ICRS: Extrusion Management
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease entity
Intrastromal corneal ring segment or intracorneal ring segment (ICRS) extrusion occurs due to a progressive superficial stromal thinning and epithelial breakdown, subsequently leading to ring protrusion.[1][2] This is reversible or mitigated with ring explantation.[1][2] ICRS extrusion is the most common cause requiring ICRS explantation and accounts for 48.2% of all explanted cases.[2] ICRS extrusion is caused most often by ring migration and/or corneal melting and presents with foreign body sensation and photophobia with epithelial defects.[3]
Etiology
ICRS extrusion results from progressive, stromal thinning, and subsequent ring protrusion through an epithelial defect, the latter of which is required for the diagnosis of ICRS extrusion.[1][2] ICRS extrusion is often preceded by corneal melting or ring migration but can also occur with deep neovascularization, infectious, and sterile keratitis.[3]
Pathology
Ring migration and corneal melting are preceding signs of ICRS extrusion resulting from epithelial hypoplasia and stromal thinning with subsequent ring exposure and protrusion through an epithelial defect.[4] Findings in ICRS extrusion resolve with ring explantation.[1][2]
- Ring migration is an early sign of ring extrusion. Shallow ICRS implantation leads to increased anterior tensile strain, stromal compression, compressed anterior stromal depth, epithelial-stromal breakdown, corneal thinning, and spontaneous extrusion.[5][6][7]
- Corneal melting suggests an underlying inflammatory process.[2] Kugler et al. proposed that surgical trauma during incision and tunnel creation results in progressive keratocyte apoptosis, tissue degeneration, and corneal melting.[8] Furthermore, this progressive keratolysis following ICRS implantation can be related to degradation of the corneal matrix by matrix metalloproteinases (MMP), because the introduction of exogenous stimuli and tear film insufficiency often leads to overexpression of MMP-1 and MMP-2, resulting in corneal thinning.[1][2]
Risk Factors
Ring migration
- Ring migration is caused by excessive ICRS width in a thin cornea, shallow tunnel placement, and narrow tunnels.[3][4][6]
- A narrow ICRS channel (6.6 mm x 7.6 mm) can result in ring migration with epithelial plugging, tunnel haze, compared to the wide (6.7 mm x 8.2 mm) tunnel group.[6]
Corneal melting
- ICRS tip placement close to the incision is the leading risk factor for infection, extrusion, and corneal melting.[8]
- Inflammation caused by infection, trauma, and stromal separation often results in channel deposits or infiltrates and can progress to ring extrusion.[1][9][10]
- Simultaneous cross-linking and keratoconus grade 3 with eccentric cones are risk factors for ring migration and corneal melting.[4]
Primary prevention
History
- Patients with a history of vernal conjunctivitis or chronic eye rubbing should be offered ICRS with caution.
- Treatment of vernal conjunctivitis should take place prior to ICRS implantation.[11]
CAS-OCT
- Cornea and anterior segment ocular coherence tomography (CAS-OCT) should be used on the first week and month following ICRS implantation to identify patients at high risk of extrusion.
- Patients at high risk have a mean percentage depth of less than 60% or a tunnel depth of less than 70% and should be followed closely.[7]
Device selection and segment placement
- ICRS implantation should be placed away from the incision site and include a ring thickness that is less than half of the pachymetry thickness at the site of implantation.[12] ICRS extrusion occurs most often in patients with thin stroma and ring placement close to the incision.[12] Furthermore, the incidence of ICRS extrusion decreased significantly after applying this ‘pachymetry law’ to ICRS implantation.[12][13]
- Lai et al. suggests that superior segment placement may reduce progressive stromal thinning.[7]
Tunnel creation
- Femtosecond lasers are recommended for tunnel creation because they are faster, easier, more reproducible. Femtosecond lasers also offer greater control and accurate tunnel dimensions.[3] These factors reduce the risk of postoperative complications, such as ring migration and late spontaneous extrusion. Femtosecond lasers also cause minimal epithelial changes, faster recovery, and more precise stromal separation as compared to mechanical dissection.[3] Other studies have shown no significant difference in extrusion rates between mechanical and femtosecond laser tunnel creations.[1]
- Shallow tunnel creation can be prevented by setting the channel depth to 80% using the femtosecond laser or the diamond blade knife.[8]
- A wide (6.7 mm x 8.2 mm) tunnel can reduce the risk of ring migration and extrusion.[6]
- ICRS implantation in the posterior 2/3 of the stroma has been proposed as a possible way to reduce stromal thinning and ICRS extrusion.[1][2]
Diagnosis
History
ICRS extrusion is diagnosed clinically with the presence of stromal thinning and ring protrusion through an epithelial defect that resolves with ring explantation. [1][2][3] ICRS extrusion has a mean onset of around 10 years, but cases can occur anywhere from 1 month to 20 years following implantation.[14][15]
Symptoms
- Foreign body sensation is the most common symptom.
- Other symptoms include photophobia, tearing, itching, and preceding eye rubbing or trauma.[3][4][9][14][16]
Signs
- Diagnostic features include an area of stromal thinning, epithelial defect, and ring protrusion.[1][2][3]
- Preceding corneal melt, ring migration, or anterior stromal necrosis are signs of impending extrusion. [1][2][3][9][14]
- Epithelial defects resolve with explantation but not with contact lens discontinuation.[1] Punctate, arcuate, or linear staining patterns can occur.[9][14][16]
- Tunnel vascularization can occur with superficial corneal vascularization.
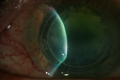
Diagnostic procedures
- Slit-lamp examination should be used to detect stromal thinning, ring protrusion, and an epithelial defect.[1]
- Corneal staining with fluorescein can confirm the epithelial defect.[1]
- Corneal topography should be used to identify unstable ring positions, as depicted by topographical shifts and keratometric flattening.[17]
- Cornea and anterior segment ocular coherence tomography (CAS-OCT) should be used to identify superficial ring placement or focal corneal thinning around the involved ring segment on pachymetry. [7][18] A superficial ring placement, defined by Lai et al. as a mean percent depth of 60% or less, increases a patient’s risk for epithelial-stromal breakdown and ring extrusion.[7]
Complications after ICRS implantation
Possible postoperative complications following ICRS implantation:
- Segment migration presents with undesirable refractive outcomes despite the help of scleral contact lenses and unstable segment position on topography.[1][4]
- Corneal melting is an epithelial breakdown with a defect, which leads to stromal thinning. Lack of corneal integrity would result in worsening irritation with scleral contact lenses.[4]
- Anterior stromal necrosis is stromal thinning and ring exposure with overlying debridable epithelium that precede ring extrusion by about 1 year. Staining occurs after debridement with the use of a cotton sponge applicator. Linear ring exposures without protrusions can be present. Erosions are a rare finding. An inflammatory halo around the tunnel can also be present. Stromal infiltrates may suggest an infectious process.[9]
- Infectious keratitis is one of the four most common causes of ring explantation[1] and usually presents with more acute pain, photophobia, decreased visual acuity, stromal infiltrates stromal necrosis and an epithelial defect that resolves with antibiotics. [19] Rapidly progressive infectious keratitis can quickly lead to endophthalmitis with hypopyon and fibrin formation.[20]
- Lamellar channel deposits are cellular and protein deposits that are found on the inner curvature of the proximal ring segment near the incision site. Lamellar channel deposits can be confirmed on the slit-lamp exam. Ruckhofer et al. suggests that increased segment thickness and duration increases the incidence of channel deposits and can present with anterior stromal necrosis.[10]
- Tunnel vascularization presents with contact lens intolerance with poor fitting fluctuating vision, halos around lights, crystallized deposits, and stromal vascularization around the ring segments. An epithelial defect without stromal thinning resolves with discontinuation and re-steepening of scleral contact lenses. Contact lens intolerance despite discontinuation and re-steepening should be managed with ring explantation, due to poor visual outcomes.[1]
Management
Explantation
- Explantation is the surgical removal of ICRS ring segments and is indicated in cases of ICRS extrusion, poor visual quality or fluctuations in vision, corneal melting, culture-positive or negative keratitis, corneal neovascularization with poor contact lens fitting, and corneal perforation.[3][4][18]
- Incisions can be made in one of two ways. If the extrusion was proximate to the incision site, the previous entry can be opened with a Sinskey hook. A 10-0 nylon suture should be used to close the defect. If the incision site is completely healed, a diamond blade set to the original depth should be used to make an incision entry beneath the extruded ring. The depth of the ring can be confirmed on CAS-OCT. A circumferential dissector can be used to create a channel beneath the segment. A Sinskey hook is then placed anterior to the segment and pushed down gently to break adhesions between the ring and the stroma and to pull the positioned segment through the new entry site.[21]
- Conjunctival and corneal swab with culture are performed in all suspected infections. Infectious keratitis should be treated aggressively with topical fortified antibiotics and explantation, but fortified antibiotics without explantation are also effective in some cases.[20] Systemic antibiotics can also be used in cases of endophthalmitis, [22] Hashemi et al. suggests that early penetrating keratoplasty can be alternatively for rapidly progressive keratitis.[20]
Postoperative management
- Combination antibiotic-steroid eye drops for 5 days[5]
- Artificial tears for 1-3 months, and are instructed to avoid eye rubbing[5]
- Adjunctive therapy includes an amniotic membrane to fill the virtual gap or bandage contact lenses to aid corneal epithelial healing. The amniotic membrane (glycerin-preserved) maintained transparency by 2 years but does not prevent myopization and increased astigmatism.[9]
- Fortified antibiotics can be continued at a lower frequency for 3 weeks in cases of infectious keratitis, following explantation.[23]
- Topical steroids for at least 10 days following explantation secondary to deep corneal neovascularization to promote ghost vessel regression and improve contact lens tolerance.[1][24]
Complications
Complications after explantation
Clinch et al. reported postoperative data of 46 out of 684 myopic eyes following ring explantation and concluded that ring removal is not associated with decreased BCVA, astigmatism, or myopia.[25]
Complications of ring segment explantation include:
- Tracks of lamellar haze that decreases over time [26]
- Persistent incision scar without visual impairment [26]
- Corneal neovascularization[16]
- Partial stromal melt[16]
- Cosmetic complaints from permanent stromal haze[16]
- Corneal leukoma[20]
Follow-up
In most cases of explantation, patient follow-up should occur on the first day postoperatively, 1 month, 3 months, 6 months, and 1 year postoperatively with slit lamp exam, UCVA, BCVA, corneal topography. Visual, refractive, and topographic changes were normal after 3 months. [5]
Reference
- ↑ Jump up to: 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 Kramer EG, Boshnick EL. Scleral lenses in the treatment of post-LASIK ectasia and superficial neovascularization of intrastromal corneal ring segments. Cont Lens Anterior Eye. 2015;38(4):298-303. doi:10.1016/j.clae.2015.02.003
- ↑ Jump up to: 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Ferrer C, Alió JL, Montañés AU, et al. Causes of intrastromal corneal ring segment explantation: clinicopathologic correlation analysis. J Cataract Refract Surg. 2010;36(6):970-977. doi:10.1016/j.jcrs.2009.12.042
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Bautista-Llamas MJ, Sánchez-González MC, López-Izquierdo I, et al. Complications and Explantation Reasons in Intracorneal Ring Segments (ICRS) Implantation: A Systematic Review. J Refract Surg. 2019;35(11):740-747. doi:10.3928/1081597X-20191010-02
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Mounir A, Farouk MM, Abdellah MM, Mohamed Mostafa E. Extrusion of Femtosecond Laser-Implanted Intrastromal Corneal Ring Segments in Keratoconic Eyes: Prevalence, Risk Factors, and Clinical Outcomes. J Ophthalmol. 2020;2020:8704219. Published 2020 Mar 28. doi:10.1155/2020/8704219
- ↑ Jump up to: 5.0 5.1 5.2 5.3 Alió JL, Artola A, Ruiz-Moreno JM, Hassanein A, Galal A, Awadalla MA. Changes in keratoconic corneas after intracorneal ring segment explantation and reimplantation. Ophthalmology. 2004;111(4):747-751. doi:10.1016/j.ophtha.2003.08.024
- ↑ Jump up to: 6.0 6.1 6.2 6.3 Ertan A, Kamburoğlu G, Akgün U. Comparison of outcomes of 2 channel sizes for intrastromal ring segment implantation with a femtosecond laser in eyes with keratoconus. J Cataract Refract Surg. 2007;33(4):648-653. doi:10.1016/j.jcrs.2007.01.014
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 Lai MM, Tang M, Andrade EM, et al. Optical coherence tomography to assess intrastromal corneal ring segment depth in keratoconic eyes. J Cataract Refract Surg. 2006;32(11):1860-1865. doi:10.1016/j.jcrs.2006.05.030
- ↑ Jump up to: 8.0 8.1 8.2 Torquetti L, Cunha P, Luz A, et al. Clinical Outcomes After Implantation of 320°-Arc Length Intrastromal Corneal Ring Segments in Keratoconus. Cornea. 2018;37(10):1299-1305. doi:10.1097/ICO.0000000000001709
- ↑ Jump up to: 9.0 9.1 9.2 9.3 9.4 9.5 Kugler LJ, Hill S, Sztipanovits D, Boerman H, Swartz TS, Wang MX. Corneal melt of incisions overlying corneal ring segments: case series and literature review. Cornea. 2011;30(9):968-971. doi:10.1097/ICO.0b013e3182031ca0
- ↑ Jump up to: 10.0 10.1 Ruckhofer J, Twa MD, Schanzlin DJ. Clinical characteristics of lamellar channel deposits after implantation of intacs. J Cataract Refract Surg 2000; 26:1473–1479
- ↑ Mohammed Iqbal, Ahmed Elmassry, Hisham Saad, Ahmed AM Gad, Ola Ibrahim, Noha Hamed, Ahmed Saeed, Ahmad S. Khalil, Mohamed Tawfik, Amr Said, Ibrahim Amer, Asaad Nooreldin, Omar Said, Mohamed Reffat, Seif Anwar, Amani Badawi. (2020) Standard cross‐linking protocol versus accelerated and transepithelial cross‐linking protocols for treatment of paediatric keratoconus: a 2‐year comparative study. Acta Ophthalmologica 98:3.
- ↑ Jump up to: 12.0 12.1 12.2 Ferrara G, Torquetti L, Ferrara P, Merayo-Lloves J. Intrastromal corneal ring segments: visual outcomes from a large case series. Clin Exp Ophthalmol. 2012;40(5):433-439. doi:10.1111/j.1442-9071.2011.02698.x
- ↑ Twa MD, Kash RL, Costello M, Schanzlin DJ. Morphologic characteristics of lamellar channel deposits in the human eye; a case report. Cornea 2004; 23:412–420
- ↑ Jump up to: 14.0 14.1 14.2 14.3 Abad JC, Gómez IC, Henriquez MA, Donado JH. Biomicroscopic Findings And Management Of Anterior Stromal Necrosis After Long-Term Implantacion Of Intacs [published online ahead of print, 2020 Jul 27]. Am J Ophthalmol. 2020;S0002-9394(20)30390-1.
- ↑ Kubaloglu A, Sari ES, Cinar Y, et al. Comparison of mechanical and femtosecond laser tunnel creation for intrastromal corneal ring segment implantation in keratoconus: prospective randomized clinical trial. J Cataract Refract Surg. 2010;36(9):1556-1561. doi:10.1016/j.jcrs.2010.04.028
- ↑ Jump up to: 16.0 16.1 16.2 16.3 16.4 Oatts JT, Savar L, Hwang DG. Late extrusion of intrastromal corneal ring segments: A report of two cases. Am J Ophthalmol Case Rep. 2017;8:67-70. Published 2017 Oct 6. doi:10.1016/j.ajoc.2017.10.004
- ↑ Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: efficacy and complications. Cornea. 2006;25(1):29-33. doi:10.1097/01.ico.0000167883.63266.60
- ↑ Jump up to: 18.0 18.1 Bourges JL, Trong TT, Ellies P, Briat B, Renard G. Intrastromal corneal ring segments and corneal anterior stromal necrosis. J Cataract Refract Surg. 2003;29(6):1228-1230. doi:10.1016/s0886-3350(02)02036-9
- ↑ Ibáñez-Alperte J, Pérez-García D, Cristóbal JA, Mateo AJ, Río BJ, Mínguez E. Keratitis after Implantation of Intrastromal Corneal Rings with Spontaneous Extrusion of the Segment. Case Rep Ophthalmol. 2010;1(2):42-46. Published 2010 Sep 13. doi:10.1159/000320585
- ↑ Jump up to: 20.0 20.1 20.2 20.3 Hashemi H, Ghaffari R, Mohammadi M, Moghimi S, Miraftaab M. Microbial keratitis after INTACS implantation with loose suture. J Refract Surg. 2008;24(5):551-552. doi:10.3928/1081597X-20080501-17
- ↑ Nguyen N, Gelles JD, Greenstein SA, Hersh PS. Incidence and associations of intracorneal ring segment explantation. J Cataract Refract Surg. 2019;45(2):153-158. doi:10.1016/j.jcrs.2018.09.021
- ↑ Neira W, Krootila K, Holopainen JM. Atopic dermatitis is a risk factor for intracorneal ring segment extrusion. Acta Ophthalmol. 2014;92(6):e491-e492. doi:10.1111/aos.12377
- ↑ Bourcier T, Borderie V, Laroche L. Late bacterial keratitis after implantation of intrastromal corneal ring segments. J Cataract Refract Surg. 2003;29(2):407-409. doi:10.1016/s0886-3350(02)01484-0
- ↑ Cosar CB, Sridhar MS, Sener B. Late onset of deep corneal vascularization: a rare complication of intrastromal corneal ring segments for keratoconus. Eur J Ophthalmol. 2009;19(2):298-300. doi:10.1177/112067210901900222
- ↑ Clinch TE, Lemp MA, Foulks GN, et al. Removal of INTACS for myopia. Ophthalmology. 2002; 109(8): 1441-1446. doi.org/10.1016/S0161-6420(02)01090-4
- ↑ Jump up to: 26.0 26.1 Schanzlin DJ, Abbott RL, Asbell PA, et al. Two-year outcomes of intrastromal corneal ring segments for the correction of myopia. Ophthalmology. 2001;108(9):1688-1694. doi:10.1016/s0161-6420(01)00692-3