Hurricane and Blizzard Keratopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
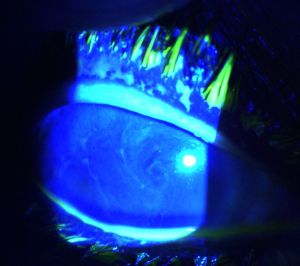
Hurricane keratopathy, or hurricane keratitis, was first described after penetrating keratoplasties by Mackman et al.[1] It is characterized by a whorled pattern seen in the epithelial layer that is highlighted by fluorescein. It appears to be due to increased corneal epithelial turnover, which is also seen in rigid contact lens wearers and with long-term steroid use [2][3]
Terminology
The whorled pattern stains with fluorescein, distinguishing it from similar-appearing cornea verticillata. The term “vortex keratopathy,” another name for cornea verticillata, has also been used to describe hurricane keratopathy.[4][5] However, some authors reserve the terms “vortex keratopathy” and “cornea verticillata” to describe non-staining patterns and hurricane keratopathy to describe those that stain.[3][6] When the pattern appears more random but has the same pathoetiology as hurricane keratopathy, the term blizzard keratopathy has been used.[2]
Etiology
- Commonly reported causes:
- Penetrating keratoplasty
- Rigid contact lens wear
- Chronic topical steroid use
Penetrating keratoplasty was the first cause identified.[1] The use of postoperative steroids and its effect on epithelial healing appears to contribute as the long-term use of topical steroids alone in the absence of surgery may cause hurricane keratopathy, and discontinuation of steroid drops often leads to the pattern disappearance .[1][2]
Rigid contact lenses may lead to hurricane keratopathy, likely due to apex touch causing small abrasions and increased epithelial turnover.[3] Gonugunta reported a case in which a patient developed hurricane keratopathy following cataract surgery, suspected to be due to the use of topical steroids in addition to increased postoperative corneal dryness causing epithelial defects.[7]
Wolfel et al. reported a single case of a patient who developed bilateral corneal epithelial keratitis resembling hurricane keratopathy after using Apremilast. In this setting, the keratopathy likely developed due to either ocular toxicity, seen in other chemotherapeutic and immunosuppressive medications, or a medication-induced change in corneal epithelial proliferation and remodeling.[8] Likewise, there is a case report secondary to belantamab[9]
Risk Factors
Preoperative lid disease, impaired corneal sensation, increased storage time of donor tissues, and use of Healon are potential risk factors for hurricane keratopathy development after penetrating keratoplasty.[6][10]
Pathophysiology
Stem cells located at the corneal-scleral limbus contribute to the regeneration of the corneal epithelium. During the course of normal epithelial regeneration, epithelial cells migrate centripetally from the limbus to the center of the cornea to contribute to corneal surface turnover.[2][7]
At first, the corneal sutures after penetrating keratoplasty were thought to act to impede the migration of cells, leading to the whorled pattern. However, Dua later observed hurricane keratopathy is seen in corneas without surgery and proposed that during periods of accelerated corneal epithelial regeneration, the increase in migration and decrease in normal cell-cell adhesions allows for fluorescein staining and disease development.[2][3]
The whorl pattern is hypothesized to be due to the electromagnetic field of the eye. The eye acts as a dipole, with the cornea having a positive electrical potential relative to the posterior pole of the eye. The electromagnetic field generated by the electric current is distributed in a concentric clockwise pattern on the cornea. Cultured corneal epithelial cells have been shown to respond to high-power magnetic fields regarding their cellular orientation and migration patterns. The concentric distribution of the electromagnetic fields may encourage epithelial cell migration to develop in the characteristic whorl-like pattern seen in hurricane keratopathy.[2][11]
Diagnosis
History
History of a recent corneal graft with use of topical steroids, long-term topical steroid use, or frequent use of rigid gas permeable contact lenses is significant when considering a diagnosis of hurricane keratopathy.[3]
Fiez et al.[6] observed a prevalence of 15% following penetrating keratoplasty, while Mathers and Lemp[12] reported a prevalence of 30% upon slit lamp examination. The central whorl-like pattern can be observed from as early as one week postoperatively and up to eighteen months postoperatively, with the highest incidence occurring between six to twelve months following surgery.[1][12] The duration of symptoms varies, with the use of rigid contact lenses correlating to symptom prolongation. Dua found that the keratopathy persisted for a mean duration of 29.9 weeks following keratoplasty, and for 42.8 weeks after the use of contact lenses.[3]
Symptoms
- Mild ocular irritation and foreign body sensation
- Increased lacrimation
- Photophobia
- Mild blurring of vision.[1][3]
Clinical Diagnosis
The hallmark of hurricane keratopathy is the presence of a whorl-like pattern of epithelial cells that appear as whorled white or grayish-brown lines on the cornea. The pattern is clockwise in the majority of patients. Hurricane keratopathy can be differentiated from vortex keratopathy due to the positive fluorescein stain, which is not observed with the latter.[3][7]
Differential diagnosis
The differential diagnosis of hurricane keratopathy includes vortex keratopathy or corneal verticillata and punctate keratopathy.
Management
General treatment
Hurricane keratopathy generally resolves spontaneously with elimination of the offending stimulus that led to increased cell turnover.[1][3] The whorl-like pattern begins to clear from the periphery and progresses to the center.[2][3]
When hurricane keratopathy develops following a recent corneal graft, discontinuation of topical steroids is observed to correspond with improvement and resolution of the keratopathy within three weeks to six months after discontinuation. In individuals using rigid gas permeable contact lenses, the keratopathy typically resolves following discontinuation of contact lens wear.[3]
The use of preservative-free artificial tears can alleviate symptoms of ocular irritation and foreign body sensation and contribute to the resolution of the keratopathy.[3]
Complications
The epithelial changes observed in hurricane keratopathy generally resolve spontaneously. However, in rare cases, an epithelial defect may persist at the apex of the whorl, or a small component of the whorl may remain at the periphery.[1][3]
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Mackman GS, Polack FM, Sydrys L. Hurricane keratitis in penetrating keratoplasty. Cornea. 1983;2(1):31-4.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Dua HS, Watson NJ, Mathur RM, Forrester JV. Corneal epithelial cell migration in humans: 'hurricane and blizzard keratopathy'. Eye (Lond). 1993;7(1):53-8.
- ↑ Jump up to: 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Dua HS, Gomes JA. Clinical course of hurricane keratopathy. Br J Ophthalmol. 2000 Mar;84(3):285-8.
- ↑ Jackson TL. Moorfields Manual of Ophthalmology, 1e. Maryland Heights: Mosby; 2007.
- ↑ Sharma P, Madi HA, Bonshek R, Morgan SJ. Cloudy corneas as an initial presentation of multiple myeloma. Clin Ophthalmol. 2014 Apr 28;8:813-7.
- ↑ Jump up to: 6.0 6.1 6.2 Feiz V, Mannis MJ, Kandavel G, McCarthy M, Izquierdo L, Eckert M, Schwab IR, Torabian S, Wang JL, Wang W. Surface keratopathy after penetrating keratoplasty. Trans Am Ophthalmol Soc. 2001;99:159-68; discussion 168-70.
- ↑ Jump up to: 7.0 7.1 7.2 Gonuginta VT, Muthaiah S. Hurricane Keratopathy – “A Curlicue on the Cornea”. Delhi J Ophthalmol. 2021; 32(2):63-64.
- ↑ Wolfel L, Franco J, Gillette TB, Chodosh J, Davis A. Bilateral punctate keratitis and hurricane keratopathy following apremilast therapy. Am J Ophthalmol Case Rep. 2023 Aug 3;32:101905. doi: 10.1016/j.ajoc.2023.101905.
- ↑ Haddad C, Motulsky E, Baleine M. Slit-lamp findings in a case of belantamab-induced microcystic hurricane keratopathy. J Fr Ophtalmol. 2024 Jan;47(1):103919. doi: 10.1016/j.jfo.2023.03.033. Epub 2023 Aug 30. PMID: 37652789.
- ↑ Hoffmann F. Zur Pathogenese der Hurrican-Keratitis [Pathogenesis of hurricane keratitis]. Klin Monbl Augenheilkd. 1986 Dec;189(6):442-4.
- ↑ Dua HS, Singh A, Gomes JA, Laibson PR, Donoso LA, Tyagi S. Vortex or whorl formation of cultured human corneal epithelial cells induced by magnetic fields. Eye (Lond). 1996;10 ( Pt 4):447-50.
- ↑ Jump up to: 12.0 12.1 Mathers WD, Lemp MA. Vortex Keratopathy of the Corneal Graft. Cornea. 1991;10(2)93-99.