuroxime include iridocyclitis, macular edema,[40][41] macular infarction,[42] retinal infarction, and retinal detachment that may or may not be transient.
Even when the dilution process is free of error, retinal toxicity may still develop sporadically.[43]
High risk patients and retinal changes
Currently published studies support the efficacy and safety of IC cefuroxime use in diabetic patients,[44] those complicated by history of keratoplasty,[45] and perioperative posterior capsular rupture. However, no randomized controlled trial has been performed to date.[46]
Adverse events are reported to occur in cataract surgeries complicated by posterior capsular rupture and anterior vitrectomy or previous vitreoretinal surgery.[47][48] Retinal changes such as transient macular edema, retinal detachment, or retinal infarction are noted in the case reports.[47][48][49][50] A randomized controlled trial (n=129) measuring retinal central point thickness showed no significant difference compared to control.[37]
On metanalysis, Bowen et al. noted ICC to be relatively safe but more prone to contamination, dilution errors, TASS, and macular toxicity compared to ICM or ICV.[23]
Cross allergenicity and hypersensitivity
Cefuroxime theoretically carries a potential to cause hypersensitivity reactions including life-threatening anaphylaxis.
In the majority of patients who self-declare to be allergic to penicillin, evidence supports use of intracameral cefuroxime prophylaxis.[51][52]
It carries low risk due to different side chains compared to penicillin, and a high rate of negative skin testing. Although rare, anaphylactic reactions have been reported to occur.[53]
2. Intracameral Moxifloxacin
Pharmacology
Concentration dependent bactericidal killing via selective bacterial topoisomerase II and IV inhibition.
As a fourth generation fluoroquinolone, moxifloxacin has a different chemical structure and mechanism of action compared to older generation fluoroquines with better gram-positive coverage and ocular penetration.[54]
It also provides coverage for gram-negative and atypical pathogens.
Current usage
Currently, Vigamox (Alcon Laboratories Inc., Fort Worth, Tx, USA) is a commercially available moxifloxacin eye drops in concentration of 0.5%. It has similar pH and osmolarity values to those of anterior chamber. It is also a preservative (benzalkonium chloride) free isotonic solution.
A single-use vial form is also available in concentration of 5mg/mL through a compounding pharmacy (Imprimis Pharmaceuticals Inc., San Diego, CA, USA).
Another less commonly used commercial product known as Moxeza had reported cases of TASS when given intracamerally due to its inactive ingredients.
Several dose concentrations have been studied with a proposed range of 150ug/ml to 500ug/ml for both safety and efficacy. [23][55]
Dosing and injection protocols
In 2019, Shorstein and Gardner proposed flushing model that would provide more consistent and sustainable anterior chamber dose delivery. [56] The model consists of injecting 0.5%/0.1mL and flushing with 0.15%/0.5ml of moxifloxicacin. Their in vitro study concluded that first injection provides enough concentration to provide adequate coverage but not long enough to cause corneal endothelial damage. Subsequent irrigating step replaces aqueous humor that may dilute the antibiotics while drug concentration in anterior chamber is sustained at intended level irrespective of AC volume.
In 2016, Arshinoff performed a retrospective review and mathematical model to conclude that final dose of 150ug/0.1ml by diluting 3ml of 0.5% Vigamox with 7ml balanced salt solution and delivering 0.3 - 0.4 ml of the diluted solution through the side port after sealing and hydrating the main incision would provide adequate concentration and duration to achieve MIC90 that produces optimal bactericidal effect. [57]
Two articles both agree on larger injection volume although proposed methods of sustaining that dose are different.
Efficacy
In India, Chang et al. conducted a high power retrospective chart review in 2016 that showed a four-fold decrease in postoperative endophthalmitis rate with IC moxifloxacin use in the Aravind Eye Care system.[58] Extended studies of Chang et al. indicated a three-fold decrease of POE in M-SICS and six-fold in phacoemulsification.[59][60]IC moxifloxacin has also been found to improve surgery outcomes of cataract surgeries complicated by PCR [59][60]or penetrating keratoplasty.[61]
The efficacy and safety of moxifloxacin has been further supported by multiple observational studies.[26][55][62]A 2019 randomized controlled study by Melegaet al. reported endophthalmitis rate of 0.05% in 1818 of studied eyes that were treated with undiluted 0.5% of IC moxifloxacin at the end of phacoemulsification.[63]Comparatively, controlled group resulted in endophthalmitis rate of 0.38%. (n=1822, p=0.035)
It has an additional advantage of relatively low MIC values for most endophthalmitis-causing bacterial pathogens.
Efficacy: resistant strains
Although moxifloxacin is a broad-spectrum antibiotic, it does not eliminate the risk completely. A case of acute endophthalmitis in immunosuppressed patients due to resistant strain of Staphylococcus epidermidis has been reported with IC moxifloxacin use. [64]
Safety
Toxic effects on anterior chambers has reported to occur at concentration greater than 500ug/mL in cultured human corneal endothelial cells. [65][66]Haruki et al. proposed that endothelial damage occurs at concentration exceeding 500ug/ml for greater than 6-24 hours and decreased cell viability at 1000ug/ml for greater than 24 hours. Several prospective studies demonstrated that IC moxifloxacin tested up to 500ug/ 0.1mL was not associated with significantly increased risk in final visual acuity, intraocular pressure, corneal thickness, corneal clarity and edema, and anterior chamber cells and flare.[23][67][68][69][70]Recently, Miyake et al. studied toxicity on human retinal vascular endothelial cells on three different antibiotics discussed. Moxifloxacin was noted to show significant increase in cell membrane damage starting at 125ug/ml (p=0.004) in a dose-dependent manner.[66]
A retrospective case review observed mild increase in macula thickness and volume. [71]
Comparing baseline to 2 years, IC moxifloxacin did not carry any significant long term risk. [72]
3. Intracameral Vancomycin
Pharmacology
Vancomycin is a bactericidal antibiotic that works by blocking cell wall synthesis, but is also bacteriostatic for at least first 6 hours.
It has good coverage of gram-positive organisms, but it is ineffective against gram-negative pathogens.
Ocular MRSA is also an increasing incidence, for which Vancomycin has excellent coverage.
Current use
Vancomycin is prepared using its powdered form to achieve a recommended dose of 1.0mg/0.1 mL.
Due to its low pH, it must be prepared with a buffer and balanced salt solution.
Any error during the compounding process has a potential to cause TASS and corneal damage.
Efficacy
Studies regarding the efficacy of IC vancomycin are lacking, including randomized controlled trial.
Some studies suggest its utility and coverage against MRSA [73]and coagulase-negative Staphylococci.[19]
Efficacy of intracameral vancomycin at reducing postoperative endophthalmitis have been supported through multiple retrospective studies.[62][74][75][76]
A 2016 review of large cohort studies by Huang et al. showed general reduction in infection rate with heterogeneity in study results while a 2015 systematic review of nonrandomized studies by Kessel et al. concluded no significant effect with very low quality of evidence. [1][26]
Safety
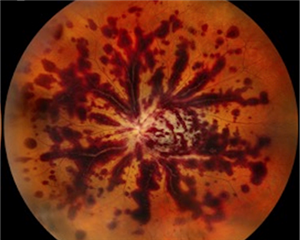
In 2017, ASCRS and ASRS formed a joint task force to identify prevalence and characteristics of hemorrhagic occlusive vascular retinitis (HORV) occurring with IC vancomycin. Investigation of 36 case reports by Witkin et al. showed association with IC vancomycin reaction while 56% developed neovascular glaucoma. [77]
Vision loss was another complication, worse with second bolus of IC vancomycin injection and better with intravitreal corticosteroid injections. 22 cases that underwent FA all showed peripheral ischemia. Hemorrhagic cases are more frequently associated with bilateral sequential cataract surgery, and PORV required several treatment approaches, including topical and systemic corticosteroids, antivirals, and early vitrectomy. The study recommended early anti-VEGF therapy and panretinal photocoagulation in addition to steroid treatment. FDA subsequently issued warning that the use of IC vancomycin is not recommended due to reported adverse events. (FDA)
The HORV task force hypothesized type III hypersensitivity reaction as the main mechanism, although recent histologic studies by Todorich et al. proposed predominantly T-cell based type IV hypersensitivity reaction. [78]
Prospective randomized controlled trials have mixed reports of effects of IC vancomycin on macular thickness. [79][80]
4. Statistical Comparison of Individual Intracameral Antibiotics
When all three antibiotics were compared in a systematic review and meta-analysis, IC cefuroxime and moxifloxacin showed both efficacy and safety at standard doses[1][23]in addition to cost-effectiveness.[81]
Efficacy
A 2018 systematic review and meta-analysis by Bowen et al. demonstrated pooled weighted averages for POE incidence for ICC, ICM, and ICV were 0.0332%, 0.0153%, and 0.0106% on moderate to high quality of evidence. High quality evidence supports use of ICC.
Arshinoff et al. generated an exponential decay model consistent with literature review and concluded that moxifloxacin as the most effective of the three with its ability to overcome resistance via dose-dependent manner. [82]
In vitro studies using bacterial isolates of endophthalmitis cases by Libre and Matthews concluded that only moxifloxacin of 3 antibiotics has coverage for all isolates and is effective against Pseudomonas. To provide effective coverage of both Staphylococcus and Pseudomonas, they recommend delivery of least 0.5mg.[83]
Safety
ICV has HORV risk, and ICM carries a risk of dilution error, contamination, TASS, and macular toxicity. [23]
Moxifloxacin is most likely to cause immediate damage to vascular endothelial cells when studied in vitro while vascular toxicity and inflammation induction were significant with in vitro injection of cefuroxime and vancomycin. [66]
Their dose-dependent toxicity on human corneal endothelial cells studied in vitro showed a narrow range of toxicity with potential to induce irreversible cell death at concentration higher than 15.0mg/mL.[84]Cell viability was significantly reduced at concentrations higher than 2.75mg/mL of cefuroxime and 5.0mg/mL of vancomycin.
Both vancomycin and cefuroxime have the potential to increase macular thickness at a comparative level, likely due to inflammation.[85]
Table 2. Summary of Current Intracameral Antibiotics Usage
| Antibiotics | Single-use Form | Other Available Forms | Dose Suggested |
|---|---|---|---|
| Cefuroxime | 50mg power (Aprokam) | 750mg powder form | 1.0mg/0.1mL |
| Moxifloxacin | 5mg/mL single-use vial (Imprimis Rx) | 0.5% Vigamox solution | 0.15-0.5mg/0.1mL |
| Vancomycin | Not available | 500mg powder form | 1.0mg/0.1mL |
5. Combination Therapy
Similar to intravitreal injection, several different combination approaches for intracameral injection have been suggested. Combined vancomycin and aminoglycoside in intracameral injections to broaden coverage has shown efficacy in a few studies. [18][86]
An in vitro study showed synergistic effects when combined intracameral cefuroxime with levofloxacin that may overcome most antibiotic-resistant strains.[87]
Enterococcus Faecalis remain difficult to combat experimentally in a combination approach.[87]
No single antibiotics covers all potential causative microorganisms.
Conclusion
Intracameral injection allows multiple benefits during cataract surgery evidenced by randomized controlled trials and meta-analysis. Of three antibiotics of choice, IC moxifloxacin seems to be the most promising when comparing POE rate and reported side effects with broad-spectrum coverage. More widely available commercial formulation is needed to adopt its use throughout countries, but there are compounding pharmacies producing combination of antibiotic/anti-inflammatory medications that appear promising. We need additional data to establish effectiveness.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Kessel L, Flesner P, Andresen J, Erngaard D, Tendal B, Hjortdal J. Antibiotic prevention of postcataract endophthalmitis: a systematic review and meta-analysis. Acta Ophthalmol. 2015;93(4):303-317.
- ↑ Jump up to: 2.0 2.1 Jabbarvand M, Hashemian H, Khodaparast M, Jouhari M, Tabatabaei A, Rezaei S. Endophthalmitis Occurring after Cataract Surgery: Outcomes of More Than 480 000 Cataract Surgeries, Epidemiologic Features, and Risk Factors. Ophthalmology. 2016;123(2):295-301.
- ↑ Jump up to: 3.0 3.1 3.2 Khanna RC, Ray VP, Latha M, Cassard SD, Mathai A, Sekhar GC. Risk factors for endophthalmitis following cataract surgery-our experience at a tertiary eye care centre in India. Int J Ophthalmol. 2015;8(6):1184-1189.
- ↑ Jump up to: 4.0 4.1 Creuzot-Garcher C, Benzenine E, Mariet AS, et al. Incidence of Acute Postoperative Endophthalmitis after Cataract Surgery: A Nationwide Study in France from 2005 to 2014. Ophthalmology. 2016;123(7):1414-1420.
- ↑ Wai YZ, Fiona Chew LM, Mohamad AS, et al. The Malaysian cataract surgery registry: incidence and risk factors of postoperative infectious endophthalmitis over a 7-year period. Int J Ophthalmol. 2018;11(10):1685-1690.
- ↑ Jump up to: 6.0 6.1 Matsuura K, Mori T, Miyamoto T, et al. Survey of Japanese ophthalmic surgeons regarding perioperative disinfection and antibiotic prophylaxis in cataract surgery. Clin Ophthalmol. 2014;8:2013-2018.
- ↑ Grabska-Liberek I, Majszyk-Ionescu J, Tesla P, Gaca-Wysocka M, Grzybowski A. Perioperative endophthalmitis prevention in cataract surgery in Mazovia and Greater Poland in 2013 and 2014. Klin Oczna. 2016;118(4):293-297.
- ↑ Jump up to: 8.0 8.1 Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978-988.
- ↑ Grzybowski A, Schwartz SG, Matsuura K, et al. Endophthalmitis Prophylaxis in Cataract Surgery: Overview of Current Practice Patterns Around the World. Curr Pharm Des. 2017;23(4):565-573.
- ↑ Haripriya A, Chang DF. Intracameral antibiotics during cataract surgery: evidence and barriers. Curr Opin Ophthalmol. 2018;29(1):33-39.
- ↑ Chang DF, Braga-Mele R, Henderson BA, Mamalis N, Vasavada A. Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: Results of the 2014 ASCRS member survey. J Cataract Refract Surg. 2015;41(6):1300-1305.
- ↑ Jump up to: 12.0 12.1 Behndig A, Cochener-Lamard B, Guell J, et al. Surgical, antiseptic, and antibiotic practice in cataract surgery: Results from the European Observatory in 2013. J Cataract Refract Surg. 2015;41(12):2635-2643.
- ↑ Schwartz SG, Grzybowski A, Flynn HW, Jr. Antibiotic prophylaxis: different practice patterns within and outside the United States. Clin Ophthalmol. 2016;10:251-256.
- ↑ Maharana PK, Chhablani JK, Das TP, Kumar A, Sharma N. All India Ophthalmological Society members survey results: Cataract surgery antibiotic prophylaxis current practice pattern 2017. Indian J Ophthalmol. 2018;66(6):820-824.
- ↑ Kelkar AS, Chang DF, Kelkar JA, Mehta HM, Lahane T, Parekh R. Antibiotic prophylaxis practice patterns for cataract surgery in India - Results from an online survey. Indian J Ophthalmol. 2017;65(12):1470-1474.
- ↑ Lundstrom M, Friling E, Montan P. Risk factors for endophthalmitis after cataract surgery: Predictors for causative organisms and visual outcomes. J Cataract Refract Surg. 2015;41(11):2410-2416.
- ↑ Jump up to: 17.0 17.1 Slean GR, Shorstein NH, Liu L, Paschal JF, Winthrop KL, Herrinton LJ. Pathogens and antibiotic sensitivities in endophthalmitis. Clin Exp Ophthalmol. 2017;45(5):481-488.
- ↑ Jump up to: 18.0 18.1 18.2 Yao K, Zhu Y, Zhu Z, et al. The incidence of postoperative endophthalmitis after cataract surgery in China: a multicenter investigation of 2006-2011. Br J Ophthalmol. 2013;97(10):1312-1317.
- ↑ Jump up to: 19.0 19.1 Lin M, Zhang W, Liu Y, et al. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital in China. J Hosp Infect. 2011;79(4):323-327.
- ↑ Li A, Shao J, Gans R, Bena J, Goshe J. Postoperative Endophthalmitis Before and After Preferred Utilization of Prophylactic Intracameral Antibiotics for Phacoemulsification Cataract Surgeries at Cole Eye Institute. Eye Contact Lens. 2019;45(5):306-309.
- ↑ Benz MS, Scott IU, Flynn HW, Jr., Unonius N, Miller D. Endophthalmitis isolates and antibiotic sensitivities: a 6-year review of culture-proven cases. Am J Ophthalmol. 2004;137(1):38-42.
- ↑ Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19(3):227-234.
- ↑ Jump up to: 23.0 23.1 23.2 23.3 23.4 23.5 23.6 23.7 Bowen RC, Zhou AX, Bondalapati S, et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018;102(9):1268-1276.
- ↑ Zhou AX, Messenger WB, Sargent S, Ambati BK. Safety of undiluted intracameral moxifloxacin without postoperative topical antibiotics in cataract surgery. Int Ophthalmol. 2016;36(4):493-498.
- ↑ Gower EW, Lindsley K, Tulenko SE, Nanji AA, Leyngold I, McDonnell PJ. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst Rev. 2017;2:Cd006364.
- ↑ Jump up to: 26.0 26.1 26.2 26.3 Huang J, Wang X, Chen X, Song Q, Liu W, Lu L. Perioperative Antibiotics to Prevent Acute Endophthalmitis after Ophthalmic Surgery: A Systematic Review and Meta-Analysis. PLoS One. 2016;11(11):e0166141.
- ↑ Tuni-Picado J, Martinez-Palmer A, Fernandez-Sala X, et al. Infectious postoperative endophthalmitis after cataract surgery performed over 7 years. The role of azithromycin versus ciprofloxacin eye drops. Rev Esp Quimioter. 2018;31(6):15-21.
- ↑ Gower EW, Lindsley K, Nanji AA, Leyngold I, McDonnell PJ. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst Rev. 2013(7):Cd006364.
- ↑ Sharifi E, Porco TC, Naseri A. Cost-effectiveness analysis of intracameral cefuroxime use for prophylaxis of endophthalmitis after cataract surgery. Ophthalmology. 2009;116(10):1887-1896.e1881.
- ↑ Nassiri S, Hwang FS, Kim J, et al. Comparative analysis of intravitreal triamcinolone acetonide-moxifloxacin versus standard perioperative eyedrops in cataract surgery. J Cataract Refract Surg. 2019;45(6):760-765.
- ↑ Ng C, Chalam KV. Endophthalmitis after dropless (Tri-Moxi injection) cataract surgery. Eur J Ophthalmol. 2019:1120672119852505.
- ↑ Fisher BL, Potvin R. Transzonular vitreous injection vs a single drop compounded topical pharmaceutical regimen after cataract surgery. Clin Ophthalmol. 2016;10:1297-1303.
- ↑ Tyson SL, Bailey R, Roman JS, Zhan T, Hark LA, Haller JA. Clinical outcomes after injection of a compounded pharmaceutical for prophylaxis after cataract surgery: a large-scale review. Curr Opin Ophthalmol. 2017;28(1):73-80.
- ↑ Purslow C, Davey K, Johnson M, Pietri G, Suri G. Budget impact assessment of Aprokam(R) compared with unlicensed cefuroxime for prophylaxis of post-cataract surgery endophthalmitis. BMC Ophthalmol. 2015;15:72.
- ↑ Friling E, Montan P. Bacteriology and cefuroxime resistance in endophthalmitis following cataract surgery before and after the introduction of prophylactic intracameral cefuroxime: a retrospective single-centre study. J Hosp Infect. 2019;101(1):88-92.
- ↑ Jump up to: 36.0 36.1 Cakir B, Celik E, Aksoy NO, et al. Toxic anterior segment syndrome after uncomplicated cataract surgery possibly associated with intracamaral use of cefuroxime. Clin Ophthalmol. 2015;9:493-497.
- ↑ Jump up to: 37.0 37.1 Lam PT, Young AL, Cheng LL, Tam PM, Lee VY. Randomized controlled trial on the safety of intracameral cephalosporins in cataract surgery. Clin Ophthalmol. 2010;4:1499-1504.
- ↑ Shahraki K, Fard MNA, Shahri F, et al. Effects of intracameral cefuroxime on corneal endothelial cell counts and its morphology after cataract surgery. Interv Med Appl Sci. 2017;9(2):100-104.
- ↑ Montan PG, Wejde G, Setterquist H, Rylander M, Zetterstrom C. Prophylactic intracameral cefuroxime. Evaluation of safety and kinetics in cataract surgery. J Cataract Refract Surg. 2002;28(6):982-987.
- ↑ Delyfer MN, Rougier MB, Leoni S, et al. Ocular toxicity after intracameral injection of very high doses of cefuroxime during cataract surgery. J Cataract Refract Surg. 2011;37(2):271-278.
- ↑ Wong DC, Waxman MD, Herrinton LJ, Shorstein NH. Transient macular edema after intracameral injection of a moderately elevated dose of cefuroxime during phacoemulsification surgery. JAMA Ophthalmol. 2015;133(10):1194-1197.
- ↑ Qureshi F, Clark D. Macular infarction after inadvertent intracameral cefuroxime. J Cataract Refract Surg. 2011;37(6):1168-1169.
- ↑ Zuo C, Mi L, Ye D, et al. Toxic retinopathy after phacoemulsification when the cefuroxime dilution is correct. J Cataract Refract Surg. 2018;44(1):28-33.
- ↑ Ma B, Liu Y, Liu S, Luo M. Evaluation of the effect of intracameral cefuroxime on macular and subfoveal choroidal thickness and macular sensitivity in diabetic patients after cataract surgery. J Cataract Refract Surg. 2017;43(2):201-206.
- ↑ Cicik ME, Dogan C, Arslan OS. Effect of Intracameral Ophthalmic Cefuroxime Solution (Aprokam((R))) in the Prophylaxis of Cataract Surgery in Patients with Keratoplasty. Balkan Med J. 2018;35(2):181-185.
- ↑ Daien V, Papinaud L, Gillies MC, et al. Effectiveness and Safety of an Intracameral Injection of Cefuroxime for the Prevention of Endophthalmitis After Cataract Surgery With or Without Perioperative Capsular Rupture. JAMA Ophthalmol. 2016;134(7):810-816.
- ↑ Jump up to: 47.0 47.1 Bryan EA, Cruz-Inigo YJ, Brems RN, Bryan JS. ACUTE MACULAR EDEMA WITH SEROUS RETINAL DETACHMENT AFTER CATARACT SURGERY IN A VITRECTOMIZED EYE: A CASE REPORT. Retin Cases Brief Rep. 2019.
- ↑ Jump up to: 48.0 48.1 Sul S, Karalezli A. Development of Retinal Infarct Due to Intracameral Cefuroxime Injection Following Complicated Cataract Surgery. Turk J Ophthalmol. 2018;48(6):317-319.
- ↑ Xiao H, Liu X, Guo X. Macular edema with serous retinal detachment post-phacoemulsification followed by spectral domain optical coherence tomography: a report of two cases. BMC Res Notes. 2015;8:647.
- ↑ Mesnard C, Beral L, Hage R, Merle H, Fares S, David T. Endophthalmitis after cataract surgery despite intracameral antibiotic prophylaxis with licensed cefuroxime. J Cataract Refract Surg. 2016;42(9):1318-1323.
- ↑ Promelle V, Jany B, Drimbea A, Jezraoui P, Milazzo S. Tolerability of intracameral cefuroxime during cataract surgery in case of penicillin allergy. J Fr Ophtalmol. 2015;38(4):283-287.
- ↑ Al-Abduljabbar KA, Stone DU. Risks of Cefuroxime Prophylaxis for Postcataract Endophthalmitis. Middle East Afr J Ophthalmol. 2017;24(1):24-29.
- ↑ Villada JR, Vicente U, Javaloy J, Alio JL. Severe anaphylactic reaction after intracameral antibiotic administration during cataract surgery. J Cataract Refract Surg. 2005;31(3):620-621.
- ↑ Thompson AM. Ocular toxicity of fluoroquinolones. Clin Exp Ophthalmol. 2007;35(6):566-577.
- ↑ Jump up to: 55.0 55.1 Matsuura K, Suto C, Akura J, Inoue Y. Comparison between intracameral moxifloxacin administration methods by assessing intraocular concentrations and drug kinetics. Graefes Arch Clin Exp Ophthalmol. 2013;251(8):1955-1959.
- ↑ Shorstein NH, Gardner S. Injection volume and intracameral moxifloxacin dose. J Cataract Refract Surg. 2019;45(10):1498-1502.
- ↑ Arshinoff SA, Modabber M. Dose and administration of intracameral moxifloxacin for prophylaxis of postoperative endophthalmitis. J Cataract Refract Surg. 2016;42(12):1730-1741.
- ↑ Haripriya A, Chang DF, Namburar S, Smita A, Ravindran RD. Efficacy of Intracameral Moxifloxacin Endophthalmitis Prophylaxis at Aravind Eye Hospital. Ophthalmology.2016;123(2):302-308.
- ↑ Jump up to: 59.0 59.1 Haripriya A, Chang DF, Ravindran RD. Endophthalmitis Reduction with Intracameral Moxifloxacin Prophylaxis: Analysis of 600 000 Surgeries. Ophthalmology.2017;124(6):768-775.
- ↑ Jump up to: 60.0 60.1 Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: Results from 2 million consecutive cataract surgeries. J Cataract Refract Surg. 2019;45(9):1226-1233.
- ↑ Arslan OS, Arici C, Unal M, Cicik E, Mangan MS, Atalay E. Safety of prophylactic intracameral moxifloxacin ophthalmic solution after cataract surgery in patients with penetrating keratoplasty. Int J Ophthalmol. 2014;7(5):795-799.
- ↑ Jump up to: 62.0 62.1 Rudnisky CJ, Wan D, Weis E. Antibiotic choice for the prophylaxis of post-cataract extraction endophthalmitis. Ophthalmology. 2014;121(4):835-841.
- ↑ Melega MV, Alves M, Cavalcanti Lira RP, et al. Safety and efficacy of intracameral moxifloxacin for prevention of post-cataract endophthalmitis: Randomized controlled clinical trial. J Cataract Refract Surg. 2019;45(3):343-350.
- ↑ Chang VS, Schwartz SG, Davis JL, Flynn HW, Jr. Endophthalmitis following cataract surgery and intracameral antibiotic: Moxifloxacin resistant Staphylococcus epidermidis. Am J Ophthalmol Case Rep. 2019;13:127-130.
- ↑ Haruki T, Miyazaki D, Matsuura K, et al. Comparison of toxicities of moxifloxacin, cefuroxime, and levofloxacin to corneal endothelial cells in vitro. J Cataract Refract Surg. 2014;40(11):1872-1878.
- ↑ Jump up to: 66.0 66.1 66.2 Miyake H, Miyazaki D, Shimizu Y, et al. Toxicities of and inflammatory responses to moxifloxacin, cefuroxime, and vancomycin on retinal vascular cells. Sci Rep. 2019;9(1):9745.
- ↑ Lane SS, Osher RH, Masket S, Belani S. Evaluation of the safety of prophylactic intracameral moxifloxacin in cataract surgery. J Cataract Refract Surg. 2008;34(9):1451-1459.
- ↑ Ekinci Koktekir B, Aslan BS. Safety of prophylactic intracameral moxifloxacin use in cataract surgery. J Ocul Pharmacol Ther. 2012;28(3):278-282.
- ↑ Lucena NP, Pereira IMS, Gaete MIL, Ferreira KSA, Melega MV, Lira RPC. Intracameral moxifloxacin after cataract surgery: a prospective study. Arq Bras Oftalmol. 2018;81(2):92-94.
- ↑ Espiritu CR, Caparas VL, Bolinao JG. Safety of prophylactic intracameral moxifloxacin 0.5% ophthalmic solution in cataract surgery patients. J Cataract Refract Surg. 2007;33(1):63-68.
- ↑ Arbisser LB. Safety of intracameral moxifloxacin for prophylaxis of endophthalmitis after cataract surgery. J Cataract Refract Surg. 2008;34(7):1114-1120.
- ↑ Cavalcanti Lira RP, Lucena NP, Ferreira KS, Santos BM. Long-term safety of intracameral moxifloxacin after cataract surgery. J Cataract Refract Surg. 2017;43(1):139-140.
- ↑ Libre PE, Della-Latta P, Chin NX. Intracameral antibiotic agents for endophthalmitis prophylaxis: a pharmacokinetic model. J Cataract Refract Surg. 2003;29(9):1791-1794.
- ↑ Rush SW, Vu D, Rush RB. The Safety and Efficacy of Routine Administration of Intracameral Vancomycin during Cataract Surgery. J Ophthalmol. 2015;2015:813697.
- ↑ Au CP, White AJ, Healey PR. Efficacy and cost-effectiveness of intracameral vancomycin in reducing postoperative endophthalmitis incidence in Australia. Clin Exp Ophthalmol. 2016;44(9):803-811.
- ↑ Anijeet DR, Palimar P, Peckar CO. Intracameral vancomycin following cataract surgery: An eleven-year study. Clin Ophthalmol. 2010;4:321-326.
- ↑ Witkin AJ, Chang DF, Jumper JM, et al. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: Clinical Characteristics of 36 Eyes. Ophthalmology.2017;124(5):583-595.
- ↑ Todorich B, Faia LJ, Thanos A, et al. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: A Clinical-Pathophysiological Analysis. Am J Ophthalmol. 2018;188:131-140.
- ↑ Ball JL, Barrett GD. Prospective randomized controlled trial of the effect of intracameral vancomycin and gentamicin on macular retinal thickness and visual function following cataract surgery. J Cataract Refract Surg. 2006;32(5):789-794.
- ↑ Axer-Siegel R, Stiebel-Kalish H, Rosenblatt I, Strassmann E, Yassur Y, Weinberger D. Cystoid macular edema after cataract surgery with intraocular vancomycin. Ophthalmology. 1999;106(9):1660-1664.
- ↑ Linertova R, Abreu-Gonzalez R, Garcia-Perez L, et al. Intracameral cefuroxime and moxifloxacin used as endophthalmitis prophylaxis after cataract surgery: systematic review of effectiveness and cost-effectiveness. Clin Ophthalmol. 2014;8:1515-1522.
- ↑ Arshinoff SA, Felfeli T, Modabber M. Aqueous level abatement profiles of intracameral antibiotics: A comparative mathematical model of moxifloxacin, cefuroxime, and vancomycin with determination of relative efficacies. J Cataract Refract Surg. 2019;45(11):1568-1574.
- ↑ Libre PE, Mathews S. Endophthalmitis prophylaxis by intracameral antibiotics: In vitro model comparing vancomycin, cefuroxime, and moxifloxacin. J Cataract Refract Surg. 2017;43(6):833-838.
- ↑ Yoeruek E, Spitzer MS, Saygili O, et al. Comparison of in vitro safety profiles of vancomycin and cefuroxime on human corneal endothelial cells for intracameral use. J Cataract Refract Surg. 2008;34(12):2139-2145.
- ↑ Perez-Canales JL, Perez-Santonja JJ, Campos-Mollo E. Evaluation of macular thickness changes after intracameral vancomycin in cataract surgery. Int Ophthalmol. 2015;35(1):49-57.
- ↑ Beigi B, Westlake W, Chang B, Marsh C, Jacob J, Riordan T. The effect of intracameral, per-operative antibiotics on microbial contamination of anterior chamber aspirates during phacoemulsification. Eye (Lond). 1998;12 ( Pt 3a):390-394.
- ↑ Jump up to: 87.0 87.1 Suzuki T, Yamamoto T, Torikai T, Ohashi Y. Combination Effect of Cefuroxime and Levofloxacin Against Bacteria Isolated from the Healthy Conjunctival Sac and Endophthalmitis Cases Using a Fractional Inhibitory Concentration Index. J Ocul Pharmacol Ther. 2017;33(1):19-23.