Firearm Ocular Injury
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Original contributors: Sorensen R, Evenstad J, Siddiqui T, Jaber J, Yen MT.
Disease Entity
Introduction
The American Academy of Pediatrics recently showed that firearms are the leading cause of death in children and youth 0 to 24 years old in the U.S.1 Intentional and unintentional firearm injuries and deaths are a serious threat to public health. Specifically concerning for ophthalmologists is how firearm injury can lead to complete irreversible vision loss.
In the United States, an estimated 3.15 per 1000 population eye injuries are treated in emergency departments every year, and one-third of these patients with serious eye trauma do not regain vision better than 20/200. Despite the gravity of eye injuries, there is a lack of population-based data on visual outcomes and treatment methods for these injuries, including firearm-related ocular trauma, since the National Trauma Database stopped collecting data in 2014 and the USEIR became inactive in 20132. An analysis of the National Trauma Database from 2008-2014 demonstrated that of the 235,254 patients who presented for firearm-related trauma, 8,715 (3.7%) presented with ocular injury3. A separate study showed 1,972 (23%) of these injuries were in pediatric patients, and most injuries were sight-threatening and associated with traumatic brain injury4.
Epidemiology
According to a study published in the JAMA Ophthalmology, firearm-associated ocular injuries are relatively common in the context of gunshot wounds to the head and neck5. The most common types of firearm-related ocular injuries include open wounds of the eyeball and ocular adnexa, orbital injuries or fractures, and contusion of the eye or adnexa. The risk factors for firearm ocular injuries vary depending on the circumstances of the injury5.
Demographics such as age, gender, and race can play a role, as can the location of the injury (home or street). Patients aged 0 to 3 years had greater odds of unintentional injuries (odds ratio [OR], 4.41; 95% CI, 2.51-7.75; P < .001) and injuries occurring at home (OR, 5.39; 95% CI, 2.81-10.38; P < .001). Patients aged less than 10 years had greater odds of open globe injuries (OR 1.84; CI 1.40-2.41; p<0.001)4. Those aged 19 to 21 years had greater odds of assault injuries (OR, 2.17; 95% CI, 1.77-2.66; P < .001) and injuries occurring on the street (OR, 1.61; 95% CI, 1.3-1.98; P < .001)4.
Types of Injuries


The specific types of firearm-related ocular injuries can vary depending on the circumstances of the injury. In pediatric patients, traumatic brain injury and visual pathway injuries (OR, 2.86; 95% CI, 1.95-4.20; P < .001) resulted mostly from self-inflicted trauma (OR, 5.99; 95% CI, 4.16-8.63; P < .001) (doi: 10.1001/jamaophthalmol.2019.3562). The most common types of firearm-related ocular injuries in pediatric patients from 2008-2014 were open wounds of the eyeball (820 [41.6%]) and ocular adnexa (502 [25.5%]), orbital injuries or fractures (591 [30.0%]), and contusion of the eye or adnexa (417 [21.1%]). The inpatient mortality of pediatric patients being treated for firearm-related ocular trauma was 12.2%4.
Management
Diagnosis
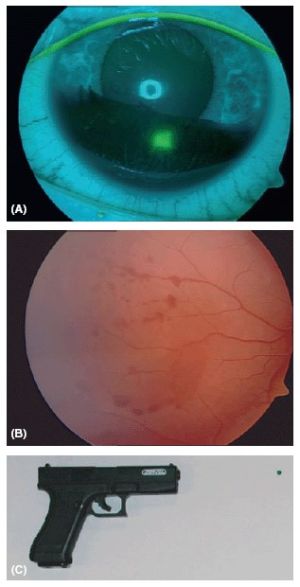
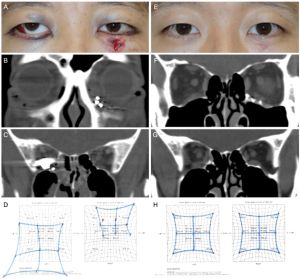
For open globe injuries in pediatric and adult patients, initial evaluation of the patient should consist of a complete history and assessment of visual acuity, afferent pupillary defect, confrontational visual fields, and degree of ocular motility. Slit-lamp examination of ocular anatomy should also be performed. Should the examination suggest an open globe injury, a rigid eye shield should immediately be placed over the injured eye. If the presence of an intraocular foreign body (IOFB) is suspected, a CT scan is indicated, as CT is the most sensitive imaging modality for the detection of metallic IOFBs10,11. Orbital injuries and fractures are approached similarly, with a thorough history and physical examination followed by diagnostic imaging, preferably CT12,13.
Medical therapy
Management of firearm ocular injuries involves a combination of medical and surgical interventions, with the specific treatment plan depending on the type and severity of the injury. In the case of open globe injuries, prophylaxis against endophthalmitis should be initiated with broad-spectrum intravenous antibiotics. In pediatric patients, cefazolin can be used as the first-line drug for open globe injuries without IOFB, whereas a course of intravenous or intravitreal vancomycin and ceftazidime should be completed when an IOFB is present. If the risk of infection is significant, or surgical intervention must be delayed, IV vancomycin and ceftazidime are indicated, with a possible transition to oral ciprofloxacin or moxifloxacin after 1-2 days for a total of 7 days of antibiotic therapy10,14. In adults, IV vancomycin and ceftazidime is recommended for at least 48 hours11. Antifungal prophylaxis is not recommended in children or adults if there is lack of evidence supporting a fungal infection. Tetanus prophylaxis may be appropriate based on the patient’s tetanus immunization status and the nature of the injury11,14. Limited data exists for antibiotic prophylaxis in pediatric orbital fractures, and the utility of perioperative antibiotic prophylaxis against orbital cellulitis and orbital abscess in adults is controversial15,16. In adult patients, antibiotic prophylaxis is not recommended for non-operative orbital fractures17.
Due to the severe pain and potential emesis associated with OGIs, high-dose anti-emetics like IV ondansetron should be administered to prevent Valsalva maneuver, thus reducing the risk of intraocular expulsion. Pain control with IV morphine and sedatives may be given as need11.
Patients with firearm ocular injuries may present with other complications of firearm trauma, such as decreased Glasgow Coma Score (GCS) and consequent requirement of intubation. These should be managed by the trauma team as the patient is initially assessed. Although patients are likely initially cared for by emergency and trauma physicians upon presentation, ophthalmology should be consulted for management of firearm ocular injuries, as a 2023 study demonstrated that in patients presenting with orbital fracture, the survival was 92.3% when ophthalmology was consulted versus 43.8% when ophthalmology was not consulted18.
Surgical Management
Due to chemical and thermal trauma in addition to mechanical trauma firearm injuries are more complex than blunt trauma injuries5. Regardless, early intervention of emergent injuries is crucial for achieving good cosmetic and functional results. OGIs should be operated on within 12-24 hours for better visual outcomes and to decrease the likelihood of endophthalmitis11. Preferred management of ruptured globes, including ruptures caused by gunshots, is primary closure to both preserve the globe and prevent further complications. When globe preservation is unlikely, primary evisceration or enucleation is indicated. Primary perforations should be sutured as soon as possible, with later follow-up vitrectomy for retinal detachment or non-resolving vitreous hemorrhage19. Orbital fractures may also require operative treatment, with the specific procedure being employed depending on the type and location of the fracture12,13. Some orbital fractures require emergent surgical intervention, such as orbital floor fractures complicated by extraocular muscle entrapment. Entrapment should be especially suspected in children presenting with orbital fracture, nausea, and vomiting, as this triad has an >80% positive predictive value for entrapment. Operative treatment can be delayed for 7-14 days for non-emergent orbital fractures, and some orbital fractures do not require surgery at all13. Should an operation be indicated in a pediatric patient, the changing craniofacial anatomy must be considered prior to surgery to ensure the best long-term outcome as the child continues to grow12.
Prevention
Preventing firearm ocular injuries is a complex issue that requires addressing multiple risk factors at both the individual and societal levels.
For any individual, ocular injury prevention begins with safe behaviors such as wearing eye protection. Eyewear protection reduces unintentional ocular damage from flying debris or shrapnel. Endorsed by the AAO, eyewear should ideally be made of polycarbonate material with the “ANSI Z87.1” certification for its superior shatter-resistance and clarity improvements, which are found at most hardware stores20.
At a provider level, providers of all specialties must realize their individual responsibility to screen for and counsel for firearm safe storage with patients to prevent unintentional injuries in a household, acts of suicide, or violence against others. A study with parents demonstrated 75.5% of parents are interested in speaking about firearms with their pediatrician21. Another study focusing on veterans’ perceptions reached similar conclusions22. A modeling study predicted up to 32% of firearm-related deaths at home could be prevented by motivating safer storage, thus underscoring the importance of provider counseling for safe storage in preventing firearm morbidity/mortality23.
Prevention can also be achieved via initiatives that range from community/hospital violence prevention programs (CVIP/HVIPs), to community firearm buyback events, to firearm safety courses, to building robust mental health services among marginalized populations. The American Medical Association supports policies and increased research pertaining to furthering firearm safety24. There is still limited data on firearm policy and its effect on reducing injuries and death. Two successful policies supported by significant data are waiting periods and child-access prevention laws, with the latter having the greatest impact on firearm-related incidents25. Other programs including firearm buyback and firearm safety courses have been seen to vary in effectiveness depending on the region in which they are instituted25.
HVIPs provide victims of violence (with or without a firearm involved) access to social services within a hospital encounter to help them cope with their injury, redirect their energy away from retaliation, and focus on healthy reintegration into society through connection to community services. HVIPs are considered effective in violence prevention with the oldest HVIP program demonstrating how patients in a HVIP were 60% less likely to engage in criminal activity than non-HVIP patients26,27.
Complications
Firearm injury can cause widespread damage to the ocular region of the face. As such, medical management includes prophylaxis against endophthalmitis and other infections. In a meta-analysis studying the efficacy of endophthalmitis prophylaxis, it was noted that endophthalmitis occurs in 3.75% of eyes (358 out of 9,542 eyes) treated for traumatic open globe surgeries. While there is no uniform prophylactic agent for endophthalmitis, microbial coverage as a function of spectrum and intraocular bioavailability must be considered28.
Surgical management for traumatic related eye injuries include evisceration and enucleation. Complications can include major discharge, implant exposure, cellulitis, lid edema, pyogenic granuloma formation, conjunctivitis, and subconjunctival cysts. It is important to note that complications were more common in patients who received a hydroxyapatite implant. Infected orbital implants are another notable complication, as infected implants may require additional removal surgery29,30.
Prognosis
Despite optimal treatment, visual prognosis may remain guarded. Many firearm-associated ocular injuries are sight-threatening and associated with traumatic brain injury . The majority of patients survive, though with potential long-term disabilities.
Summary
In conclusion, firearm ocular injuries are a serious public health issue that requires ongoing attention and intervention, especially in pediatric patients. It is important that more evidence-based policy is created and implemented to reduce firearm related ocular trauma. An important aspect of improving policy and treatment is reestablishing a comprehensive eye trauma registry.
References
- Lee LK, Fleegler EW, Goyal MK, et al. Firearm-Related Injuries and Deaths in Children and Youth: Injury Prevention and Harm Reduction [published online ahead of print, 2022 Oct 8]. Pediatrics. 2022;10.1542/peds.2022-060070. doi:10.1542/peds.2022-060070
- Chen A, McGwin G, Justin GA, Woreta FA. The United States Eye Injury Registry: Past and Future Directions. Ophthalmology. 2021;128(5):647-648. doi:10.1016/j.ophtha.2020.11.026
- Truong T, He CH, Poulsen DM, Parsikia A, Mbekeani JN. Firearm-associated ocular injuries: analysis of national trauma data. Arq Bras Oftalmol. 2021;84(1):58-66. doi:10.5935/0004-2749.20210055
- Weiss R, He C, Gise R, Parsikia A, Mbekeani JN. Patterns of Pediatric Firearm-Related Ocular Trauma in the United States. JAMA Ophthalmol. 2019;137(12):1363. doi:10.1001/jamaophthalmol.2019.3562
- Zhang Y, Kang X, Wu Q, Zheng Z, Ying J, Zhang MN. Explosive eye injuries: characteristics, traumatic mechanisms, and prognostic factors for poor visual outcomes. Mil Med Res. 2023;10(1):3. doi:10.1186/s40779-022-00438-4
- Saunte JP, Saunte ME. 33 cases of airsoft gun pellet ocular injuries in Copenhagen, Denmark, 1998-2002. Acta Ophthalmol Scand. 2006;84(6):755-758. doi:10.1111/j.1600-0420.2006.00734.x
- Kar IB, Kar R, Mishra N, Singh AK. An eye for a lost eye: A case of self-inflicting gunshot injury. Natl J Maxillofac Surg. 2014;5(1):74-78. doi:10.4103/0975-5950.140184
- Moon Y, Seo JW, Kang S, Sa HS. Clinical Characteristics of Intraorbital Foreign Bodies: Our Experience with 14 Cases. J Korean Ophthalmol Soc. 2017;58(3):251-258. doi:10.3341/jkos.2017.58.3.251
- Sharma LCR, Jose MA. Gunshot Injuries of the Maxillofacial Region. In: Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A, eds. Oral and Maxillofacial Surgery for the Clinician. Springer Nature Singapore; 2021:1267-1281. doi:10.1007/978-981-15-1346-6_59
- Li X, Zarbin MA, Bhagat N. Pediatric open globe injury: A review of the literature. J Emerg Trauma Shock. 2015;8(4):216-223. doi:10.4103/0974-2700.166663
- Zhou Y, DiSclafani M, Jeang L, Shah AA. Open Globe Injuries: Review of Evaluation, Management, and Surgical Pearls. Clin Ophthalmol. 2022;16:2545-2559. Published 2022 Aug 10. doi:10.2147/OPTH.S372011
- Oppenheimer AJ, Monson LA, Buchman SR. Pediatric orbital fractures. Craniomaxillofacial Trauma Reconstr. 2013;6(1):9-20. doi:10.1055/s-0032-1332213
- Roth FS, Koshy JC, Goldberg JS, Soparkar CNS. Pearls of orbital trauma management. Semin Plast Surg. 2010;24(4):398-410. doi:10.1055/s-0030-1269769
- Director Infection Management and Prevention service, Immunology and Rheumatology. Acute Management of Open Globe Injuries. 2022.
- Zix J, Schaller B, Iizuka T, Lieger O. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomised, double-blind, placebo-controlled pilot clinical study. Part 1: orbital fractures in 62 patients. Br J Oral Maxillofac Surg. 2013;51(4):332-336. doi:10.1016/j.bjoms.2012.08.008
- Reiss B, Rajjoub L, Mansour T, Chen T, Mumtaz A. Antibiotic Prophylaxis in Orbital Fractures. Open Ophthalmol J. 2017;11:11-16. doi:10.2174/1874364101711010011
- Esce AR, Chavarri VM, Joshi AB, Meiklejohn DA. Evaluation of Antibiotic Prophylaxis for Acute Nonoperative Orbital Fractures. Ophthal Plast Reconstr Surg. 2021;37(5):462-464. doi:10.1097/IOP.0000000000001915
- De Niear MA, Tang VD, Nguyen M, Lin LK. Utilization of Ophthalmic Management in Patients with Head-and-Neck Trauma Secondary to Firearms. J Emerg Trauma Shock. 2023;16(2):43-47. doi:10.4103/jets.jets_165_21
- Ben Simon GJ, Moisseiev J, Rosen N, Alhalel A. Gunshot Wound to the Eye and Orbit: A Descriptive Case Series and Literature Review. J Trauma Inj Infect Crit Care. 2011;71(3):771-778. doi:10.1097/TA.0b013e3182255315
- Turbert D. Safety Glasses and Protective Eyewear Prevent Potentially Blinding Eye Injuries. American Academy of Ophthalmology. 2023.
- Silver AH, Curley M, Azzarone G, Dodson N, O'Connor K. A Parent Survey Assessing Association of Exposure to Gun Violence, Beliefs, and Physician Counseling. Hosp Pediatr. 2022;12(3):e95-e111. doi:10.1542/hpeds.2021-006050
- Aunon FM, Azrael D, Simonetti JA, Miller M. Beliefs Among Veteran Firearm Owners Regarding Whether Clinicians Should Discuss Firearm Safety With Patients. JAMA Netw Open. 2023;6(6):e2321219. Published 2023 Jun 1. doi:10.1001/jamanetworkopen.2023.21219
- Monuteaux MC, Azrael D, Miller M. Association of Increased Safe Household Firearm Storage With Firearm Suicide and Unintentional Death Among US Youths [published correction appears in JAMA Pediatr. 2019 Jul 1;173(7):704]. JAMA Pediatr. 2019;173(7):657-662. doi:10.1001/jamapediatrics.2019.1078
- American Medical Association. Firearm Safety and Research, Reduction in Firearm Violence, and Enhancing Access to Mental Health Care H-145.975. American Medical Association. 2023.
- McCracken H. Understanding Firearm Deaths by State—and How to Reduce Them. RAND Corporation
- Warden K. Hospital-Based Intervention Programs Reduce Violence and Save Money. Center for American Progress. 2022.
- Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma. 2006;61(3):534-540. doi:10.1097/01.ta.0000236576.81860.8c
- Van Swol JM, Myers WK, Beall JA, Atteya MM, Blice JP. Post-traumatic endophthalmitis prophylaxis: a systematic review and meta-analysis. J Ophthalmic Inflamm Infect. 2022;12(1):39. Published 2022 Nov 18. doi:10.1186/s12348-022-00317-y
- Jordan DR. Enucleation and evisceration surgery complications. American Academy of Ophthalmology.
- Kord Valeshabad A, Naseripour M, Asghari R, et al. Enucleation and evisceration: indications, complications and clinicopathological correlations. Int J Ophthalmol. 2014;7(4):677-680. doi:10.3980/j.issn.2222-3959.2014.04.17

