Hypotony Maculopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Definition
Hypotony may be defined both statistically and clinically. The statistical definition of hypotony is intraocular pressure (IOP) less than 6.5mmHg, which is more than 3 standard deviations below the mean IOP. The clinical definition of hypotony is IOP low enough to result in vision loss. The vision loss from low IOP may be caused by corneal edema, astigmatism, cystoid macular edema, or maculopathy. Hypotony maculopathy is characterized by a low IOP associated with fundus abnormalities, including chorioretinal folds, optic nerve head edema in the acute setting , and vascular tortuosity.
History
Hypotony maculopathy was first described by Dellaporta in 1954. In 1972, Gass developed the term, “Hypotony Maculopathy”, to emphasize the etiology of visual loss associated with the chorioretinal folds.[2]
Etiology
Hypotony maculopathy may occur after ocular inflammation, trauma, or surgery. Most cases are secondary to glaucoma filtration surgery with a reported incidence of 1.3% to 18%. Furthermore, the risk of hypotony maculopathy increases with the use of antifibrosis agents during glaucoma surgery.[3]
Postoperative Hypotony
- Mitomycin C (MMC) toxicity of the ciliary body
- Overfiltration
- Bleb Leak
- Wound Leak
- Iridocyclitis
- Cyclodialysis
- Ciliochoroidal Detachment
- Retinal Detachment
Traumatic Hypotony
- Scleral perforation
- Retinal Detachment
- Cyclodialysis
- Iridocyclitis
- Ciliochoroidal Detachment
Bilateral Hypotony
- Osmotic Dehydration
- Diabetic coma
- Uremia
- Myotonic Dystrophy
Miscellaneous forms of hypotony
- Ciliary body hypoperfusion from vascular occlusive disease
Risk Factors [4]
- Male gender
- Myopia
- Young Age
- Primary Glaucoma Filteration Surgery
- Use of antifibrotic agents (Mitomycin C >> 5-Fluorouracil)
- Elevated Pre-Operative IOP
Pathophysiology
Hypotony can occur with either increased outflow of aqueous humor or, less often, reduced production of aqueous humor by the ciliary body. Increased outflow may occur via a surgical wound leak, overfiltering bleb, cyclodialysis cleft, scleral rupture, etc. Decreased aqueous humor production by the ciliary body is usually seen in the setting of inflammatory conditions. With the onset of hypotony, the scleral wall collapses inward resulting in choroid and retina redundancy which gives the characteristic chorioretinal wrinkling. The antero-posterior diameter of the eye shortens which can manifest as a refractive hyperopic shift.[2] Anterior bowing of the lamina cribrosa in the optic nerve leads to restricted axoplasmic flow causing disc swelling in the acute phase.[5] Patients with advanced optic nerve disease may not develop optic nerve head swelling and edema due to fewer viable axons.
Diagnosis
Symptoms
Patients may complain of distortion in their central vision or may be completely asymptomatic.
Physical Examination
- Intraocular pressure less than 6.5mm Hg
- Painless, decreased vision
- Hyperopic shift in refraction
- Characteristic fundus changes: chorioretinal folds, vascular tortuosity, and optic disc swelling
Diagnostic Procedures
Ultrasound biomicroscopy (UBM): Assists in further evaluation of anterior chamber depth and iris contour and visualization of anatomical structures posterior to the iris. The position of the ciliary body or its anterior rotation may provide useful information. It may also detect cyclodialysis cleft when missed clinically.
Optical coherence Tomography (OCT): Helps to confirm the diagnosis and monitor outcomes after various types of interventions. It may detect the subtle wrinkling of the chorioretinal folds in the posterior pole that may be difficult to assess with direct or indirect ophthalmoscopy. Furthermore, OCT has been shown to detect pathology in the presence of a normal ocular exam. Careful review of all radial line scans of OCT is important to assess for folds and diagnose the condition. [6]
Fluorescein angiography (IVFA): Shows an increase in choroidal fluorescence at the crest of choroidal folds due to the thinning of the RPE . The troughs appear hypofluorescent. Clinically, these changes appear as alternating dark and light bands or streaks in the retina. IVFA may also reveal leakage associated with the optic disc in the acute phase.
Indocyanine Green Angiography (ICG): May detect cases not diagnosed with IVFA. Multiple hypofluorescent streaks in the fundus are noted.
B-scan: Shows the presence or absence of choroidal or retinal detachments that may be associated when a clear view of the entire posterior pole is not obtained clinically.It may also show thickening of the posterior sclera and choroid.
Laboratory Test
None
Differential Diagnosis[3][7]
The development of chorioretinal folds may be seen with the following list of diseases included in the differential diagnosis. The mnemonic THIN RPE can helpful.
- T –Tumors: Tumors such as choroidal melanoma or metastasis can cause chorioretinal folds from either compression of choroidal vessels that leads to choroidal edema and scleral thickening or from mechanical displacement.
- H-Hypotony: In hypotony as mentioned above, the scleral wall collapses inward resulting in choroid and retina redundancy which gives the characteristic chorioretinal wrinkling that can be caused by a bleb leak, a wound leak, an over filtering bleb, iridocyclitis, and cyclodialysis.
- I-Inflammation or Idiopathic: Inflammation, as is seen in posterior scleritis, can lead to thickening of the sclera and choroid causing overlying chorioretinal folds. Idiopathic is a diagnosis of exclusion. It is often seen in males and is typically bilateral and symmetric. It is felt to caused by scleral shrinkage likely from a prenatal or childhood illness.
- N-Neovascularization: Neovascularization as is seen in Age-related Macular Degeneration causes displacement and folds of the overlying sensory sensory retina. Photocoagulation and disciform scars may also cause folds secondary to contraction.
- R-Retrobulbar Mass or Retinal Detachment: Retrobulbar masses can lead to mechanical indentation of the globe along with choroidal vascular congestion. Retinal detachments can cause hypotony as mentioned previously in this article.
- P-Papilledema: Papilledema from increased intracranial pressure can be associated with chorioretinal folds radiating from the optic nerve due to obstruction of the axoplasmic flow.
- E-Extraocular Hardware: Scleral buckles, radioactive plaques, and orbital implants can cause focal chorioretinal folds at the location of the hardware.
Management
Medical and Conservative Management
The successful treatment of hypotony maculopathy depends on identification of the underlying etiology and its appropriate treatment. The most common cause of hypotony maculopathy, as mentioned above, is recent glaucoma filtration surgery that may result in either a bleb leak or an overfilterring bleb. In the case of a bleb leak, conservative measures include aqueous suppressants, topical antibiotics, or use of a bandage contact lens. Aqueous suppressants reduce the aqueous outflow through the leak which may facilitate healing of the overlying epithelium. A bandage contact lens promotes epithelial migration and wound healing. A topical antibiotic provides prophylaxis for infection. Aminoglycosides may induce conjunctival inflammation that can stimulate wound healing. Cyanoacrylate glue, autologous blood injection, and compression sutures are other options that can be employed. Various treatment strategies for an overfiltering bleb include quick tapering regimen of topical steroids, autologous blood injection, use of laser to stimulate inflammation, diathermy, trichloroacetic acid, and compression sutures to minimize aqueous outflow. In case hypotony is due to uveitis and hyposecretion, corticosteroids are given to reduce inflammation and thus improve ciliary body function. Inflammation reduces aqueous production and increases uveoscleral outflow. Topical cycloplegics are also used to relax the iris and ciliary body, reducing the potential space for subciliary effusions. [8]
Surgical Management
Surgical intervention is undertaken immediately in cases of trauma, including scleral rupture or retinal detachment. In other etiologies, conservative management should be utilized first, as described above. If these measures fail to resolve the hypotony maculopathy, surgical intervention is warranted. Bleb excision and revision may be required using either the conjunctival advancement approach or a free conjunctival autograft. Vitrectomy has also been decribed as a method of possible treatment for unresolving chorioretinal folds. An ILM peel may provide elimination of contractile forces from subclinical fibrocellular proliferation.[9] Perfluorocarbon liquid has been described to “steam-roller” the retina flat by temporallily increasing the intraoperative IOP to 50 mm Hg intraoperatively.[10]
Prevention
Preventive measures can be taken to decrease the risk of postoperative complications after glaucoma filtration surgery. Antimetabolites should be used judiciously. Care should be taken to avoid contact between the antifibrotic agents and conjunctival edges to avoid thinning of the conjunctiva and subsequent bleb leaks. Multiple scleral flap sutures may be placed to titrate and control aqueous humor flow through the margins of the scleral flap to avoid excessive filtration. Incorporation of Tenon’s capsule with the conjunctiva during closure along with the utilization of tapered needles reduce the risk of postoperative bleb leaks. Care should also be taken in the timing of laser- suture-lysis in the postoperative period to avoid abrupt reduction in IOP.[11]
Prognosis
Prognosis for visual recovery depends on early detection and correction of the underlying pathology. Timely normalization of low IOP may restore scleral and retinal anatomy. If the condition is long standing, intraretinal fibrosis and fibrosis within the sclera and choroid may lead to permanent structural and functional damage even with resolution of the etiology.[12]
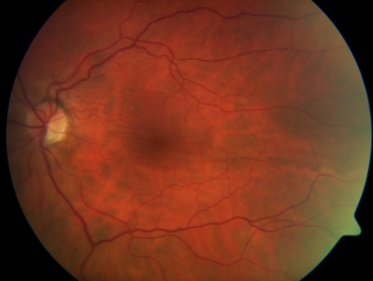
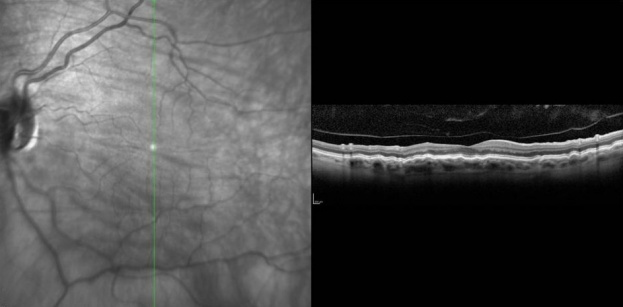
Reference Images
- Photos Courtesy of Sarwat Salim, MD, University of Tennessee
Fundus Photo demonstrating horizontal chorioretinal folds
Heidelberg OCT demonstrating chorioretinal fold with vertical scan
References
- ↑ American Academy of Ophthalmology. Hypotony maculopathy. https://www.aao.org/image/hypotony-maculopathy-2 Accessed July 26, 2019.
- ↑ Jump up to: 2.0 2.1 Gass JD. Hypotony maculopathy. In: Bellows JG (ed.) Contemporary ophthalmology. Honoring Sir Stewart Duke-Elder. Baltimore: Williams & Wilkins. 1972:343–366.
- ↑ Jump up to: 3.0 3.1 Costa VP, Arceiri ES.Hypotony maculopathy. Acta Ophthalmol 2007;586-597.
- ↑ Fannin LA, Schiffman JC, Budenz DL.Risk factors for hypotony maculopathy. Ophthalmology. Jun 2003;110(6):1185-91.
- ↑ Minckler DS, Bunt AH.Axoplasmic transport in ocular hypotony and papilledema in the monkey. Arch.Ophthalmol 95:1430-1436.
- ↑ Budenz DL, Schwartz K, Gedde SJ.Occult hypotony maculopathy diagnosed with optical coherence tomography. Arch Ophthalmol 2005;123:113-114.
- ↑ Gasperini J, Elliot D MD, E.T. Cunningham Jr. ET. How to Recognize and Treat Chorioretinal Folds.Rev.Ophthalmol Vol. No: 13:11Issue: 11/1/2006.
- ↑ Fraunfelder FT. Roy and Fraunfelder’s Current Ocular Therapy. Elsevier Health Sciences; 2008. 732 p.
- ↑ Benson S, Barton K, Gregor Z. Vitrectomy for a Persisting Macular Fold in a Case of Resolved Hypotony Maculopathy. American Journal of Ophthalmology. VOL. 138, NO. 3. September 2004. (487-489)
- ↑ Duker JS, Schuman JS. Successful surgical treatment of hypotony maculopathy following trabeculectomy with topical mitomycin C. Ophthalmic Surg 1994;25:463–465.
- ↑ Scott ML, Netland PA, Salim S.Opthalmic Pearls: Glaucoma - Assessing and Managing Hypotony Maculopathy. Eyenet. Oct. 2009
- ↑ Jampel HD, Pasquale LR, Dibernardo C.Hypotony maculopathy following trabeculectomy with mitomycin C. Arch. Ophthalmol 1992; 110:1049-1050