Foville Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
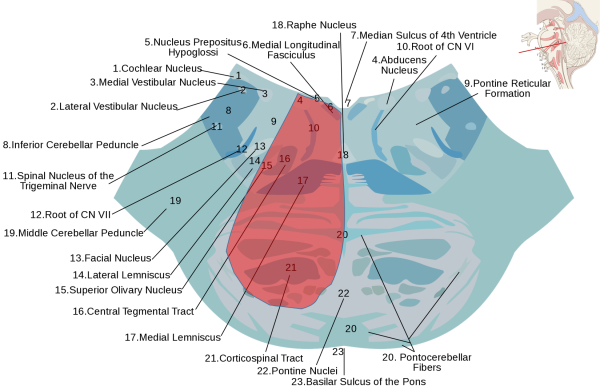
Foville syndrome (FS) is an inferior medial pontine stroke syndrome that most commonly presents with contralateral hemiparesis and ipsilateral abducens and facial palsies.[1][2][3] Ipsilateral Horner syndrome, loss of hearing, facial pain/temperature sensation, and contralateral loss of vibration, fine touch, and proprioception may also be present.[2] These findings are the result of compromised blood flow to the medial caudal pons from perforating branches of the basilar artery.[2][3]
Affected Structures
Usually affected:
- Abducens nucleus or fascicle
- Intrapontine fibers of the facial nerve
- Corticospinal tract
Sometimes affected:
- Medial lemniscus
- Spinal trigeminal nucleus
- Descending sympathetic fibers
- Eighth nerve nuclei
Differentiation from Millard-Gubler Syndrome
FS shares findings of facial nerve palsy and contralateral face-sparing hemiparesis with the ventral pontine syndrome (Millard-Gubler syndrome).[6] Some presentations of Millard-Gubler include sixth nerve involvement, making the distinction between the two syndromes difficult.[6] However, the more dorsal extent of FS involves the abducens nucleus and the adjacent parapontine reticular formation (PPRF).[2][3] Thus, FS can present with conjugate lateral gaze palsy, presenting with an inability to adduct the contralateral eye towards the lesion.[2]
History
FS was first characterized in 1858 by psychiatrist Achille Louis Francois Foville (1831-1887),[7] not to be confused with his father and famed anatomist of the same name (1799-1878).[8]
Etiology
FS is typically caused by a lesion in the lower pontine tegmentum. However, lesions in the superior pons from basilar artery aneurysm have also been reported.[9] These lesions are typically ischemic, precipitated by risk factors for atherosclerotic disease. However, lesions from other causes have also been identified.[10] Both pontine and subarachnoid hemorrhages have been reported to cause the clinical manifestation of FS.[11] Infection from tuberculosis[10] and neoplasm from cerebellar tumor and bronchogenic carcinoma have been reported as well.[12] Therefore, although ischemic infarction is the most common etiology of FS, any damage to the pons may result in the clinical manifestations.
Clinical Manifestations
Due to the involvement of the abducens nucleus, facial nerve fibers, and corticospinal tract of the inferior medial pons, the classic presentation is an abduction deficit of the ipsilateral eye, ipsilateral facial palsy, and contralateral hemiparesis, respectively.[9] However, involvement of other structures in the pons can cause other manifestations. In addition to the sixth and seventh cranial nerves, the spinal trigeminal nucleus and eighth nerve nuclei may be affected.[2] Involvement of the fifth nerve nucleus and/or tract can present with loss of sensation to touch, pain and temperature on the ipsilateral face.[9] Involvement of the eighth cranial nerve can present as ipsilateral sensorineural hearing loss.[2] Additionally, ipsilateral peripheral deafness may occur from involvement of the superior olivary nucleus.[9] If there is damage to the trapezoid body or lateral lemniscus, contralateral deafness may present as well.[10] Involvement of descending tracts in the pons leads to other clinical manifestations. The classic presentation is contralateral hemiparesis from damage to the corticospinal tract. Involvement of the medial longitudinal fasciculus presents with internuclear ophthalmoplegia, manifesting as an inability to adduct the ipsilateral eye.[10] Involvement of the sympathetic fibers can present with the Horner syndrome (ipsilateral ptosis, miosis, and anhidrosis).[9] Lastly, involvement of the cerebellar fibers can present with ataxia.[10]
Diagnostic Criteria/Differential Diagnosis
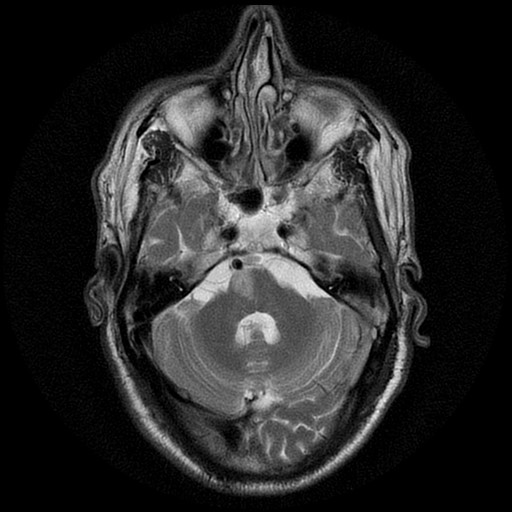
There are no defined diagnostic criteria for FS but a combination of clinical features and radiographic findings confirm the dorsal pontine localization.[2]
When considering the differential diagnosis, it is important to consider any structural lesion that can be found in the inferomedial area of the pons. This includes inflammatory disorders, neoplastic processes, hemorrhages, and vascular malformations such as arteriovenous malformations.[2]
Treatment
Vascular disease is the most common etiology of FS.[2] This can manifest as atheromatous branch occlusion or small vessel occlusion (i.e. lacunar stroke). Thus, antiplatelet therapy, along with secondary prevention by controlling vascular related risk factors, is considered to be the mainstay treatment.[2] In addition to antiplatelet therapy, statin therapy should be started at the time of admission. Other important secondary treatments include following the AHA/Stroke guidelines by controlling blood pressure, diabetes, hyperlipidemia, and smoking cessation.[13][14][15] Finally, further evaluation and rehabilitation by physical medicine and rehabilitation, physical therapists, and occupational therapists is an important step in management. Outpatient follow up after discharge is needed to monitor for possible complications and ensure appropriate recovery. Clinicians should be aware of the clinical and radiographic features of the inferior medial pontine syndrome of Foville (FS).
References
- ↑ Abdrabou, A., El-Feky, M. Inferior medial pontine syndrome. Reference article, Radiopaedia.org. (accessed on 12 Aug 2022) https://doi.org/10.53347/rID-32268
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Khazaal O, Marquez DL, Naqvi IA. Foville Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544268/
- ↑ 3.0 3.1 3.2 Massi DG, Nyassinde J, Ndiaye MM. Superior Foville syndrome due to pontine hemorrhage: a case report. Pan Afr Med J. 2016;25:215. Published 2016 Dec 6. doi:10.11604/pamj.2016.25.215.10648
- ↑ Adapted from “Lower Pons horizontal” (https://upload.wikimedia.org/wikipedia/commons/d/dc/Lower_pons_horizontal_KB.svg) by Marshall Strother and “Brain stem sagittal section” (https://commons.wikimedia.org/wiki/File:Brain_stem_sagittal_section.svg) by Patrick J. Lynch, medical illustrator, CC BY 3.0 https://creativecommons.org/licenses/by/3.0, via Wikimedia Commons
- ↑ Image courtesy of Dr Mohammad A. ElBeialy, Radiopaedia.org, rID: 29951. Used under CC BY-NC-SA 3.0 (https://creativecommons.org/licenses/by-nc-sa/3.0/)
- ↑ 6.0 6.1 Sakuru R, Elnahry AG, Bollu PC. Millard Gubler Syndrome. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532907/
- ↑ Foville A. Note sur une paralysie peu connue de certains muscles de l’œil, et sa liaison avec quelques points de l’anatomie et la physiologie de la protubérance annulaire. Bull Soc Anat. Paris. 1858;33:393–414.
- ↑ Brogna C, Fiengo L, Türe U. Achille Louis Foville's atlas of brain anatomy and the Defoville syndrome. Neurosurgery. 2012;70(5):1265-1273. doi:10.1227/NEU.0b013e31824008e7
- ↑ 9.0 9.1 9.2 9.3 9.4 Acharya, Pant, B., Chandra, A., & Chandra, A. (2021). Fovilles Syndrome a Case to Remember Case Report. Journal of Biomedical Research & Environmental Sciences, 2(10), 1015–1017. https://doi.org/10.37871/jbres1344
- ↑ 10.0 10.1 10.2 10.3 10.4 Cheng, Yen, M.-Y., & Wang, A.-G. (2013). Foville’s syndrome with ipsilateral internuclear ophthalmoplegia due to spontaneous pontine hemorrhage. Taiwan Journal of Ophthalmology, 3(2), 75–77. https://doi.org/10.1016/j.tjo.2012.12.001
- ↑ Takase, Saeki, N., Oka, N., Satoh, A., Otaki, M., & Yamaura, A. (1981). Superior Foville syndrome after clipping of basilar bifurcation aneurysm--case report (author’s transl). Nō shinkei geka, 9(3), 343–47.
- ↑ Man, B. L., & Fu, Y. P. (2015). Bronchogenic carcinoma presented as Foville's syndrome. BMJ case reports, 2015, bcr2014205025. https://doi.org/10.1136/bcr-2014-205025
- ↑ Beucler N, Boissonneau S, Ruf A, Fuentes S, Carron R, Dufour H. Crossed brainstem syndrome revealing bleeding brainstem cavernous malformation: an illustrative case. BMC Neurol. 2021;21(1):204. Published 2021 May 20. doi:10.1186/s12883-021-02223-7
- ↑ Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, Dick F, Taylor GS, Murray G. Medical complications after stroke: a multicenter study. Stroke. 2000 Jun;31(6):1223-9.
- ↑ Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL., American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018 Mar;49(3):e46-e110.

