Infraorbital Rim/Tear Trough Implants in Context of Thyroid Eye Disease/Prominent Globe
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Thyroid eye disease (TED) is considered a chronic inflammatory and autoimmune condition. TED is the most common orbital disease in North America. It is highly associated with hyperthyroidism, yet there have been documented cases of TED in patients with Hashimoto’s thyroiditis as well as patients with euthyroidism. The onset of TED can occur before, concurrently, or as an effect of thyroid dysfunction disorders.[1] In cases of hyperthyroidism, onset of TED is most likely to occur at the same time as onset of hyperthyroidism, but it can also present a year before onset or up to five years after onset of hyperthyroidism.[2]
Disease
Anatomy
Graves’ hyperthyroidism is caused by autoantibodies that bind to the thyrotropic receptor on endothelial cells of thyroid follicles, which stimulates excess production of thyroid hormone. This subsequently causes a loss of tolerance to thyroid stimulating hormone receptors (TSHR). Almost all patients with thyroid eye disease have anti-thyrotropin-receptor antibodies that cause immunoreactivity against the thyrotropin receptor.[3] High levels of the growth factor IGF-1 has also been linked to thyroid dysregulation. In a disease-free patient, synergistic activation of TSHR and IGF-1R (receptor for growth factor IGF-1) promotes DNA synthesis and thyroid cell proliferation. Yet when there is overactivation of IGF-1 levels, lowering TSH can help maintain normal thyroid function. Conversely, low levels of IGF-1 have been associated with impaired thyroid hormone secretion. A recent study confirms this, with findings that show an IGF-1R blocking drug can reduce TED disease activity.
The inflammation that causes TED begins with an infiltration of lymphocytes to the extraocular muscles and retro-ocular connective tissue.[4] The subsequent cytokine activation and secretion of glycosaminoglycans by orbital fibroblasts leads to interstitial edema, ultimately resulting in volume expansion of extraocular muscles, retro-orbital fat, and connective tissue. This can cause anterior displacement of the globe causing exophthalmos and lower lid retraction. Additionally, the edematous extraocular muscles lose compliance and can compress the optic nerve at the orbital apex, leading to compressive optic neuropathy. Impaired lid closure and corneal ulceration are other likely consequences.
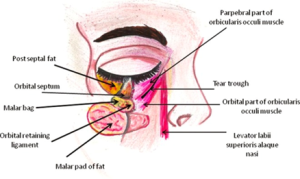
The tear trough refers to the medial one third of the periorbital hollow under the globe of the eye.[5] It forms in the depression of the orbicularis oculi muscle of the lower eyelid, which attaches to the inferior orbital rim. The area begins medially at the inferior orbital rim and increases in vertical distance laterally until it reaches a maximum vertical distance under the center of the globe, after which the vertical distance decreases till the lateral endpoint of the inferior orbital rim.The tear trough ends where the thin skin under the eyelid meets the thicker nasal and cheek skin below it. The thinner skin under the eyelid is typically also a different color, texture, and opacity as compared to the reminder of the skin on the face.
A tear trough deformity (TTD) is a natural consequence to change in the periorbital tissue. It presents as a sunken in appearance of the globe of the eye, creating a dark shadow over the lower eyelid that creates or further highlights dark circles under the eyes. Periorbital volume loss is the single largest contributor to a TTD. It is also theorized that, with increasing age, the orbital septum becomes attenuated and fat herniates through the palpebral orbicularis to create the TTD.[6] Ptosis, prolapse of nasal fat pad or pockets, skin laxity, decreasing thickness of skin under the eyes, prominent subcutaneous venous pooling, and hyperpigmentation can all enhance the periorbital darkening.
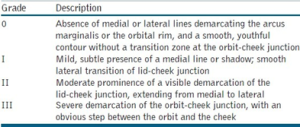
The various types of TTDs are typically classified by increasing severity. Barton et al. proposed the following grading system based on a patient’s anatomy (Table 1).
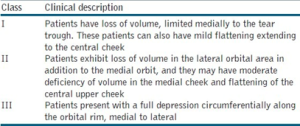
A paper published by Haideh Hirmand classified the TTD based on clinical evaluation of the patient (Table 2).
Diagnosis
General Pathology/Symptoms
Early symptoms of TED include double vision, especially at the extreme ends of the gaze, retro-orbital ache, blurred vision that does not improve upon blinking, excessive lacrimation, photophobia, dry and gritty ocular sensation, and an altered periocular appearance. Specifically, eyelid retraction and restricted eye movements, due to the edematous extraocular muscles as mentioned above, can be used to diagnose TED. Patients below the age of 40 tend to have fat expansion, while patients above the age of 60 tend to have more extraocular muscle-related swelling.[3]
Diagnosis of Lid Retraction, Exophthalmos, and Exposure Keratopathy Linked to TED
The diagnosis of thyroid eye disease typically involves a thorough medical history and physical examination, including a detailed evaluation of the eyes and eyelids. Laboratory tests are primarily utilized to evaluate thyroid function in the context of thyroid eye disease. Patients experience a variety of symptoms, but the most common include ocular discomfort, lacrimation, dry eye, redness, photophobia, orbital pain, diplopia, and refractive errors. With a physical examination, lagophthalmos, upper and/or lower lid retraction, and exophthalmos may be visualized as well.[8]
Imaging studies such as CT scans and MRI may also be used to evaluate the extent of the disease. One of the most key features noted on imaging includes hypertrophy of orbital fat and enlargement and inflammation of extraocular muscles may be noted. In patients with thyroid eye disease who have developed hollowing or volume loss in the infraorbital region, imaging may reveal a decrease in the volume of the anterior maxillary sinus and a change in the position of the orbital fat pads. This hollow and sunken feature can often be associated with an aged or tired appearance.
Furthermore, imaging studies aid in identifying changes to the orbital bones. To measure globe to orbital rim changes more specifically, a physician may use the Hertel Exophthalmometer to measure the projection from the anterior surface of the cornea beyond the lateral rim. However, measurements can be quite variable due to natural differences in skull morphology, ethnicity, sex, and age. Specifically with age, the infraorbital rim begins to move posteriorly as the cheek mass moves from an anterior projection to the cornea to a more posterior position. This movement can be attributed to an increased look of prominence in the eyes.[9]
Management
Medical Therapy
Medical treatment methods for patients with thyroid eye disease varies based upon the disease stage, ranging from mild, moderate, severe, and refractory. However, fundamental to all stages of disease is achieving well-controlled thyroid hormone levels to prevent progressing ophthalmological complications.
For the active inflammatory phase, supportive interventions such as artificial tears and topical anti-inflammatories are helpful to modulate symptoms. Subsequently, lubricants specifically for resulting lid retraction, nocturnal ointments for lagophthalmos, prisms for diplopia, and botulinum toxin injections for upper-lid retraction can be utilized effectively to alleviate extraocular presentations of TED.[10] Most importantly, most medical therapy options such as orbital radiation therapy are indicated to reduce inflammation and slow progression of disease, but may not be as effective in restoring volume or contour to the infraorbital region. Consequently, in conjunction with medications, advancements in oculoplastic surgical techniques have been a recent focus to work on improving cosmetic consequences from thyroid eye disease in the infraorbital region.
Procedures and Surgical Treatment
In patients with thyroid eye disease who have developed infraorbital rim defects, surgical intervention may be required to restore volume and contour to the affected area. Infraorbital rim implants can be utilized to augment the bone and soft tissue of the infraorbital rim, improving the appearance of the region and reducing consequential hollowing from the disease. While mostly an elective surgery, this can help to create a more youthful and vibrant appearance for patients. Occasionally, the restoration of volume can be achieved by using dermal filler injections or a fat transfer procedure. Infraorbital rim implants are often combined with customized cosmetic orbital decompression and lower eyelid retraction surgery with canthoplasty.[11] However, it is important to highlight that surgical procedures are most effective when the active phase of thyroid eye disease has subsided and the patient has been in the stable, chronic fibrotic stage for a minimum of six months.[12]
Fillers
According to a multispecialty consensus recommendation article, the tear trough is the most challenging area of the face to treat with HA. As such, many techniques are currently in place to insert filler and reduce the appearance of tear trough deformities. The consensus group technique to treat tear trough deformity with HA is the Vertical Supraperiosteal Depot Technique (VDST).
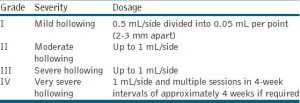
VSDT places small depots of soft tissue filler via a vertical injection on the periosteum. Due to bony support, little material is needed for pronounced correction on the skin, and VSDT is used to avoid overcorrection. Most of the filler should be injected underneath the orbicularis oculi, at the supraperiosteal level along or below the orbital rim or both. It is important to note, that the medical orbicularis oculi will require direct injection to the muscle itself. The needle should be placed perpendicular to the skin with entry points at the lateral and, if required, the medial canthus. This technique allows retrograde linear threading along the orbital rim, and ultimately, a deep injection. The amount of filler is dependent on the grade of deformity severity.[7]


Fat Grafts
The use of fat grafting in patients has gained popularity due to the ease of harvest and ready availability in most patients.[6] Further, the absence of implanting foreign material in the body can be an attractive option. The procedure can be either performed with liposuction or direct surgical placement with open surgical techniques for lower eyelid rejuvenation. When performing liposuction, an 18 to 19 gauge cannula should be used. The cannula will be attached to a 1-mL syringe for transfer, introduced into the lower lid via a stab incision, and camouflage with the natural crease in the “crows” feet area. To maximize safety and minimize complications, injection sizes of 1 mL or less should be used, although there is reference to 3 mL per side being described. Injections should be laid medial to lateral in the lower eyelid within the supraperiosteal plane. It is important to ensure there is no overcorrection of the deformity to avoid contour irregularities.
Infraorbital Rim Implants
Implants can be made from a variety of materials, including silicone, polyethylene, or PEEK (polyetheretherketone). The choice of the material and size of the implant will depend on the patient’s individual anatomy and aesthetic goals. Silicone is an alloplastic that is very commonly used for the wide array of advantages it brings. Silicone is highly pliable and soft, which allows for easy shaping and customization to the patient’s facial anatomy.[13] It is also noted to be durable, long-lasting, and biocompatible for lower rates of allergic or inflammatory reactions. However, notable disadvantages are the possible shifting that may occur if not properly secured, and more difficult to remove if revision surgery is needed.
Polyethylene (Medpor) implants have also been used as it is lightweight, easily shaped in the contour of the patient’s facial anatomy, and often has been recognized for its fast recovery time and reliability.[14] Furthermore, it is biocompatible and allows for tissue ingrowth to anchor the implant in place. A few studies have also allowed the implant to rest on the infraorbital rim by fixing it with biodegradable screws.[15] This could make the polyethylene implant more difficult to remove.
Gore-Tex has also been utilized as material for an infraorbital rim implant because of its soft, pliable, and flexible characteristics that allow the surgeon to achieve a more natural facial contour. It has also been known for its ease of use during surgery. However, disadvantages include being prone to shifts, and higher possibility for infection from making a larger incision.
Lastly, PolyEtherEtherKetone (PEEK) implants have been presented as an innovative solution in facial aesthetic plastic surgery, most particularly in improving volume and malar shape. This material is known for its strength and rigidity to improve the structural support of the infraorbital region. In recent case reports, bone-anchored PEEK implants have been utilized as a means of augmenting the malar region and altering its shape through the use of both skeletal and soft tissue camouflage.[16] However, the structural rigidity could be noted as a possible disadvantage for surgeons to adjust to a patient’s natural facial contour during surgical implantation.
There are various techniques used by surgeons to place infraorbital rim implants for patients with thyroid eye disease, including a transconjunctival, subciliary, transcutaneous, and endoscopic approach.
More specifically, the transconjunctival approach involves making an incision on the inside of the lower eyelid to allow the surgeon to access the infraorbital rim. This technique has become highly popularized because the lack of sutures is faster, has lower complication rates, results in decreased damage to eyelid function and eye shape, and entails minimal scarring.[17] This method has also been known to have a relatively faster healing time. Furthermore, the subciliary approach involves making an incision just below the lower eyelashes to insert the implant, which provides greater access and visibility compared with the transconjunctival approach. However, the subciliary incision would potentially leave a visible scar and often leads to lower lid retraction.[18] The subcutaneous approach involves making an incision below the eyelashes, extending horizontally toward the temples, which gives greater access to the infraorbital rim and surrounding tissues, but also leaves a visible scar.[19] Lastly, an endoscopic approach would involve a small camera being used to access the infraorbital rim through small incisions in the scalp or inside of the patient’s mouth.[19] This allows for a minimization of scarring and provides greater precision and control during the procedure. However, this does involve a higher risk of complications during the procedure.
Complications
In regards to fillers, the immediate complications following procedures are pain, erythema, swelling and bruising, asymmetry, and migraine. Delayed complications can include orange-brown staining of the skin, postinflammatory hyperpigmentation, puffiness due to overcorrection, rare infections, the tyndall effect, nodules, and blindness. To ensure proper management of fillers, it is important for patients to avoid strong or extended pressure to the treated area; avoid massaging, strenuous activity, and extreme temperatures up to 6-hours post treatment; and schedule follow-up sessions to assess clinical results.[7]
The complications and hesitations around fat grafting for tear trough deformity can be related to unpredictable resorption rates, frequent requirement of multiple procedures, and the risk of permanent contour irregularities. To reduce complications, treatments with massage; direct excision suctioning; and injection of steroids, phosphatidylcholine, or deoxycholate for cases of contour irregularity or overcorrection are recommended.[6] However, it is important to caution that surgical correction though blepharoplasty incisions for contour irregularities are reported, and ultimately lead to a surgical incision when patients originally want a less invasive approach. Blindness is also a potential compilation; however, this has only been described with fat injection in other periorbital areas. Overall, to decrease potential disastrous complications, limited injection material per site, blunt needles, superficial plane injection, and minimal injection pressure are recommended.
While there are plenty of non-surgical techniques that can treat tear trough deformities, namely fillers and fat transfer, patients with increased loss of volume in the area may select to receive a tear trough/infraorbital rim implant to provide a long-lasting volume enhancement. Common alloplastic implants used are made from either polyethylene (Medpor) or silicone, and when used in the face, each type is attributed to different complication rates, with silicone implants having higher incidence of infections or displacements and Medpor implants having higher incidence of prominence problems.[13] Other complications associated with treatment of tear trough deformities include:
- Chemosis due to lymphatic obstruction or dryness of conjunctiva
- Lid malposition ranging from minimal scleral show to ectropion
- Over Dissection of nasojugal area leading to damage of the buccal branch of the facial nerve
- Persistent dark circles from periorbital hyperpigmentation
- Postoperative edema and ecchymosis
and the treatment of each complication is dependent on the severity of expression.[6]
Beyond the commonly reported complications of injection, malposition, and localized nerve injury, there has also been a case reported on penetration of the lacrimal sac from a tear trough implant. Although uncommon, the piercing of the lacrimal sac with an infraorbital implant should also be considered as a complication, especially if the implant is placed incorrectly. Complications strictly related to the surgeries involving implants include: Incorrect implant size, neuropraxia, intra-sinus penetration, fistula, displacement and migration, implant fracture, and loosening of hardware. While implants can be bought in varying sizes, there is also reported use of customized facial implants that may indicate better fitting implants on an individualized basis.[20]
In the context of TED, it is important to understand how thyroid disease may change their preoperative and postoperative management. For patients documented for euthyroidism, no additional testing before surgery will be needed. However, in the context of patients with known history of TED, it would be appropriate to check thyrotropic level.
For a patient with known hyperthyroidism undergoing an infraorbital rim-implant surgery, it is important to take into consideration any effects the elevated thyroid levels may have on the heart. Namely, increased TSH can impact the cardiovascular system by increasing positive inotropic and chronotropic effects on the heart, increasing vasodilation due to decreased systemic vascular resistance, and increased sodium and water retention. Further, atrial fibrillation occurs in 10-15% of patients, and the likelihood increases with age. Despite these known effects to the cardiovascular system, there are no published studies that evaluate perioperative outcomes of hyperthyroid patients compared to euthyroid patients. Performing operations on hyperthyroid patients is associated with precipitating thyroid storm, leading to tachycardia, confusion, gastrointestinal complaints, fever, and cardiovascular collapse; therefore, patients should present with normal TSH levels prior to receiving elective procedures to reduce complication risk. Specifically, in patients with Graves disease, antithyroid drugs (ATDs) should be used to rapidly decrease thyroid hormone levels. Physicians should also consider putting patients on beta-blockers to ensure that cardiac status can be optimized.
With elective infraorbital rim implantation, the timing of when a patient receives the implant is important on how to manage perioperative care. As such, there is potential for patients to be experiencing hypothyroidism following thyroidectomy for TED.[21] Perioperative management of hypothyroid patients includes a TSH test to determine adequacy of treatment and optimal thyroid levels. Surgical complications include increased risk for coronary events, diminished cardiac output, ventilatory and renal dysfunctions, decreased gastrointestinal motility leading to higher occurrence of postoperative ileus, normocytic anemia, and a rare occurrence of myxedema coma. Due to the pathophysiological changes associated with low TSH levels, it may be preferred to postpone any elective surgery until thyroid levels have been addressed.
Prognosis
The efficacy and duration of hyaluronic acid treatment of tear trough deformities has been reported to range from six months to two years.[6] Although found with a small sample size, Donath at el was also able to determine that 85% of aesthetic result was maintained for 15 months. The long lasting effect was attributed to low levels of movement in the area when compared to nasolabial folds or lips. Further, positive results with proper technique and patients results in 85-88% increase in aesthetic improvement, with proper patients being selected based on attributes such as; thicker skin, minimal pigmentation changes, and moderate deformity. Patients with more significant deformities may benefit from more invasive techniques; such as lower lid blepharoplasty.
While the prognosis between surgical procedures to fix tear trough deformities varies on the procedure type, technique, and surgeon experience, one study highlighted the performance of alloplastic implant augmentation for 10 patients over a nine-year period. Of the patient’s included, there was an average follow-up of 3 years and no reported infections, palpebral fissure distortions or infraorbital nerve damage. Notably, only one patient had to go under an additional revision surgery and one patient had implants removed due to there being a “too great of change” in his appearance. Of the 10 patients who were directly covered in the study, six unique diagnoses were attributed to the patients, with one repair being for thyroid ophthalmopathy. The low incidence of revisional surgery in this study may be generalizable to many conditions that lead to TTD; however, it is important to note that this study only covered 10 patients and alloplastic implants.[9]
Summary
Thyroid eye disease (TED) often presents with exophthalmos and lower lid retraction, due to the increased production of thyroid hormone leading to inflammation and volume expansion of the extraocular eye muscles. The presence of exophthalmos and lower lid retraction leads to a pronounced appearance of the tear-trough, and a tear trough deformity is a natural consequence to changes in the periorbital tissue. Tear trough deformities can further be classified with different grades or classes, which ultimately determines the best treatment for the deformity.
TED is diagnosed through a complete medical history and physical exam. In patients who have increased prominence of eyes with sunken or hollow features, treatment of tear trough deformities may be indicated and can be performed with minimally invasive techniques, including hyaluronic acid fillers and fat grafting. These techniques are generally used for less severe presentations of deformities or for patients looking for non-surgical options. For severe cases, surgery and insertion of infraorbital rim implants is often recommended.
Surgical tear trough implantation is generally an elective procedure that can lead to a more youthful and vibrant appearance for the patient. Silicone, polyethylene, or PEEK are the usual composition of implants and the size and type of implant depend on a patient’s individual anatomy and aesthetic goals. Surgical approaches to tear trough implantation include transconjunctival, subciliary, transcutaneous, and endoscopic approaches. The approach to treatment and the type of implant can impact the expected complications of a tear trough deformity repair procedure. Surgeons performing tear trough implants in the context of TED should ensure hormone levels are balanced to reduce any complications associated with hyperthyroidism or hypothyroidism.
References
- ↑ McAlinden C. An overview of thyroid eye disease. Eye Vis. 2014;1:9. doi:10.1186/s40662-014-0009-8
- ↑ Lazarus JH. Epidemiology of Graves’ orbitopathy (GO) and relationship with thyroid disease. Best Pract Res Clin Endocrinol Metab. 2012;26(3):273-279. doi:10.1016/j.beem.2011.10.005
- ↑ Jump up to: 3.0 3.1 Bahn RS. Graves’ Ophthalmopathy. N Engl J Med. 2010;362(8):726-738. doi:10.1056/NEJMra0905750
- ↑ Perros P, Neoh C, Dickinson J. Thyroid eye disease. BMJ. 2009;338:b560. doi:10.1136/bmj.b560
- ↑ Anatomy and Nonsurgical Correction of the Tear Trough Deformity. Accessed April 11, 2023. https://oce.ovid.com/article/00006534-201002000-00036/HTML
- ↑ Jump up to: 6.0 6.1 6.2 6.3 6.4 Stutman RL, Codner MA. Tear Trough Deformity: Review of Anatomy and Treatment Options. Aesthet Surg J. 2012;32(4):426-440. doi:10.1177/1090820X12442372
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Sharad J. Dermal Fillers for the Treatment of Tear Trough Deformity: A Review of Anatomy, Treatment Techniques, and their Outcomes. J Cutan Aesthetic Surg. 2012;5(4):229-238. doi:10.4103/0974-2077.104910
- ↑ Shah SS, Patel BC. Thyroid Eye Disease. In: StatPearls [Internet]. StatPearls Publishing; 2022. Accessed May 29, 2023. https://www.ncbi.nlm.nih.gov/books/NBK582134
- ↑ Jump up to: 9.0 9.1 Yaremchuk, Michael J. “Infraorbital Rim Augmentation.” Plastic and reconstructive surgery (1963) 107.6 (2001): 1585–1592. Web.
- ↑ Liaboe CA, Simmons BA, Clark TJ, Shriver EM. Thyroid Eye Disease: A Summary of Information for Patients. EyeRounds.org. March 4, 2020; Available from: http://eyerounds.org/patients/thyroid-eye-disease.htm
- ↑ Customized Infraorbital Rim Implant Beverly Hills | Tear Trough Implant. Taban MD. Accessed May 29, 2023. https://tabanmd.com/customized-infraorbital-rim-implant/
- ↑ Saenz, B., Mueller, B., Vanrachack, A. V., & Davies, B. (2019, October 15). Thyroid eye disease in your exam lane. Review of Optometry. https://www.reviewofoptometry.com/article/thyroid-eye-disease-in-your-exam-lane#:~:text=Surgical%20intervention%20is%20best%20done,for%20at%20least%20six%20months
- ↑ Jump up to: 13.0 13.1 Rojas YA, Sinnott C, Colasante C, Samas J, Reish RG. Facial Implants: Controversies and Criticism. A Comprehensive Review of the Current Literature. Plast Reconstr Surg. 2018;142(4):991. doi:10.1097/PRS.0000000000004765
- ↑ Niechajev I. Facial reconstruction using porous high-density polyethylene (medpor): long-term results. Aesthetic Plast Surg. 2012;36(4):917-927. doi:10.1007/s00266-012-9911-4
- ↑ Hwang SM, Park SH, Lee JS, Kim HD, Hwang MK, Kim MW. Improvement of Infraorbital Rim contour Using Medpor. Arch Craniofacial Surg. 2016;17(2):77-81. doi:10.7181/acfs.2016.17.2.77
- ↑ Narciso R, Basile E, Bottini DJ, Cervelli V. PEEK Implants: An Innovative Solution for Facial Aesthetic Surgery. Case Rep Surg. 2021;2021:5518433. doi:10.1155/2021/5518433
- ↑ Nagaraj V, Ghosh A, Nanjappa M, Ramesh K. ‘Sutureless’ transconjunctival approach for infraorbital rim fractures. Contemp Clin Dent. 2015;6(Suppl 1):S56-S58. doi:10.4103/0976-237X.152939
- ↑ Raschke GF, Rieger UM, Bader RD, Schaefer O, Guentsch A, Schultze-Mosgau S. Transconjunctival versus subciliary approach for orbital fracture repair--an anthropometric evaluation of 221 cases. Clin Oral Investig. 2013;17(3):933-942. doi:10.1007/s00784-012-0776-3
- ↑ Jump up to: 19.0 19.1 Abussuud Z, Ahmed S, Paluzzi A. Surgical Approaches to the Orbit: A Neurosurgical Perspective. J Neurol Surg Part B Skull Base. 2020;81(4):385-408. doi:10.1055/s-0040-1713941
- ↑ Okafor LO, Jamison A, Ali S, Malhotra R. Tear Trough Malar Implant Penetrating Lacrimal Sac Causing Lacrimal Obstruction and Epiphora: Case Report and Review. Ophthal Plast Reconstr Surg. 2022;38(3):e70-e72. doi:10.1097/IOP.0000000000002104
- ↑ Palace MR. Perioperative Management of Thyroid Dysfunction. Health Serv Insights. 2017;10:117863291668967. doi:10.1177/1178632916689677
- Perros P, Crombie AL, Matthews JNS, Kendall-Taylor P. Age and gender influence the severity of thyroid-associated ophthalmopathy: a study of 101 patients attending a combined thyroid-eye clinic. Clin Endocrinol (Oxf). 1993;38(4):367-372. doi:10.1111/j.1365-2265.1993.tb00516.x
- Hassan Hussien M, Abd El-Wahed Hassan E, El-Haddad NSEDM. Comparison between hyaluronic acid filler and botulinum toxin type A in the treatment of thyroid upper eyelid retraction. Ther Adv Ophthalmol. 2020;12:2515841420979113. doi:10.1177/2515841420979113

