Internuclear Ophthalmoplegia of Abduction (Lutz Posterior INO)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Internuclear ophthalmoplegia (INO) of abduction (also known as “Lutz posterior INO”, “reverse INO”, or "pseudo abducens palsy") is a rare horizontal gaze palsy that can be either unilateral or bilateral. It is an examination finding where the patient exhibits ABduction limitation and contralateral ADduction nystagmus.[1] This is the “reverse” of a typical internuclear ophthalmoplegia with ADduction limitation and contralateral ABduction nystagmus. The location of the lesion resulting in INO of abduction is highly debated.
Disease
ICD-9 378.86 Internuclear ophthalmoplegia
ICD-10 H51.2 Internuclear ophthalmoplegia
Etiology
A lesion along the horizontal gaze pathway.
Risk Factors
Risk factors depend on the specific etiologies listed above.
Pathophysiology
Lutz first described a case of INO of abduction in 1923.[2] Although his hypothesis that supranuclear fibers in the pons divide to innervate the ipsilateral medial rectus and the contralateral lateral rectus is now known to be untrue, the clinical sign of a reverse INO has clearly been described. Lutz termed his reverse INO a "posterior INO", as he thought the "posterior" supranuclear fibers traveled to the lateral rectus muscle.[3] Kommerell suggested the more specific term "internuclear ophthalmoplegia of abduction" in 1975.[4] This is not to be confused with Cogan's anterior and posterior INO, which refer to an anterior midbrain or posterior pontine localization along the medial longitudinal fasciculus (MLF). [1]
The INO of abduction has two components. The first component is an ABduction limitation due to abducens weakness. It is debated if this limitation localizes relative to the abducens nerve, i.e. pre-nuclear, nuclear, fascicular or internuclear. Cases of reverse INO have been localized to the paramedian pontine rostral formation (PPRF),[5] pre-nuclear rostral pons,[6] abducens fasiculus,[7][8] pontine MLF,[9] and midbrain.[9] Localization has been achieved by post-mortem pathology with immunostaining, neuroimaging demonstrating a distinct lesion, and a combination of imaging and brainstem electrophysiology studies.[5][6][7][8][9] The second component is a contralateral ADduction nystagmus. The etiology of this nystagmus is unclear but could be due to increased signaling to the yoked contralateral medial rectus after ipsilateral lateral rectus weakness, as proposed in reverse for a typical INO.[10]
Depending on the location of the INO of abduction lesion, convergence may be preserved or impaired. Along the lines of Cogan's classification for typical INO, anterior midbrain lesions in proximity to the oculomotor fibers will impair convergence, while posterior pontine lesions will spare convergence.[1]
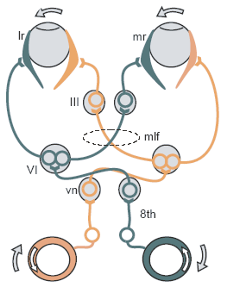
Figure 1. Horizontal gaze pathway. III, 3rd cranial nerve (oculomotor) nucleus); LR, lateral rectus muscle; MLF, medial longitudinal fasciculus; MR, medial rectus muscle; VI, 6th cranial nerve (abducens) nucleus; VN, 8th cranial nerve (vestibular) nucleus; 8th, vestibular neve.
Diagnosis
The diagnosis is made clinically.
Symptoms
The patient may complain of blurry vision or binocular horizontal diplopia.
Clinical diagnosis
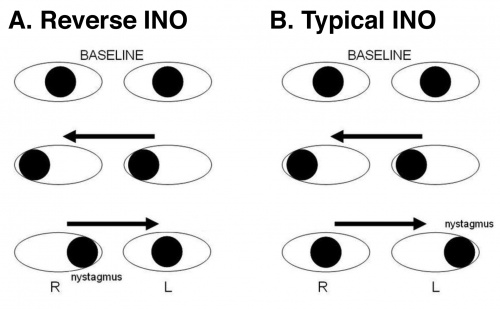
When examining for horizontal saccades by asking the patient to look rapidly between two targets at opposite sides of their horizontal peripheral field, the patient will exhibit deficit of ABduction and a contralateral slow ADduction nystagmus (Figure 2A). This is the opposite, or reverse, of a typical INO, where the patient exhibits limitation of ADduction and contralateral slow ABduction nystagmus (Figure 2B). The INO of abduction can be unilateral or bilateral.
Figure 2. Comparison between reverse INO and typical INO (adapted from [11])
Diagnostic procedures
A brain magnetic resonance imaging may be indicated to further elucidate the etiology.
Differential diagnosis
The most likely causes for an INO of abduction are stroke, demyelinating disease, neoplasm and myasthenia gravis.
The complete differential diagnosis to consider includes causes of typical INO, as follows:[12]
- Stroke
- Multiple sclerosis
- Other:
- Head trauma
- Cerebral herniation
- Infection (HIV, cysticercosis, syphilis, meningitis, sepsis, brucellosis)
- Tumors (medulloblastoma, pontine glioma, lymphoma, epidermoid, ganglioglioma, metastasis)
- Post-surgical/-procedural (tumor excision, aneurysm clipping, cavernous angioma removal)
- Brainstem hemorrhage (hypertension, cavernous angioma, arteriovenous malformation, bleeding diathesis)
- Vasculitis (e.g. system lupus erythematosus)
Management
There is no specific treatment for the INO of abduction itself. The underlying disease should be worked up and managed appropriately. For symptomatic diplopia, treatment options include fogging one glasses lens, patching one eye, a Fresnel prism or ground-in prism glasses, or strabismus surgery.[13]
Prognosis
Little is documented regarding the prognosis of INO of abduction, due to it's rare presentation. Typical INO due to ischemia is expected to resolve on the order of 2-3 months,[14] similar to other vascular cranial neuropathies causing external ophthalmoplegia. INO due to ischemia, multiple sclerosis or infection can spontaneously resolve over 3-9 months, however it has been described to persist for greater than 12 months.[15]
References
- ↑ 1.0 1.1 1.2 Zee DS, Newman-Toker D. Walsh & Hoyt's Clinical Neuro-Ophthalmology, 6th Edition, Chapter 19 Supranuclear and Internuclear Ocular Motility Disorders. Philadephia: Lippincott Williams & Wilkins, Philadelphia, 2005. Print.
- ↑ Lutz A. Ueber die Bahnen der Blickwendung und deren Dissoziierung. Klin Monatsble Augenheilkd 1923;70:213-35.
- ↑ Thomke F, Hopf HC, Kramer G. Internuclear ophthalmoplegia of abduction: clinical and electrophysiological data on the existence of an abduction paresis of prenuclear origin. J Neurol Neurosurg Psychiatry 1992;55:105-11.
- ↑ Kommerell G. Internuclear ophthalmoplegia of abduction. Isolated impairment of phasic ocular motor activity in supranuclear lesions. Arch Ophthalmol 1975;93:531-4.
- ↑ 5.0 5.1 Bogousslavsky J, Regli F, Ostinelli B, Rabinowicz T. Paresis of lateral gaze alternating with so-called posterior internuclear ophthalmoplegia. A partial paramedian pontine reticular formation-abducens nucleus syndrome. J Neurol. 1985;232(1):38-42.
- ↑ 6.0 6.1 Rothstein TL, Alvord EC, Jr. Posterior internuclear ophthalmoplegia. A clinicopathological study. Arch Neurol 1971;24:191-202.
- ↑ 7.0 7.1 Oliveri RL, Bono F, Quattrone A. Pontine lesion of the abducens fasciculus producing so-called posterior internuclear ophthalmoplegia. Eur Neurol 1997;37:67-9.
- ↑ 8.0 8.1 Wiest G, Wanschitz J, Baumgartner C, Trattnig S, Deecke L, Mueller C. So-called posterior internuclear ophthalmoplegia due to a pontine glioma: a clinicopathological study. J Neurol. 1999 May;246(5):412-5.
- ↑ 9.0 9.1 9.2 Thömke F, Hopf HC. Abduction paresis with rostral pontine and/or mesencephalic lesions: Pseudoabducens palsy and its relation to the so-called posterior internuclear ophthalmoplegia of Lutz. BMC Neurol. 2001 Dec 18;1:4.
- ↑ Zee DS, Hain TC, Carl JR. Abduction nystagmus in internuclear ophthalmoplegia. Ann Neurol 1987;21:383-8.
- ↑ https://en.wikipedia.org/wiki/Internuclear_ophthalmoplegia
- ↑ Keane JR. Internuclear ophthalmoplegia: unusual causes in 114 of 410 patients. Arch Neurol. 2005 May;62(5):714-7.
- ↑ Fraine L. Nonsurgical management of diplopia. Am Orthopt J. 2012;62:13-8.
- ↑ Eggenberger E, Golnik K, Lee A, Santos R, Suntay A, Satana B, Vaphlades M, Stevens C, Kaufman D, Wall M, Kardon R. Prognosis of ischemic internuclear ophthalmoplegia. Ophthalmology. 2002 Sep;109(9):1676-8.
- ↑ Bolaños I, Lozano D, Cantú C. Internuclear ophthalmoplegia: causes and long-term follow-up in 65 patients. Acta Neurol Scand. 2004 Sep;110(3):161-5.

